Research - (2022) Volume 10, Issue 2
Bonding Protocol for all Ceramic Restorations-A Proposal for a Clinical Decision Tree
Amrutha Shenoy, Vinay Sivaswamy and Subhabrata Maiti*
*Correspondence: Subhabrata Maiti, Department of Prosthodontics and Implantology, Saveetha Institute Of Medical And Technical Sciences Saveetha University, India, Email:
Abstract
Statement of problem: With an increasing number of all ceramic materials available for clinical use, an overview of the scientific literature on the adhesion methods for different all ceramic materials and their potential influence is indicated. Aim: This study proposed the development of a protocol for bonding of all ceramic prostheses using various adhesives/cements for the improvement of the longevity of restorations. Materials and methods: A decision tree protocol was developed with criteria (i) Type of all ceramic material: Alumina, lithium disilicate and zirconia. (ii) Type of surface treatment, if any required (iii) Type of adhesive/cement/ luting agent used for long term success. (iv) Survival rates and complication rates seen with different bonding protocols. A decision tree protocol was set up with the current available literature. Results: According to the literature, multiple all-ceramic materials and systems are currently available for clinical use, and there is no single universal material or system that can be used in all clinical situations. The successful application is dependent upon the clinician to match the materials, manufacturing techniques, and cementation or bonding procedures, with the individual clinical situation. Conclusion: There are various methods that can be used for treatment of ceramic bonding. Further continued investigations will be needed for the appropriate protocol updates.
Keywords
Ceramic surface treatment, Zirconia, Lithium disilicate, Ceram alumina, Self-adhesive cements
Introduction
Following the introduction of the first Feld spathic porcelain crown by Land [1], the interest and demand for non-metallic and biocompatible restorative materials increased for dentists and patients. Recently, all-ceramic restorations have become popular, mainly because of esthetics and good mechanical properties. Bonding is one the most important factors that influences the long term success of any of these all ceramic crowns. Various surface treatment protocols have been described previously due to lack of susceptibility to etching and this makes it impossible to realize the adhesive procedures. Realizing safe and standardized adhesive cementation protocols of these crowns is necessary in order to adequately complete the conservative/prosthetic treatment plan, especially when it is necessary to improve the mechanical characteristics of the tooth-prosthesis complex.
Resin bonding has been advised for low and moderate strength ceramics that are not supported by a core, especially if the preparation is minimally invasive or is lacking retention form, thus bonding of lithium disilicate and zirconia complete-coverage restorations has always been a controversial topic [1-4]. Most of the existing knowledge in this regard is based on in vitro studies that have shown that adhesive resin cementation increased the retention of lithium disilicate crowns [5], improved the fracture strength and reduced the marginal leakage of alumina crowns [6], improved the fracture resistance of lithium disilicate crowns [7], and increased the fatigue resistance of zirconia crowns [8]. In contrast, another study showed that the retention of zirconia crowns did not differ between a resin- modified glass Ionomer cement and resin cements [9]. Also, other studies reported no difference in the fracture resistance of zirconia fixed partial dentures and crowns [9-12], retention of zirconia crowns [13], and fracture resistance of pressed or milled lithium disilicate crowns after adhesive or conventional cementation [14,15]. Two clinical studies based on the same cohorts of participants compared the failure rates and complications of short-span lithium disilicate fixed partial dentures when conventional or adhesive cementation was used and reported no difference after 8 and 10 years.
Given the increase in popularity of all-ceramic restorations/ prostheses mainly, lithium disilicate and zirconia restorations, a review and synthesis of current data related to the clinical outcomes of these restoration materials when treated using different surface treatment protocols and cemented with resin cements as opposed to conventional cements is necessary. The purpose of this study was to analyse clinical performance of toothsupported all ceramic crowns and to describe the complications/failure characteristics when different surface treatment protocols were used and when adhesive or conventional cementation is used to better guide the practitioner with a clinical workflow that can be used in daily practice.
Objectives
The aim of this paper was to present a detailed workflow for restoration with different all ceramic materials, focused on different adhesives/ cements, various surface treatments if needed and overall survival and complications through a systematic decision tree.
