Research - (2020) Volume 8, Issue 6
Cause-Effective Relations between Vegetative Status and Inflammation Factors in the Formation of Essential Arterial Hypertension in Children
Agzamova Shoira Abdusalamovna*, Akhmedova Firuza Mirzakirovna, Makhkamova Gulnoza Turaxodjaevna and Shaykhova Munira Ikramovna
*Correspondence: Agzamova Shoira Abdusalamovna, Tashkent Pediatric Medical Institute, Uzbekistan, Email:
Abstract
Study of causal relationships between vegetative status and inflammatory factors (highly sensitive C-reactive protein (CRPhs), tumor necrosis factor-alpha (TNF-α) and anti-inflammatory interleukin-10 (IL-10) in the formation of essential arterial hypertension in children established the heterogeneity of the ergo- and trophotropic effects of the autonomic nervous system on the activity of pro- and anti-inflammatory cytokines and the level of cortisol. The clinical course of essential arterial hypertension in children is manifested by functional abnormalities, tense functioning of the autonomic nervous system, subclinical inflammation with an increase in the level of TNF-α, CRP-hs and a decrease in IL-10, which has features depending on the form of essential arterial hypertension. Increased secretion of cortisol in the group of children with arterial hypertension and the establishment of correlations different from the control and comparative groups between the studied parameters indicate a changed in the stressrealizing system of the body with overstrain of the neuroendocrine channel of blood pressure regulation with the activation of the pro-inflammatory cytokine TNF-α, which is the trigger mechanism for the formation of arterial hypertension. These changes, apparently, are characteristic of chronic stress of inflammatory genesis, which determine the pathogenetic significance in the development of essential arterial hypertension in children.
Keywords
Essential arterial hypertension, Children, Blood pressure, Autonomic nervous system, Highly sensitive C-reactive protein (CRP-hs), Tumor necrosis factor-alpha (TNF-α), Interleukin-10 (IL-10).
Introduction
As you know, health is assessed by the degree of adaptation of the organism to the environment, and the onset of the disease is considered as a phenomenon of maladjustment of functional systems. From this point of view, essential arterial hypertension is considered as a manifestation of maladjustment of the mechanisms that regulate blood pressure. The processes of adaptation and regulation of blood pressure are tightly controlled by the links of the autonomic nervous system [1-4]. Determination of heart rate is the most informative non-invasive method of qualitative and quantitative assessment of autonomic regulation of heart rate. The sympathetic and parasympathetic links of the autonomic nervous system provide a high level of adaptation of the heart rhythm. According to the results of a number of studies that study the heart rate variability in patients with arterial hypertension, it was found that the adaptive response was impaired in those examined during orthostasis and that the sympathetic component prevailed over the parasympathetic component. These deviations in the regulatory system, of course, precede hemodynamic, metabolic, and energetic disturbances. Heart rate is an indicator of these deviations and therefore its study is of great prognostic and diagnostic value in diseases of the cardiovascular system [5-7].
At present, in the study of the functional state of the autonomic nervous system in children with arterial hypertension, the assessment of autonomic tone is widely used, using Wayne tables, the calculation of the indices of the Kerdo autonomic index, the clinoorthostatic test, and the parameters of cardiointervalography. Cardiointervalography as a method for assessing the state of the autonomic nervous system has no age restrictions, is safe, non-invasive, and is used in both healthy and sick children. It allows you to characterize the activity of the sympathetic and parasympathetic parts of the autonomic nervous system through their influence on the heart rate [8-11].
The immune system, like any other system, in the process of life support of the organism is not autonomous and self-regulating. Its functional state is largely related to other systems. Integration of immunity processes with other morpho functional systems of the body, as well as the relationship between individual links within the system itself, are provided by the higher centers of the autonomic nervous system [3,5,9,12]. In this regard, it is of interest to study the factors of autonomic support of the system of immune processes in the body, which can provide a basis for a more objective scientific assessment of immune responses and their specificity and more clearly substantiate and improve methods of disease prevention, using the example of essential arterial hypertension, through the system of leading mechanisms of the autonomic nervous system. systems.
Purpose of the study. To study the causal relationships between vegetative status and inflammation factors (highly sensitive C-reactive protein (CRP-hs), tumor necrosis factor-alpha (TNF-α) and anti-inflammatory interleukin-10 (IL-10) in the formation of essential arterial hypertension in children.
