Research - (2022) Volume 10, Issue 1
Causes and Patterns of Traumatic Mandibular and Maxillofacial Fractures in Saudi Arabia: Systematic Review and Meta-Analysis
Noura Alsufyani1,2*, Rabab Bukhamseen3 and Majd Qadoumi3
*Correspondence: Noura Alsufyani, Department of Oral & Maxillofacial Radiology, Oral Medicine and Diagnostic Sciences, College of Dentistry, King saud university, Riyadh, Kingdom of Saudi Arabia, Email:
Abstract
Aims: to assess the demographic distribution, causes and types of mandibular-maxillofacial (MM) traumatic fractures in the Kingdom of Saudi Arabia (KSA). Methods: Several databases were searched for reports on MM factures in the KSA. Variables collected from articles that met inclusion criteria were: age, gender, city in KSA, cause and site of facial trauma. Results: 19 of 41 articles were eligible for data collection. Most subjects were male, 6,416 (23.5%) and >18 years old, 4,067 (56.8%). Of 8,981 fractures, there were 504 (5.6%) dentoalveolar, 1,867 (20.8%) zygomatico-maxillary complex, and 4,314 (48.0%) mandibular- with condylar fracture being the most frequent mandibular fracture, 969 (10.8%). Motor-vehicle accident (MVA) was the leading cause of MM fracture in KSA with pooled prevalence of 55.5% (39.0%-71.3%, I2=99.4%). Mandibular fracture was the most common site of fracture with pooled prevalence of 45.2% (35.5%-55.1%, I2=98.5%). Conclusion: Fracture of the mandible is the most common type of fracture and MVA remains the main cause of MM trauma. Young male adults comprise the majority of demographics. Medical studies on this topic lag behind recently published non-medical reports that take into account the implementation of stringent seatbelt and speed laws, and recently-allowed female driving in KSA.
Keywords
Prevalence, Fractures, Facial bones, Mandible, Meta-analysis
Introduction
The Kingdom of Saudi Arabia (KSA) has one of the highest rates of road-traffic deaths in the world, with an increase from 17.4 to 27.4% people dying for every 100,000 since the last decade [1]. Motor vehicle accidents (MVA) are the main cause of trauma in KSA and worldwide. In the KSA, around four people are injured per hour and 81% of total fatalities in hospitals are due to MVA, with majority of victims being young adults causing devastating social, economic, and health consequences [2].
Other causes of trauma are due to fall, physical or firearm assault, sports, work-related, animal attacks, and others. The etiology of fractures has shifted throughout the past three decades due to changes in culture, economics, and traffic regulations [3]. Mandibular-maxillofacial (MM) trauma may present as a single or multiple fracture(s) and may cause pain, masticatory dysfunction, speech impairment, facial disfigurement, emotional distress, and reduced quality of life.
The incidence and patterns of MM trauma in KSA have been recently reported in a systematic review, however the authors recorded the fracture site as maxilla and mandible only, and failed to record causes other than MVA for 5 out of 13 articles included.[4] Studies that reported the frequencies of facial trauma and/or causes in KSA show large variability in the study design, cohort age, single city or medical centre from which the data was collected [4].
This study aims to determine, via systematic review and meta-analysis, the proportion of MM fractures resulting from different traumatic etiologies among adults and children in KSA.
Materials and Methods
Article screening and evaluation
The search was completed following the PRISMA guidelines in three phases:
Phase I: Identification and screening
An electronic search strategy was developed for PubMed (Table 1) and adapted for each of the following bibliographic databases and grey literature: PubMed, Scopus, Web of Science, and Google scholar. The search started June/2019 and concluded at the end of March/ 2020.
| Search | Query | #of article hits |
|---|---|---|
| #1 | “maxilla” OR “maxillary” OR “maxillofacial” OR “facial” OR “mandible” OR “mandibular” OR “jaw” OR “jaws” | |
| #2 | “trauma” OR “fracture” OR “injury” OR “injuries” | |
| #3 | “Saudi Arabia” OR “Kingdom of Saudi Arabia” OR “KSA” OR “Saudi” | |
| #4 | #1 AND #2 AND #3 | Pubmed 12 |
| Scopus 33 | ||
| Web of Science 19 |
Inclusion criteria: Human studies, reporting trauma in the maxillofacial and/or mandibular structures, in KSA.
Exclusions: Editorials/letter to the editor and studies reporting dental fractures only. The titles and abstracts of the articles were reviewed for inclusion to the next phase.
Phase II: Eligibility
Full article review was completed, and inclusion/ exclusion criteria applied. Using the references of the included articles, manual search was completed to search for relevant articles possibly missed from the electronic search.