Glass ceramics
The most appropriate are luting composites [16,17] which not only provide the strongest bond but can increase the fracture resistance of the restored tooth and indirect ceramic restoration as well [16,18-20]. However, surface treatment is necessary to ensure a long term bond between ceramic material and the tooth structure. The mechanical alteration can be achieved by surface acid etching, airborne particle abrasion or grinding with diamond rotary instruments [21-23]. The chemical treatment is performed using universal or ceramic primers, i.e. salinization [24,25], while the method used for chemo-mechanical alteration of the bonding surface is tribochemical silica-coating, i.e. silicatization [26,27]. Numerous alternative treatments are proposed for treatment of restorations made up from zirconia such as: selective infiltration etching (SIE) [28,29] followed by application of various silane-based zirconia primers [30,31], gas - phase chloro-silane pre-treatment [32], gas - plasma, argon - ion bombardment, alumina or zirconia sandblasting [33], non - thermal plasma treatment [33,34], nano -structure alumina coating [35] or aluminium nitride coating by reactive magnetron sputtering [36].
Which surface conditioning method will be selected depends on the chemical composition of the ceramic restoration [36-38]. Ceramics, the matrix of which is based on silicon dioxide ("conventional" or glassceramics) belong to the group in which acid etching is the recommended surface treatment [38]. These include feldspar-based, leucite-reinforced, lithium disilicate [38] and zirconia-reinforced lithium silicate ceramics [38] as well as fluorapatite ceramics. Airborne particle abrasion (sandblasting) can be used for surface treatment of all types of ceramics [21,23]. Universal or ceramic primers having reactive radicals in their molecules change the chemical composition of the ceramic surface, thus making it much more reactive for binding with composite cement [21,38]. Tribochemical silica - coating is primarily used for the treatment of aluminium trioxide and zirconium dioxide ceramics; acid etching will not have any impact on their surface morphology, as these materials don’t contain silicon in their composition [23].
Lithium disilicate ceramics
Surface treatment
According to Kim et al. the effect of the surface treatment primarily depends on the chemical composition of the ceramic. Hydrofluoric acid etching is the most appropriate treatment of a lithium disilicate ceramic. Exposure of crystals is observed after etching of the lithium disilicate ceramic. It may be noted that all glassy ceramics have almost identical content of silicon dioxideabout 60%, while the presence of aluminium oxide is similar between feldspar-based and leucite- reinforced ceramics - about 20%, and between lithium disilicate and zirconia-reinforced lithium silicate - about 4%. However, the specific internal structure and presence of other oxides influence the effect of HF acid etching. According to Bajraktarova-Valjakova et al. numerous micropores and channels of different sizes with irregular ceramic particles can be observed on the surface of VITA Mark II; the etching surface of IPS Empress CAD gets honeycomblike appearance, while numerous elongated or bean-like [23,39,40] crystals have been extruded as a result of silica - matrix dissolving after etching of IPS e.max CAD and Celtra Duo respectively. HF etching of VITA Enamic causes dissolving of the superficial ceramic network, so that the acrylic polymer network becomes visible with scattered irregular ceramic particles.
In conclusion, there are various methods that can be used for the treatment of ceramic bonding surfaces when adhesive luting is recommended. Undoubtedly, the most appropriate treatment method for silica-based ceramics is acid etching.
Bonding
In a systematic review by Georgios Maroulakos et al. [41], adhesive resin cementation was reported for 1957 lithium disilicate crowns in 10 of the included articles [41-63]. The range of crown survival rate was 83.5% to 100%, whereas the complication-free rate ranged from 71.0% to 96.7%. Conventional cementation was reported for 163 lithium disilicate crowns in 2 of the included articles [57,64]. Crown survival was reported by one article as 98.5%,57 whereas another article re-ported a 87.1% complication-free rate. Gehrt64 reported 82.0% complication-free rates for adhesively cemented lithium disilicate crowns and 87.1% for conventionally cemented ones (Figure 1) [42].
