Research - (2022) Volume 10, Issue 2
A Study on Surgical Site Infections with Special Reference to Methicillin Resistant Staphylococcus aureus in a Tertiary Care Hospital
*Correspondence: M Nishanthy, Department of Microbiology, Sree Balaji Medical College and Hospital, India, Email:
Abstract
Surgical site infections are one of the most important causes of health care associated infections in surgical patients. Prevalence of surgical site infections varies between 5%-24% in India. Staphylococcus aureus is one of the most important organisms causing surgical site infections. Treatment of MRSA infections are challenging, because of the restricted availability of antimicrobials of proven efficacy. In this study a total of 242 pus Samples were received over a periodfrom January 2018 to December 2018,212(87.6%) samples were culture positive showing growth of aerobic bacteria , among these 212positive samples, males were 141 and females were71.The most Common organism isolated was Staphylococcus aureus with 75(35.3%) isolates ,of these75 Staphylococcus aureus isolates, 21 (28.0%)isolates were methicillin resistant Staphylococcus aureus. In antibiotic susceptibility patterns, MRSA isolates were highly susceptible to linezolid, clindamycin, gentamicin, chloramphenicol tetracycline and highly resistant to penicillin, cefoxitin, erythromycin, cotrimoxazole, ciprofloxacin, tetracycline, gentamicin, chloramphenicol.
Keywords
Methicillin resistant Staphylococcus aureus, Surgical site infection, Resistance, Prevalence, Staphylococcus aureus
Introduction
Surgical site infections are one of the most important causes of health care associated infections in surgical patients. It is defined as infection occurring in the surgical site within 30 days after surgical procedure affecting either incision or deep tissues at the operation site [1]. Those patients who are likely to develop surgical site infections are those whose hospital stays are longer, with more expensive hospitalizations, associated with increased mortality [2]. Based on several studies prevalence of surgical site infections vary between 5%-24% in India [3]. Surgical site infections are caused by organisms than can be exogenous or endogenous microorganisms that can enter the operative wound at the time of surgery [4]. Breach in the integrity and protective functions of the skin paves way for the development for surgical site infections [5].There are several factors which influence infected surgical wounds such as type of surgery, and pre and post-operative care which is provided. Staphylococcus aureus is one of the most important organisms causing surgical site infections .MRSA was most common pathogen in patients who underwent cardiac, vascular and orthopaedic surgeries. Treatment of MRSA infections are challenging, because of the restricted availability of antimicrobials of proven efficacy [6]. Hence the objective of this study was to find out the prevalence forms among SSI’s and also its antimicrobial susceptibility pattern.
Materials and Methods
The study was conducted in the department of microbiology at Sree Balaji Medical College and hospital from Jan 2019 to December 2019.During the study period a total of 1380 surgeries were conducted and a total of 242 defined cases of surgical site infections as per CDC guidelines from surgical ward, orthopaedic ward, obstetrics and gynaecology ward were enrolled in the study.
Inclusion criteria
All patients having history of any operation with surgical wound occurring within 30 days after surgery having pus or serous discharge or seropurulent discharge without signs of sepsis were considered as surgical site infections.
Exclusion criteria
Patients with cellulitis and without discharge are excluded from study.
Methods
Pus samples were collected under strict aseptic precautions and transported immediately to the central laboratory. In the microbiology laboratory all samples were immediately processed as per CLSI guidelines. All these pus samples were routinely subjected to Gram stain and culture on nutrient agar, blood agar, Mac-conkey agar and incubated at 37 deg C for 18-24 hrs. and a battery of biochemical test was done to confirm Staphylococcus aureus isolates.