Phase III: Included studies
The Newcastle-Ottawa scale [5] was used for methodological quality and risk of bias assessment. Demographic data (age and gender), site of fracture, cause of trauma, and city in KSA were collected for each study.
Two reviewers (RB and MQ) individually conducted the review. Any uncertainty or disagreement about an article was resolved by discussion and consensus among the reviewers and the supervisor (NA).
Statistical analysis
Eligible studies were included for meta-analysis to calculate the overall rate of common trauma sites and causes by pooling with a random effects model. To visualize rates and corresponding 95% CIs within and across the common sites and causes of trauma, forest plots were generated. The I2 statistics were calculated to assess for heterogeneity and Egger’s regression to assess publication bias. The analyses were performed using MedCalc Statistical Software V. 19.2.6 (MedCalc Software Ltd, Ostend, Belgium). For all statistical tests, p<0.05 was considered statistically significant.
Results
A total of 81 articles were screened for inclusion criteria. Of these, 19 articles were eligible for systematic review. The meta-analysis for trauma cause was completed for 14 articles, and 15 articles for the trauma site, Figure 1. Of the articles included, 8 were of high quality, the remaining 11 articles were of moderate quality.
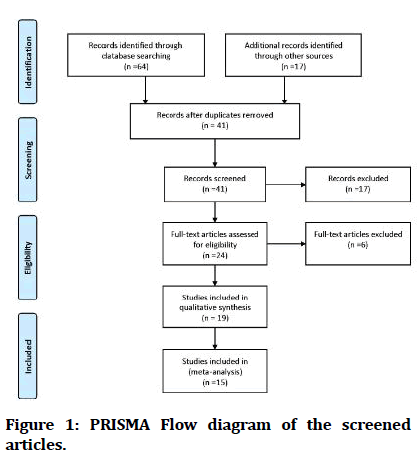
Figure 1: PRISMA Flow diagram of the screened articles.
Of the 8,233 subjects with MM fracture, 6413 (77.9%) were males and 4305 (52.3%) were adults. One study[6] from AlQurayyat city reported the highest number of subjects (n=2160) followed by eight studies [3,7-13] from Riyadh (n=1442), one study [14] from Makkah (n=1130), and three studies[15-17] from Madinah (n=1465). Other single studies from other cities are: Jeddah [18], Aseer region [19], AlBaha [20], Hofuf [21], Khamis Mushait [22], and Tabuk [23].
The most common cause of traumatic MM fractures in Saudi Arabia was MVA, 3074 (45.4%). The frequency of other trauma causes is presented in Figure 2. The most common fracture site was the zygomaticomaxillary complex (ZMC), n=1867 (20.7%), followed by the mandible n=4,314 (48.0%); of which n=969 (10.7%) were in the condylar head, then the dentoalveolar area n=504 (5.6%). Frequency of other sites is presented in Figure 3. Detailed descriptive data of each study are summarized in a Table 2.
| Study (Sample size) [Bias/quality score] | Age (years) | Gender | City | Reason for trauma | Type of fracture | Total fracture | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | Fall | Sport | MVA | Assault | Other | ||||||
| Al Arfaj et al [10] (n= 102) [Moderate] | <18 | 41 | 16 | Riyadh | 30 | 14 | 7 | 6 | Nasal 45 | 45 | ||
| Abdullah et al [3] (n= 97) [Moderate] | <18 | 69 | 13 | 19 | 7 | 49 | 6 | NR 1 | Condyle 42 | DenAlv 24 | 303 | |
| Coronoid 3 | ZMOC 73 | |||||||||||
| Ramus 2 | Nasal 6 | |||||||||||
| Angle 33 | Lefort I 14 | |||||||||||
| Body 30 | Lefort II 6 | |||||||||||
| Parasym 56 | Lefort III 2 | |||||||||||
| >18 | 103 | 15 | 21 | 4 | 73 | 17 | NR 3 | Sym 12 | ||||
| Almasri et al [19] (n= 95) [Moderate] | NR | 92 | 3 | Aseer | - | 3 | 90 | 8 | Condyle 31 | DenAlv 6 | 134 | |