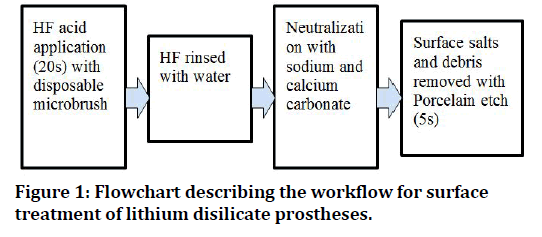
Figure 1. Flowchart describing the workflow for surface treatment of lithium disilicate prostheses.
In ceram glass infiltrated Alumina ceramic
Surface treatment
Bonding to In-Ceram glass infiltrated alumina ceramic requires techniques that are different from techniques that can be used for conventional silica-based dental ceramics. A long-term durable bond to In-Ceram alumina ceramic can be achieved with either the combination of tribochemical silica coating and conventional BIS-GMA composite resin or with the combination of sandblasting and composite resin modified with a phosphate monomer [51]. The bonded surface can be tribochemically silica coated and silanted (Rocatec), followed by etching of enamel for 30s with 36% phosphoric acid.
Bonding
The restoration can then be inserted using phosphate monomer containing luting resin (eg. Panavia) [52].
Zirconia
Surface treatment
Tribochemical silica coating has a positive impact on the bond of luting composite to aluminium oxide and zirconium oxide ceramics [39]. Hydrofluoric acid etching has no effect on the so-called polycrystalline ceramics; such are aluminium trioxide [53,54] and zirconium dioxide partially stabilized with yttrium oxide [55]. Increase in mechanical strength by increasing the number of crystals and reducing the content of glass (silicon dioxide), leads to the creation of acid - resistant ceramics (non-etchable). Treatment with any acid will not induce any satisfactory (micro retentive) changes to the surface micro - morphology to ensure proper bonding of composite cement [56,57-59]. Surface treatment of such ceramic restorations is performed using other methods: tribochemical silica coating [26,29,60], chemical treatment with methacryloyloxydecyl dihydrogen phosphate (MDP) - containing primers [60], or alternative methods. Tribochemical coating seems to be less effective for zirconia ceramics than for glass-infiltrated ceramics [55,61]. Y-TZP ceramics present greater hardness compared with systems with a glassy structure, which prevents the impregnation of silica onto the surface [62]. For this reason, silane agents do not bond adequately to zirconia ceramics [55].
Air abrasion with aluminium oxide particles is routinely performed to remove layers of contaminants, thus increasing micromechanical retention between the resin cement and the restoration [63,64]. Usually, air abrasion units use aluminium oxide particles with sizes ranging from 25 μm to 250 μm. These particles may or may not be silica-coated (tribochemical treatment) [65]. The effect of air abrasion on the mechanical properties of zirconia has been repeatedly discussed in the literature, and both positive and negative results have been described [66,67].
Some authors have stated that air abrasion increases the flexural resistance of zirconia ceramics, because it induces T-M phase transformations, creating compressive layers on the surface [65]. Apparently, the depth of the surface flaws induced by air abrasion do not exceed the thickness of the compressive layers, justifying the improved properties of air-abraded surfaces [65,67]. When the effects of air abrasion and milling with finegrained dia- mond instruments (20 μm -40 μm) were compared with the use of coarse diamond burs (125 μm -150 μm), it was observed that less severe protocols reduced surface roughness and provided the formation of compressive layers on the surface. Conversely, coarse diamond burs reduced the flexural strength and reliability of Y-TZP ceramics [65]. In a different study, air abrasion and coarse diamond burs also presented opposite effects on the flexural resistance of a zirconia ceramic [66]. The authors of that study added that, during milling with the diamond bur, a vast amount of material was removed and sparks were commonly observed despite the use of constant water spray, indicating that both stress and tem- premature were high during the operation.
Other techniques for the superficial treatment of zirconia ceramics have been described; these are plasma spraying and fusing glass pearls to the zirconia surface [66,68]. Both treatments improved the bond strength of resin cements to the surface. Nevertheless, they were not compared with conventional methods of surface treatments for Y-TZP ceramics, such as air abrasion and tribochemical coating [66,68,69].
Bonding
Bonding agents include zinc phosphate cements, conventional and resin-modified glass Ionomer cements, resin cements and self-adhesive resin cements [70]. However, resin cements possess some advantages compared with the other classes of materials, since they have lower solubility and better esthetic characteristics [17,71,72]. In addition, the adhesive bond between the resin cement and ceramic might increase the restoration’s resistance during occlusal loads [1,39,40].