Confirmatory disc diffusion testing for MRSA
The broth culture is prepared in peptone water and incubated at 35 ˚C for 2-6 hrs. until achieving turbidity of 0.5 McFarland standards. Mueller-Hinton agar plates are supplemented with 4% sodium chloride as per the NCCLS recommendation was inoculated with test strains and the ATCC strain 25923 as lawn culture in separate plates used as screening test for MRSA. Cefoxitin (30 mcg) antibiotic disc was placed in appropriate positions and then incubated for 18-24 hrs. The zone of inhibition around the cefoxitin disc was measured as either less than 21mm (MRSA) or more than 22mm (MSSA).Isolated Staphylococcus aureus was tested for antibiotic sensitivity testing by Kirby-Bauer disc diffusion method on Muller Hinton Agar with commercially available himedia discs such as penicillin(10units),gentamicin(10mcg), erythromycin(15 mcg),tetracycline(30mcg),ciprofloxacin(5mcg),clindamyc in(2mcg),trimethoprim/sulphamthoxazole(1.25/3.75mcg), chloramphenicol(30 mcg),linezolid(30 mcg).Methicillin resistance Staphylococcus aureus was determined by disc diffusion method using cefoxitin (30 mcg) discs and results were interpreted as per CLSI guidelines. S. aureus ATCC 25923, S. aureus ATCC 43300 was used as control strains.
Results
Out of 242 pus Samples received,212(87.6%) samples were culture positive showing growth of aerobic bacteria ,among these 212positive samples, males were 141 and females were71.The most Common organism isolated was Staphylococcus aureus with 75(35.3%) isolates ,of these75 Staphylococcus aureus isolates, 21 (28.0%)isolates were methicillin resistant Staphylococcus aureus (Figures 1 and Figure 2), (Table 1).
Figure 1. Male and female ratio.
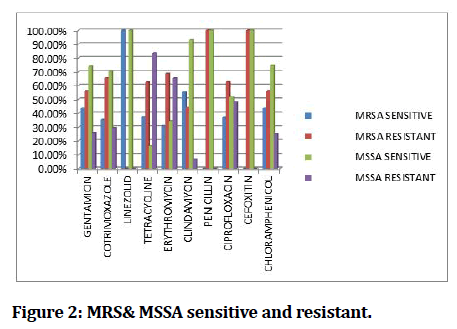
Figure 2. MRS& MSSA sensitive and resistant.
| Drugs | Mrsa ( n=21 ) (28%) | MSSA ( n=54 ) (72%) | ||
|---|---|---|---|---|
| Sensitive | Resistant | Sensitive | Resistant | |
| Gentamicin | 43.70% | 56.30% | 74.00% | 26% |
| Cotrimoxazole | 35.50% | 65.50% | 70.30% | 29.70% |
| Linezolid | 100% | 0 | 100% | 0 |
| Tetracycline | 37.50% | 62.50% | 16.30% | 83.70% |
| Erythromycin | 31.10% | 68.90% | 34.50% | 65.50% |
| Clindamycin | 55.50% | 44.50% | 93.10% | 6.90% |
| Penicillin | 0 | 100% | 100% | 0 |
| Ciprofloxacin | 37.30% | 62.70% | 51.80% | 48.20% |
| Cefoxitin | 0 | 100% | 100% | 0 |
| Chloramphenicol | 43.70% | 56.30% | 74.50% | 25.50% |
Table 1: Comparison of antibiotic susceptibility pattern between MRSA and MSSA producers.