Material and Methods
62 schoolchildren aged 13-16 years old (average age 14.65 ± 0.19) were examined. The surveyed children were divided into 4 groups: Control (n=20)-children with normal blood pressure, comparative (n=18)-children with high normal blood pressure, main group 1 (n=12)-children with labile arterial hypertension, the main second (n=12)-children with stable arterial hypertension.
Criteria for inclusion in a clinical study: children with grade I essential arterial hypertension, without target organ damage and children with normal and high normal blood pressure without exacerbation of chronic foci of infections within 6 months.
Exclusion criteria from a clinical study: congenital anomalies and kidney diseases, endocrine pathology, secondary or symptomatic arterial hypertension, essential arterial hypertension of II or more degree.
Comprehensive studies were carried out using standard research methods in accordance with the Russian guidelines for arterial hypertension [13].
The study was conducted in compliance with the ethical principles of the World Medical Association Declaration of Helsinki and was carried out with the informed consent of parents and patients.
Cardiointervalographic parameters were assessed according to the following indicators: fashion, variation range (Delta X), fashion amplitude and stress index (in orthostasis), initial autonomic tone and autonomic reactivity.
The degree of influence of the autonomic nervous system on the cardiovascular system was assessed by calculating the Kerdo index and diagnosing the type of self-regulation of blood circulation.
To quantitatively determine the level of cortisol in the blood serum, we used kits from Siemens (Germany) on an Immulite 2000 XPi Siemens apparatus, Germany. Values of 138-690 nmol/L are taken as the reference level of cortisol. The level of overly sensitive C-reactive protein (CRP-hs) was determined in blood serum using Siemens reagent kits (Germany) on a Dimension EXL 200 Siemens device, Germany. The CRPhs reference level is taken as 0-3.0 mg / L. Concentrations of cytokines TNF-α and IL-10 in blood serum were determined using commercial kits "Vector-Best", Russia.
Statistical processing of the material was carried out by calculating the mean values (M), their standard error (m), Student's t criteria, while the difference was considered significant at p <0.05. The "case-control" method was used to assess the frequency of exposure to risk factors by calculating the odds ratio [14]. We calculated the values of the relative risk - RR (relative risk RR=Ie/Io=[a/(a + b)]/[c/(c + d)]). The analysis of the relationship of variables was carried out with the calculation of the Spearman correlation coefficient (r) [15].
Results and Discussion
According to the results of studies of the parameters of autonomic homeostasis in relation to the level of cortisol in children with essential arterial hypertension, a significant predominance of hypersympathicotonic initial autonomic tone (p <0.001, AR=0.33) with a low level of exposure to humoral factors (p<0.05) with rest and pronounced dissipative reactions on orthostasis (hypersympathicotonic autonomic reactivity - 45.8%, (odds ratio=1.3, RR=1.2) and asymptoticotonic autonomic reactivity - 33.3%, (odds ratio=2.8, RR=2.2), respectively).
There is a clear relationship between the Kerdo index and heart rate levels of systolic blood pressure and diastolic blood pressure in the main groups. In the group of children with high normal blood pressure and labile arterial hypertension, there is a tendency to decrease the frequency of the balanced influence of the autonomic nervous system with a parallel increase in the frequency of the sympathetic influence of the autonomic nervous system on the cardiovascular system. An increase in the sympathetic effect on the cardiovascular system was significantly more often recorded in the group of children with stable arterial hypertension (p <0.01) than in the control group and, accordingly, the lowest frequency of balanced influence (p<0.05). In relation to the parameters of the type of selfregulation of blood circulation (type of selfregulation of blood circulation), the prevalence of the cardiac component in the group of children with stable arterial hypertension (p<0.001) was revealed with a statistically significant difference in relation to the control. These changes in children with essential arterial hypertension, characterize a decrease in the activity of the functioning of parasympathetic and humoral mechanisms in the system of autonomic regulation.
The compared parameters of the level of cortisol did not go beyond the normative range. But the average values of the concentration of cortisol in the blood serum in children with stable arterial hypertension (p<0.001) and with labile arterial hypertension (p<0.05) were significantly high compared with healthy children. The frequency of detecting cortisol levels> 402.2 nmol/l in children increases the odds ratio of the formation of labile arterial hypertension by 2.3 times (Odds ratio=2.3, RR=1.7) and stabilization of arterial hypertension by 3.3 times (Ratio odds=3.3, RR=1.93), as well as maintaining high normal blood pressure by 1.2 times (odds ratio=1.2, RR=1.1), respectively. Cortisol levels> 402.2 nmol/l were significant in stabilizing hypertension (RR=1.93). The data obtained have prognostic value in relation to the formation of stable arterial hypertension in children.