There is some evidence that demonstrates that a better bond to Y-TZP ceramics is obtained using resin cements with phosphate ester monomers, such as the MDP monomer18. The phosphate ester group might chemically bond to metal oxides, such as zirconium dioxide [63,73] Wolfart and others evaluated the durability of the bond with two resin cements (MDPbased and Bis-GMA-based) to a zirconia ceramic. The MDP-based material presented higher bond strength to zirconia surfaces air abraded with alumina particles and this bond survived 150 days of water storage. Other studies also stated that resin cements with phosphate ester groups increase the bond strength of air abraded and tribochemical-coated surfaces (Figure 2 and Figure 3) [55].
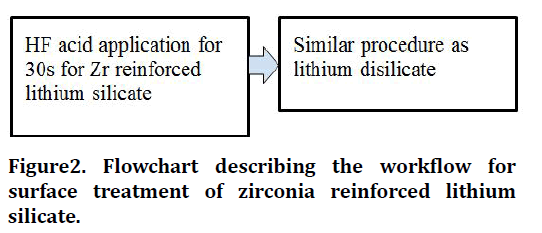
Figure 2. Flowchart describing the workflow for surface treatment of zirconia reinforced lithium silicate.
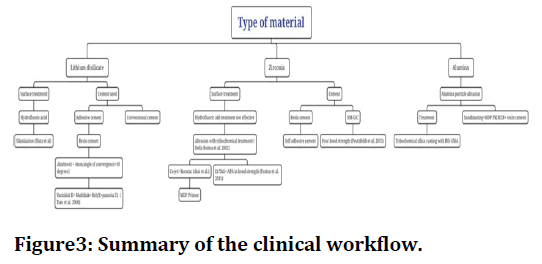
Figure 3. Summary of the clinical workflow.
Conclusion
The role of bonding efficacy plays a major role in the survival of any all-ceramic prosthesis. There are various methods that can be used for treatment of ceramic bonding. Based on the available evidence and within the limitations of this review, following conclusions were drawn:
• To bond zirconia, airborne particle abrasion with 50 micron aluminum oxide at 0.10-0.25MPa in combination with a MDP primer containing adhesive resin is recommended, following rubber dam isolation.
• Acid etching is the most appropriate treatment method for silica-based ceramics.
• Tribochemical silica coating and conventional BISGMA resin or combination of sandblasting and MDP containing resin appeared suitable for bonding of in Ceram alumina.
References
- Land CH. Porcelain Literature. 1903.
- Blatz MB, Vonderheide M, Conejo J. The effect of resin bonding on long-term success of high-strength ceramics. J Dent Res 2018; 97:132-139.
- Christensen GJ. Use of luting or bonding with lithium disilicate and zirconia crowns. J Am Dent Assoc 2014; 145:383-386.
- Mizrahi B. The anterior all-ceramic crown: A rationale for the choice of ceramic and cement. Br Dent J 2008; 205:251-255.
- Johnson GH, Lepe X, Patterson A, et al. Simplified cementation of lithium disilicate crowns: Retention with various adhesive resin cement combinations. J Prosthet Dent 2018; 119:826-32.
- Blatz MB, Oppes S, Chiche G, et al. Influence of cementation technique on fracture strength and leakage of alumina all-ceramic crowns after cyclic loading. Quintessence Int 2008; 39.
- de Kok P, Pereira GK, Fraga S, et al. The effect of internal roughness and bonding on the fracture resistance and structural reliability of lithium disilicate ceramic. Dent Mater 2017; 33:1416-25.
- Campos F, Valandro LF, Feitosa SA, et al. Adhesive cementation promotes higher fatigue resistance to zirconia crowns. Oper Dent 2017; 42:215-24.
- Ehlers V, Kampf G, Stender E, et al. Effect of thermocycling with or without 1 year of water storage on retentive strengths of luting cements for zirconia crowns. J Prosthet Dent 2015; 113:609-15.