Discussion
Detection of methicillin resistant Staphylococcus aureus is by detection of Mec-a gene, but all laboratories will not include molecular techniques in their routine practice. Hence it is essential for phenotypic isolates for detection of MRSA isolates in a rapid and accurate manner, to ensure accurate treatment with antibiotics and avoiding spread of MRSA isolates. Cefoxitin does not require any special incubation temperature and any special medium. Hence in this study cefoxitin was used for testing MRSA isolates .Detection of Mec-a positive isolates with cefoxitin disc in predicting oxacillin resistance has been reported [7].In our study a total of 242 pus samples which were collected from surgical site infections ,higher incidence was seen in surgery cases(36.8%), orthopaedic cases(22.6%),/obstetrics-gynaecology cases(22.6%),other department cases around (18.0%) respectively. Also the surgical site infections are more common in male patients compared to female patients. Staphylococcus aureus was most common pathogen isolated around 75 isolates with (35.3%).In antibiotic susceptibility patterns, MRSA isolates were highly susceptible to linezolid, clindamycin, gentamicin, chloramphenicol, tetracycline and highly resistant to penicillin, cefoxitin, erythromycin, cotrimoxazole, ciprofloxacin,tetracycline,gentamicin,chloramphenicol. Staphylococcus aureus is one of the notorious organism to acquire resistance even to penicillinase stable penicillin like oxacillin and cefoxitin [8]. The prevalence of surgical site infections in our study is 17.5% and the prevalence of methicillin resistant Staphylococcus aureus in our study was 28.0%.We found that all MRSA strains are highly susceptible to linezolid, which is of relevant clinical use for following antibiotic policy in hospitals .MRSA contributes around 5.1% of surgical site infections according to Harbarth et al. [9]. Hence proper infection control practices, effective hand washing to prevent carrier transmission and active surveillance of SSIs, with effective training to health care workers can curtail the spread of MRSA.
Conclusion
Early detection and appropriate intervention of cases of surgical site infections is determining factor to reduce incidence of morbidity and mortality. However complete elimination is not possible but still significant reduction in infections will cause dramatic benefits. Adequate drug concentration delivery to the site of infection is necessary; hence a proper antibiotic policy should be formulated in every hospital to curtail the spread of MRSA transmission. Also every health care personnel and staff should be screened for nasal carriers of MRSA to prevent transmission to patients, thereby reducing significant morbidity and mortality.
References
- Mangram AJ, Horan TC, Pearson ML, et al. Guidelines for Prevention of SSI, 1999, Criteria for defining SSIs. The hospital infection control practices advisory committee. Infect Control Hosp Epidemiol 1999; 20.
- Kirkland KB, Briggs JP, Trivette SL, et al. The impact of surgical-site infections in the 1990s: attributable mortality, excess length of hospitalization, and extra costs. Infect Control Hosp Epidemiol 1999; 20:725-730.
- Pathak A, Saliba EA, Sharma S, et al. Incidence and factors associated with surgical site infections in a teaching hospital in Ujjain, India. Am J Infect Control 2014; 42:e11-5.
- Nichols RL. Current Strategies for prevention of surgical site infections. Curr Infect Dis Rep 2004; 6:426-34.
- Calvin Cutaneous wound repair. Wounds 1998; 10:12-32.
- Ranjan KP, Ranjan N, Gandhi S. Surgical site infections with special reference to methicillin resistant Staphylococcus aureus: Experience from a tertiary care referral hospital in North India. Int J Res Med Sci 2013; 1:108-111.
- Skov R, Smyth R, Clausen M, et al. Evaluation of cefoxitin 30 mcg disc on iso-sensitest agar for detection of methicillin resistant Staphylococcus aureus. J Antimicrob Chemother 2003; 52:204-7.
- Batabyal B, Biswas S, Kundu GK, et al. A study on surgical site infections caused by Staphylococcus aureus with a special search for methicillin-resistant isolates in oral & maxillofacial infections. Asian J Pharm Life Sci 2011; 5:502-508.
- Harbarth S, Fankhauser C, Schrenzel J, et al. Universal screening for methicillin-resistant Staphylococcus aureus at hospital admission and nosocomial infection in surgical patients. JAMA 2008; 299:1149-1157.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Department of Microbiology, Sree Balaji Medical College and Hospital, Chromepet, Chennai, IndiaReceived: 03-Feb-2022, Manuscript No. JRMDS-22-53372; , Pre QC No. JRMDS-22-53372 (PQ); Editor assigned: 04-Feb-2022, Pre QC No. JRMDS-22-53372 (PQ); Reviewed: 18-Feb-2022, QC No. JRMDS-22-53372; Revised: 21-Feb-2022, Manuscript No. JRMDS-22-53372 (R); Published: 28-Feb-2022