Analysis of the averaged parameters of the CRP-hs level found that an increase in blood pressure was associated with an increase in the CRP-hs level. In children with stable arterial hypertension, the CRP-hs level was significantly higher than in children with normal blood pressure values. In children with arterial hypertension, CRP-hs determination had high sensitivity (Se=87.5%) and specificity (Sp=86.2%), but moderate validity (73.7%), and a high diagnostic efficiency (86.7).
According to the results of the analysis of the levels of TNF-α and IL-10 in the studied groups, regularities were established between the production of TNF-α and the activity of the anti-inflammatory cytokine - IL-10. At the same time, a significantly high level of TNF-α (p <0.05) in the group of children with stable arterial hypertension was associated with insufficient production of IL-10. However, a high concentration of IL-10 (p <0.05) in children with high normal blood pressure was associated with a lower level of TNF-α (r=-0.35, p<0.05).
To date, it has been established that immune systemic inflammation is one of the main mechanisms of the development of cardiovascular pathology [11,16]. C-reactive protein (CRP), tumor necrosis factor-α (TNF-α) are associated with a high risk of complications in cardiac pathology and are considered as immunological markers of cardiovascular risk [17,18]. In several modern reviews, there is information that the variability of the increase in CRP as an indicator of systemic inflammation may have a pathogenetic significance in the development of endothelial dysfunction in essential arterial hypertension [19,20].
Overexpression of proinflammatory cytokines potentiates the progression of disorders in the blood rheology system, which is accompanied by an increase in peripheral vascular resistance, promotes the processes of vascular remodeling, impaired vascular tone, which are the trigger mechanism for the formation and progression of arterial hypertension [16,18]. At the same time, the level of TNF-α> 2.84 pg/ml determines the risk of developing essential arterial hypertension in subsequent siblings 2.2 (RR=2.2) times higher than in its absence.
The results of the mathematical analysis of pairwise correlations between the parameters of cardiointervalography and the levels of CRPhs, TNF-α, IL-10 and cortisol in the studied groups indicate the heterogeneity of the ergoand trophotropic effects of the autonomic nervous system on the activity of pro- and anti-inflammatory cytokines and the level of cortisol. Regular relationships were established between the level of cortisol in blood serum and the parameters of the functioning of the cardiovascular system, as well as the constants of cardiointervalography in children with different values of blood pressure.
In children of the control group (Figure 1), there were direct correlations between the level of cortisol and indicators of heart rate, Kerdo index, mod amplitude parameters, stress index 1 and stress index 2 (r=+0.25, p>0.05, r=+0.44, p<0.01, r=+0.53, p<0.001, r=+0.51, p<0.001, r=+0.50, p <0.001, respectively). An inverse correlation was established between the level of cortisol and the values of the type of selfregulation of blood circulation (r=-0.45, p<0.01). Direct correlations were established between CRPhs and values in orthostasis of the mode amplitude, stress index 2, autonomic reactivity, cortisol level (r=-0.50, p<0.001, r=0.48, p<0.01, r=0, 41, p<0.01, r=0.34, p<0.05, respectively). For TNF-α, multidirectional relationships were revealed: positive with amplitude mode, delta X (in orthostasis), (r=0.53, p<0.001 r=0.45, p<0.01,) and negative with amplitude mode, delta X, stress index 2, autonomic reactivity in orthostasis, (r=-0.42, p<0.01, r=-0.40, p<0.01, r=-0.42, p<0.01, respectively).