- Rosentritt M, Hmaidouch R, Behr M, et al. Fracture resistance of zirconia FPDs with adhesive bonding versus conventional cementation. Int J Prosthodont 2011 ;24.
- Zesewitz TF, Knauber AW, Nothdurft FP. Fracture resistance of a selection of full-contour all-ceramic crowns: An in vitro study. Int J Prosthodont 2014; 27:264-266.
- Nakamura K, Mouhat M, Nergård JM, et al. Effect of cements on fracture resistance of monolithic zirconia crowns. Acta Biomater Odontol Scand 2016;2:12-9.
- Ernst CP, Aksoy E, Stender E, et al. Influence of different luting concepts on long term retentive strength of zirconia crowns. Am J Dent 2009; 22:122-128.
- Heintze SD, Cavalleri A, Zellweger G, et al. Fracture frequency of all-ceramic crowns during dynamic loading in a chewing simulator using different loading and luting protocols. Dent Mater 2008; 24:1352-1361.
- Preuss A, Rosentritt M, Frankenberger R, et al. Influence of type of luting cement used with all-ceramic crowns on load capability of post-restored endodontically treated maxillary central incisors. Clin Oral Investig 2008; 12:151-156.
- Chen L, Suh BI. Bonding of resin materials to all-ceramics: a review. Curr Res Dent 2012; 3:7-17.
- Krämer N, Lohbauer U, Frankenberger R. Adhesive luting of indirect restorations. Am J Dent 2000; 13:60D-76D.
- Blatz MB, Sadan A, Kern M. Resin-ceramic bonding: A review of the literature. J Prosthet Dent 2003; 89:268-74.
- Vargas MA, Bergeron C, Diaz-Arnold A. Cementing all-ceramic restorations: recommendations for success. J Am Dent Assoc 2011; 142:20S-4S.
- Burke FJ, Fleming GJ, Nathanson D, et al. Are adhesive technologies needed to support ceramics? An assessment of the current evidence. J Adhes Dent 2002; 4.
- Ho GW, Matinlinna JP. Insights on ceramics as dental materials. Part II: Chemical surface treatments. Silicon 2011; 3:117-23.
- El-Meliegy E, Van Noort R. Glasses and glass ceramics for medical applications. Springer Sci Busin Media 2011.
- Borges GA, Sophr AM, De Goes MF, et al. Effect of etching and airborne particle abrasion on the microstructure of different dental ceramics. J Prosthet Dent 2003; 89:479-88.
- Matinlinna JP, Lassila LV, Özcan M, et al. An introduction to silanes and their clinical applications in dentistry. Int J Prosthodont 2004; 17.
- Lung CY, Matinlinna JP. Aspects of silane coupling agents and surface conditioning in dentistry: An overview. Dent Mater 2012; 28:467-77.
- Lung CY, Kukk E, Hägerth T, et al. Surface modification of silica-coated zirconia by chemical treatments. Appl Surf Sci 2010; 257:1228-35.
- Bottino MC, Özcan M, Coelho PG, et al. Micro-morphological changes prior to adhesive bonding: High-alumina and glassy-matrix ceramics. Braz Oral Res 2008; 22:158-63.
- Aboushelib MN, Kleverlaan CJ, Feilzer AJ. Selective infiltration-etching technique for a strong and durable bond of resin cements to zirconia-based materials. J Prosthet Dent 2007; 98:379-88.
- Casucci A, Mazzitelli C, Monticelli F, et al. Morphological analysis of three zirconium oxide ceramics: Effect of surface treatments. Dent Mater 2010; 26:751-60.
- Aboushelib MN, Matinlinna JP, Salameh Z, et al. Innovations in bonding to zirconia-based materials: Part I. Dental Materials 2008; 24:1268-72.
- Aboushelib MN, Feilzer AJ, Kleverlaan CJ. Bonding to zirconia using a new surface treatment. J Prosthodont 2010; 19:340-6.
- Piascik JR, Swift EJ, Thompson JY, et al. Surface modification for enhanced silanation of zirconia ceramics. Dent Mater 2009; 25:1116-21.
- Hallmann L, Ulmer P, Wille S, et al. Effect of surface treatments on the properties and morphological change of dental zirconia. J Prosthet Dent 2016; 115:341-9.