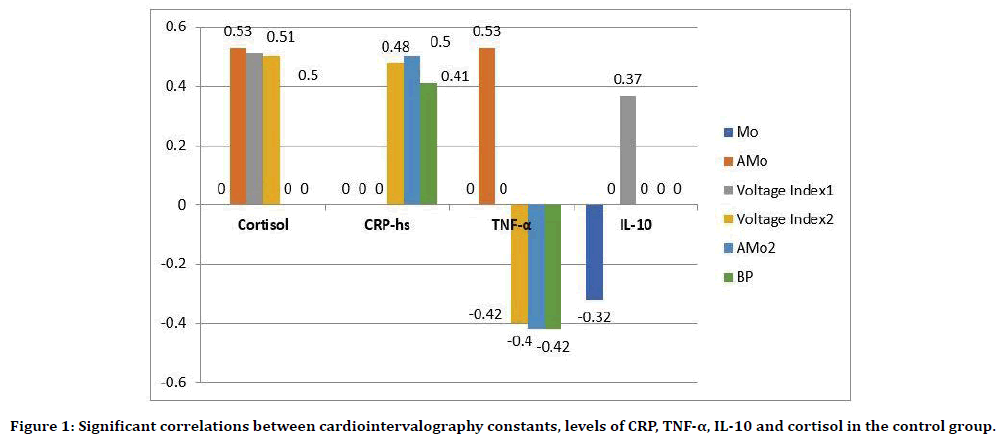
Figure 1. Significant correlations between cardiointervalography constants, levels of CRP, TNF-α, IL-10 and cortisol in the control group.
Children with high normal blood pressure (Figure 2) were characterized by a decrease in the strength of multidirectional correlations between the level of cortisol and indicators of the Kerdo index and the type of self-regulation of blood circulation (r=+ 0.21, p> 0.05, r=-0.21, p> 0.05, respectively); disappearance of connections with the amplitude of the mode and stress index 1 and stress index 2, but the appearance of a direct average strength of the connection with the Mode in orthostasis (r=+0.50, p<0.001). The connections between CRP-hs and systolic, diastolic blood pressure, such as self-regulation of blood circulation, delta X with an inverse vector (r=-0.37, p <0.05, r=-0.58, p <0.001, r=- 0.65, p <0.001, r=-0.37, p<0.05, respectively) and values of heart rate, Kerdo index, stress index 1 with positive (r=0.48, p <0.05, r=0.65, p <0.001, r=0.52, p<0.001, respectively) with positive.
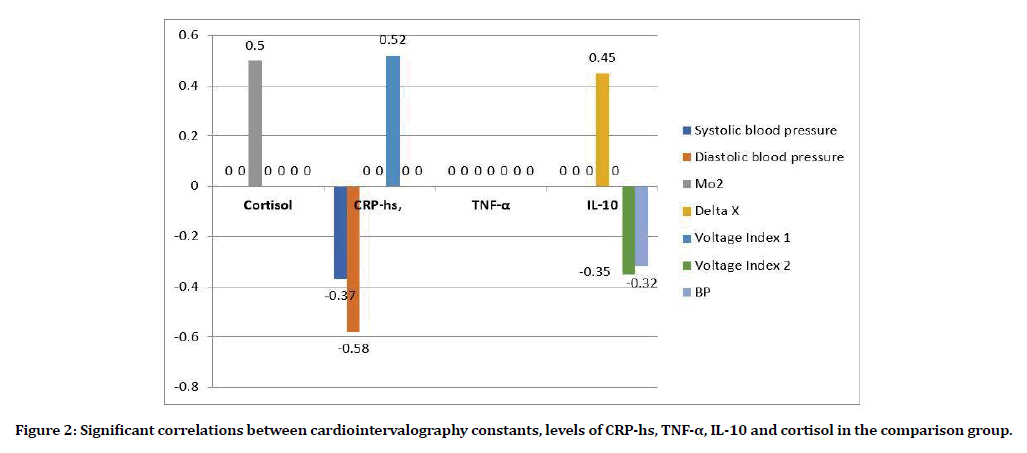
Figure 2. Significant correlations between cardiointervalography constants, levels of CRP-hs, TNF-α, IL-10 and cortisol in the comparison group.
In children with labile arterial hypertension, the values of the correlation coefficients between the level of cortisol and heart rate indicators, Kerdo index, mod amplitude parameters, stress index 2 and the type of blood circulation selfregulation were not established. Relationships of low strength without statistical significance with stress index 1, delta X, mode amplitude in orthostasis and autonomic reactivity (r=0.23, p> 0.05, r=-0.29, p>0.05,=-0 , 26, p>0.05, r=- 0.25, p>0.05, respectively) were typical for children with labile arterial hypertension. Also found the only reliable relationship, inherent only in this group of children, between the levels of cortisol and IL-10 (r=0.52, p<0.01). Perhaps this fact indicates the stabilizing effect of the stress hormone on the production of the anti-inflammatory cytokine IL-10 in an uncontrolled process of systemic inflammation. Multidirectional connections appear between TNF-α and Kerdo index indicators, such as self-regulation of blood circulation (r=- 0.50, p<0.05, r=0.50, p<0.05, respectively) with the disappearance of connections with cardiointervalography constants in orthostasis. Identical dynamics can be traced between CRPhs parameters delta X, stress index 2, autonomic reactivity in orthostasis (r=0.45, p <0.01, r=- 0.35, p <0.05, r=-0.32, p<0.05, respectively).
Completely different correlations were found in the group of children with stable arterial hypertension (Figure 3). Significant direct correlations were established between the level of cortisol and heart rate parameters, the amplitude of the mode in orthostasis and the stress index 2 (r=0.52, p<0.01, r=0.44, p<0.05, r=0.46, p<0.05, respectively), as well as the feedback between the mode in orthostasis (r=-0.43, p<0.05). Only in this group were the dependences of diastolic blood pressure on the level of cortisol (r=0.28, p>0.05), Maud on CRPhs (r=0.46, p<0.05) noted. Relationships were found between TNF-α and systolic arterial pressure (r=-0.60, p<0.001), delta X, stress index 1 (r=-0.42, p<0.05, r=0.40, p<0.05, respectively), absent in the compared groups. New relationships were established between IL-10 and the values of delta X, Mod (in orthostasis) (r=0.49, p<0.05, r=- 0.40, p<0.05, respectively).
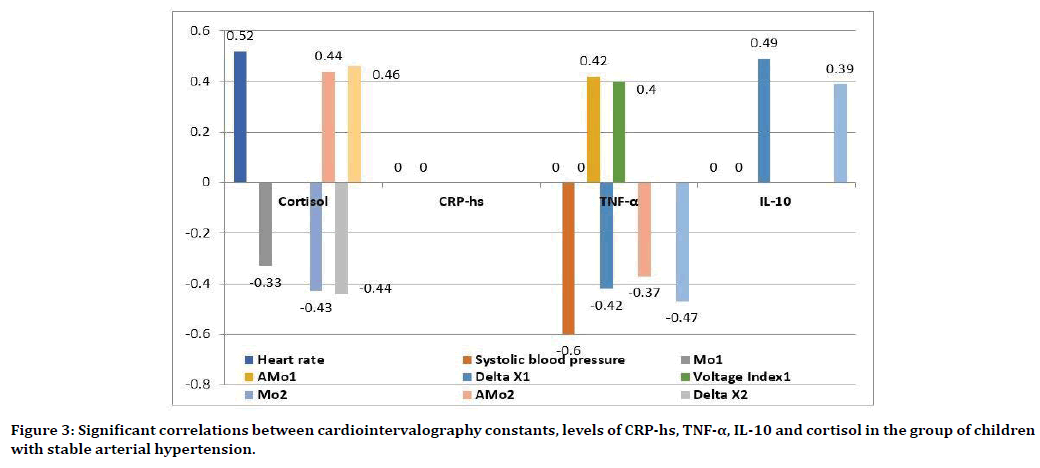
Figure 3. Significant correlations between cardiointervalography constants, levels of CRP-hs, TNF-α, IL-10 and cortisol in the group of children with stable arterial hypertension.
Conclusion
Revealed relationships between the values of cortisol, inflammation factors and parameters of the functioning of the cardiovascular system, as well as the constants of cardiointervalography testified to the preservation of intrasystemic regulatory mechanisms that ensure the physiological state of the cardiovascular system in children with normal blood pressure values.
Children with high normal blood pressure were characterized by a more compensated state of the neurohumoral level of regulation of the heart and blood pressure through the vascular system, with the involvement of the inflammatory factor as a highly sensitive C-reactive protein (CRPhs) in the process, which indicates a protectiveadaptive response of the body.
An increase in the secretion of cortisol in the group of children with arterial hypertension and the establishment of other correlations indicate a change in the stress-realizing system of the body with an overstrain of the neuroendocrine channel of blood pressure regulation with the activation of the pro-inflammatory cytokine - TNF-α, which are the triggering mechanism of formation arterial hypertension. These changes, apparently, are characteristic of chronic stress of inflammatory genesis, which determine the pathogenetic significance in the development of essential arterial hypertension in children.
Acknowledgments
We are grateful to the staff members of Tashkent Pediatric Medical Institute for the cooperation and support in our research. The participants kindly gave full written permission for this report.
Consent
Written informed consent was obtained from all participants of the research for publication of this paper and any accompanying information related to this study.
Conflict of Interest
The authors declare that they have no competing interests.
Funding
No funding sources to declare.