- Valverde GB, Coelho PG, Janal MN, et al. Surface characterisation and bonding of Y-TZP following non-thermal plasma treatment. J Dent. 2013; 41:51-9.
- Jevnikar P, Krnel K, Kocjan A, et al. The effect of nano-structured alumina coating on resin-bond strength to zirconia ceramics. Dent Mater 2010; 26:688-96.
- Külünk T, Külünk Ş, Baba S, et al. The effect of alumina and aluminium nitride coating by reactive magnetron sputtering on the resin bond strength to zirconia core. J Adv Prosthodont 2013; 5:382-7.
- Özcan M, Vallittu PK. Effect of surface conditioning methods on the bond strength of luting cement to ceramics. Dent Mater 2003; 19:725-31.
- Peumans M, Valjakova EB, De Munck J, et al. Bonding effectiveness of luting composites to different CAD/CAM materials. J Adhes Dent 2016; 18:289-302.
- Kim BK, Bae HE, Shim JS, et al. The influence of ceramic surface treatments on the tensile bond strength of composite resin to all-ceramic coping materials. J Prosthet Dent 2005; 94:357-62.
- Borges GA, Spohr AM, Oliveira WJ, et al. Effect of refrigeration on bond strength of self-etching adhesive systems. Braz Dent J 2006; 17:186-90.
- Maroulakos G, Thompson GA, Kontogiorgos ED. Effect of cement type on the clinical performance and complications of zirconia and lithium disilicate tooth-supported crowns: A systematic review. Report of the Committee on Research in Fixed Prosthodontics of the American Academy of Fixed Prosthodontics. J Prosthet Dent 2019; 121:754-65.
- Rauch A, Reich S, Dalchau L, et al. Clinical survival of chair-side generated monolithic lithium disilicate crowns: 10-year results. Clin Oral Investig 2018; 22:1763-9.
- Schmitz JH, Beani M. Effect of different cement types on monolithic lithium disilicate complete crowns with feather-edge preparation design in the posterior region. J Prosthet Dent 2016 ; 115:678-83.
- Huettig F, Gehrke UP. Early complications and performance of 327 heat-pressed lithium disilicate crowns up to five years. J Adv Prosthodont 2016; 8:194-200.
- Seydler B, Schmitter M. Clinical performance of two different CAD/CAM-fabricated ceramic crowns: 2-Year results. J Prosthet Dent 2015; 114:212-6.
- Simeone P, Gracis S. Eleven-year retrospective survival study of 275 veneered lithium disilicate single crowns. Int J Periodontics Restorative Dent 2015; 35:685–694.
- Toman M, Toksavul S. Clinical evaluation of 121 lithium disilicate all-ceramic crowns up to 9 years. Quintessence Int 2015;46.
- Fabbri G, Zarone F, Dellificorelli G, et al. Clinical evaluation of 860 anterior and posterior lithium disilicate restorations: retrospective study with a mean follow-up of 3 years and a maximum observational period of 6 years. Int J Periodont Restorative Dent 2014; 34.
- Esquivel‐Upshaw J, Rose W, Oliveira E, et al. Randomized, controlled clinical trial of bilayer ceramic and metal‐ceramic crown performance. J Prosthodont 2013; 22:166-73.
- Gehrt M, Wolfart S, Rafai N, et al. Clinical results of lithium-disilicate crowns after up to 9 years of service. Clin Oral Investig 2013; 17:275-84.
- Kern M, Thompson VP. Bonding to glass infiltrated alumina ceramic: adhesive methods and their durability. J Prosthet Dent 1995; 73:240-9.
- Sasse M, Kern M, Marré B, et al. Clinical performance of cantilevered fixed dental prostheses abutments in the shortened dental arch. J Dent 2014; 42:373-6.
- Lu YC, Tseng H, Shih YH, et al. Effects of surface treatments on bond strength of glass‐infiltrated ceramic. J Oral Rehabil 2001; 28:805-13.
- Özcan M, Alkumru HN, Gemalmaz D. The effect of surface treatment on the shear bond strength of luting cement to a glass-infiltrated alumina ceramic. Int J Prosthodont 2001; 14.