References
- Flynn JT, Kaelber DC, Baker-Smith CM, et al. Clinical practice Guideline for screening and management of high blood pressure in children and adolescents. Pediatr 2017; 140:e20171904.
- http://apps.who.int/iris/bitstream/10665/148114/1/9789241564854_eng.pdf?ua=1
- Wayne AM, Voznesenskaya TG, Vorobieva OV. Vegetative disorders: Clinical picture, diagnosis, treatment. A guide for doctors. Edn Golubeva VL. Moscow: Medical Information Agency, 2010.
- Litwin M, Feber J, Ruzicka M. Vascular Aging: Lessons from pediatric hypertension. Canadian J Cardiol 2016; 32.
- Akhmedova FM, Agzamova SA, Shamansurova EA. Vegetative status and cortisol level in school age children with normal, high normal arterial pressure and essential arterial hypertension. Central Asian J Pediatr 2019; 2:191-196.
- Agzamova SA, Akhmedova F, Shamansurova EA. Evaluation of potentially removable risk factors of arterial hypertension in children of Uzbekistan. Eur Sci Review 2018; 7:72-75.
- Agzamova SA, Hasanova GM. Obesity in children: Frequency of occurrence and features of thickness of epicardial fat depending on indicators of body weight index and lipid spectrum. Int J Psychosocial Rehab 2020; 24:434-442.
- Kaladze NN, Zyukova IB. The state of the stress implementing system in children with arterial hypertension. Modern Pediatr 2013; 5:147-150.
- Timofeeva EP, Ryabichenko TI, Skosyreva GA, et al. The state of the autonomic nervous system in adolescents 15–17 years old. Russian Bulletin Perinatol Pediatr 2016; 4:82-87.
- Ledyaev MYA, Mozoleva SS, Gavrikov LK. Early diagnosis of arterial hypertension in adolescent children. Health Uzbekistan 2019; 2:40-43.
- Ewald DR, Haldeman LA. Risk factors in adolescent hypertension. Glob Ped Health 2016; 3.
- Gaiduk TA, Shostakovich-Koretskaya LR, Gaiduk OI. Immunological factors of cardiovascular risk (TNF-α) depending on various hemodynamic forms of arterial hypertension in adolescents. Klinichna Med 2018; 2:29-33.
- Agapitov LI, Cherepnina IV. Diagnostics, treatment, and prevention of arterial hypertension in children and adolescents. J Cardiovascular Therapy Prevention 2009; 8:32.
- Ponomareva LA. Using the principles of evidence-based medicine in the organization and conduct of hygienic research (Method Recommended). Tashkent 2004; 25.
- Kelmanson IA. Principles of evidence-based pediatrics. Foliant 2004; 240.
- Barbaro NR, De Araujo T, Tanus-Santos JE, et al. Vascular damage in resistant hypertension: TNF-α inhibition effects on endothelial cells. BioMed Res Int 2015; 631594.
- Nazheva MI, Demidov IA. Diagnostic value of determining the baseline concentrations of C-reactive protein and interleukin-6 in the blood for assessing the risk of cardiovascular diseases. Med Bulletin South Russia 2015; 3:86–91.
- Seminsky IZH, Serebrennikova SN, Guzovskaya EV, et al. The role of cytokines in the pathogenesis of diseases. Siberian Med Magazine 2015; 1:14-17.
- Khaybullina Z. Inflammation and oxidative stress: Critical role for metabolic syndrome-Mini-review. J Vasc Med Surg 2017; 5: 302.
- Khaybullina Z, Zufarov M, Sharapov N, et al. Oxidative stress-induced effects on proinflammatory cytokines and vascular endothelial growth factor after interventional treatment of coronary heart disease. J Clin Exp Cardiolog 2017; 8:6.
Author Info
Agzamova Shoira Abdusalamovna*, Akhmedova Firuza Mirzakirovna, Makhkamova Gulnoza Turaxodjaevna and Shaykhova Munira Ikramovna
Tashkent Pediatric Medical Institute, Tashkent, UzbekistanCitation: Agzamova Shoira Abdusalamovna, Akhmedova Firuza Mirzakirovna, Makhkamova Gulnoza Turaxodjaevna, Shaykhova Munira Ikramovna, Cause-Effective Relations Between Vegetative Status and Inflammation Factors in the Formation of Essential Arterial Hypertension in Children, J Res Med Dent Sci, 2020, 8 (6): 12-18.
Received: 24-Aug-2020 Accepted: 08-Sep-2020