- Kern M, Wegner SM. Bonding to zirconia ceramic: Adhesion methods and their durability. Dent Mater 1998; 14:64-71.
- Dérand P, Derand T. Bond strength of luting cements to zirconium oxide ceramics. Int J Prosthodont 2000; 13.
- Bona AD, Anusavice KJ, Shen C. Microtensile strength of composite bonded to hot-pressed ceramics. J Adhes Dent 2000;2.
- Madani M, Chu FC, McDonald AV, et al. Effects of surface treatments on shear bond strengths between a resin cement and an alumina core. J Prosthet Dent 2000; 83:644-7.
- Bona AD, Anusavice KJ, Hood JA. Effect of ceramic surface treatment on tensile bond strength to a resin cement. Int J Prosthodont 2002;15.
- Inokoshi M, Kameyama A, De Munck J, et al. Durable bonding to mechanically and/or chemically pre-treated dental zirconia. J Dent 2013; 41:170-9.
- Ernst CP, Cohnen U, Stender E, et al. In vitro retentive strength of zirconium oxide ceramic crowns using different luting agents. J Prost Dent 2005; 93:551-8.
- Matinlinna JP, Heikkinen T, Özcan M, et al. Evaluation of resin adhesion to zirconia ceramic using some organosilanes. Dent Mater 2006;22:824-31.
- Wolfart M, Lehmann F, Wolfart S, et al. Durability of the resin bond strength to zirconia ceramic after using different surface conditioning methods. Dent Mater 2007; 23:45-50.
- Valandro LF, ÖZCAN M, Amaral R, et al. Effect of testing methods on the bond strength of resin to zirconia-alumina ceramic: Microtensile versus shear test. Dent Mater J 2008; 27:849-55.
- Curtis AR, Wright AJ, Fleming GJ. The influence of surface modification techniques on the performance of a Y-TZP dental ceramic. J Dent 2006; 34:195-206.
- Kosmač T, Oblak C, Jevnikar P, et al. The effect of surface grinding and sandblasting on flexural strength and reliability of Y-TZP zirconia ceramic. Dent Mater. 1999; 15:426-33.
- Papanagiotou HP, Morgano SM, Giordano RA, et al. In vitro evaluation of low-temperature aging effects and finishing procedures on the flexural strength and structural stability of Y-TZP dental ceramics. J Prosthet Dent 2006; 96:154-64.
- Derand T, Molin M, Kvam K. Bond strength of composite luting cement to zirconia ceramic surfaces. Dent Mater 2005; 21:1158-62.
- Derand T, Molin M, Kvam K. Bond strength of a composite luting agent to alumina ceramic surfaces. Acta Odontol Scand 2006; 64:227-30.
- Piwowarczyk A, Lauer H, Sorensen JA. The shear bond strength between luting cements and zirconia ceramics after two pre-treatments. Oper Dent 2005; 30:382.
- Lüthy H, Loeffel O, Hammerle CH. Effect of thermocycling on bond strength of luting cements to zirconia ceramic. Dent Mater 2006; 22:195-200.
- Yoshida K, Kamada K, Atsuta M. Effects of two silane coupling agents, a bonding agent, and thermal cycling on the bond strength of a CAD/CAM composite material cemented with two resin luting agents. J Prosthet Dent 2001; 85:184-189.
- Yoshida K, Tsuo Y, Atsuta M. Bonding of dual‐cured resin cement to zirconia ceramic using phosphate acid ester monomer and zirconate coupler. J Biomed Mater Res 2006; 77:28-33.
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Author Info
Amrutha Shenoy, Vinay Sivaswamy and Subhabrata Maiti*
Department of Prosthodontics and Implantology, Saveetha Institute Of Medical And Technical Sciences Saveetha University, Chennai, IndiaReceived: 10-Jan-2022, Manuscript No. JRMDS-22-51489; , Pre QC No. JRMDS-22-51489 (PQ); Editor assigned: 12-Jan-2022, Pre QC No. JRMDS-22-51489 (PQ); Reviewed: 26-Jan-2022, QC No. JRMDS-22-51489; Revised: 31-Jan-2022, Manuscript No. JRMDS-22-51489 (R); Published: 07-Feb-2022