| Coronoid 2 | ZMOC 27 | |||||||||||
| Ramus 1 | Frontal 21 | |||||||||||
| Angle 18 | ||||||||||||
| Body 8 | ||||||||||||
| Parasym 29 | ||||||||||||
| Sym 1 | ||||||||||||
| Samman et al [16] (n= 197) [Moderate] | <16(44) | 34 | 10 | Madinah | 12 | 2 | 178 | 5 | Condyle 103 | DenAlv 22 | 260 | |
| Coronoid 7 | ||||||||||||
| Ramus 5 | ||||||||||||
| Angle 51 | ||||||||||||
| Body 23 | ||||||||||||
| >16(153) | 131 | 22 | Parasym 45 | |||||||||
| Sym 4 | ||||||||||||
| Alsuliman et al [11](n= 306) [Moderate] | <20 (96) | 271 | 35 | Riyadh | 4 | 4 | 66 | 21 | Camel attack 4 | ZMC 283 | 303 | |
| Zyg arch 20 | ||||||||||||
| >20 (210) | 13 | 6 | 155 | 33 | ||||||||
| Bokhamseen et al [21] (n= 270) [High] | <18 (78) | 68 | 10 | Hofuf | 43 | 22 | 171 | 18 | Gunshot 2 | Condyle 56 | ZMOC 86 | 476 |
| Occ. 8 | Angle 51 | Nasal 11 | ||||||||||
| Body 58 | Orbital 57 | |||||||||||
| Ramus 4 | Zyg arch 19 | |||||||||||
| Animal attack 6 | Coronoid 3 | Lefort I 20 | ||||||||||
| Parasym 64 | Lefort II 18 | |||||||||||
| >18 (192) | 173 | 19 | Sym 24 | LEfort III 5 | ||||||||
| Aldwsari et al [9] (n= 237) [High] | <20 (46) | 231 | 6 | Riyadh | - | - | 237 | - | Condyle 4 | Max sinus 29 | 222 | |
| MANDIBLE 18 | Orbit 22 | |||||||||||
| Parasym 4 Temporal 33 Parietal 44 | Occipital 4 | |||||||||||
| Zyg arch 15 | ||||||||||||
| Frontal 29 | ||||||||||||
| Nasal 17 | ||||||||||||
| >20 (191) | Sphenoid 3 | |||||||||||
| Rabi et al [17] (n= 403) [Moderate] | <20 (134) | 337 | 66 | Madinah | 66 | 13 | 225 | 27 | Occ. 14 | Condyle 83 | DenAlv 31 | 585 |
| Angle 46 | Zygoma 117 | |||||||||||
| >20 (266) | Body 96 | Nasal 42 | ||||||||||
| Sym 38 | Orbital 35 | |||||||||||
| Parasym 41 | Lefort I 7 | |||||||||||
| Lefort II 39 | ||||||||||||
| Lefort III 10 | ||||||||||||
| Alqahtani22 2018 (n= 205) [Moderate] | <25 | 114 | 0 | Khamis Mushait | - | - | - | 215 | - | DenAlv 105 | 191 | |
| >25 | 91 | Mandible 58 | ||||||||||
| Maxilla 17 | ||||||||||||
| Zygoma 11 | ||||||||||||
| Shalhoub et al [8] (n= 2) [Moderate] | >20 | 2 | 0 | Riyadh | - | - | - | - | Occ. 2 | Mand body 2 | 4 | |
| Sym 1 | ||||||||||||
| Max sinus 1 | ||||||||||||
| Lawoyin et al [20] (n= 473) [Moderate] | <15 | 332 | 141 | Albaha | - | - | 90 | 84 | Gunshot 4 | Mandible 41 | 89 | |
| NR 9 | Nose 39 | |||||||||||
| Maxilla 9 | ||||||||||||
| Brown et al. [12] (n= 268) [Moderate] | 27.1 (age range 2-78) | 214 | 54 | Riyadh | 40 | 15 | 200 | 0 | 5 Gunshot | Condyle 134 | Lefort I 94 | 552 |
| 8 Occ. | Ramus 11 | Lefort II 153 | ||||||||||
| Angle 72 | Lefort III 21 | |||||||||||
| Body 59 | ||||||||||||
| Symp 8 | ||||||||||||
| Lawoyin et al [23] (n= 140) [High] | <20 [57] | 135 | 5 | Tabuk | 13 | 21 | 85 | 10 | 11 others | Condyle 7 | DenAlv 8 | 143 |
| >20 [83] | Ramus 8 | Nasal 52 | ||||||||||
| Angle 1 | Zygoma 17 | |||||||||||
| Body 25 | Orbit 12 | |||||||||||
| Lefort I 6 | ||||||||||||
| Lefort II 5 | ||||||||||||
| Frontal 2 | ||||||||||||
| Alhammad et al [7] (n= 372) [High] | <15 (n=9) | 325 | 47 | Riyadh | 40 | 16 | 295 | 12 | 9 | Condyle 30 | DenAlv 30 | 531 |
| Coronoid 3 | Nasal 38 | |||||||||||
| Ramus 4 | Zygoma 119 | |||||||||||
| Angle 21 | Orbit 109 | |||||||||||
| Body 21 | Lefort I 23 | |||||||||||
| Sym 14 | Lefort II 34 | |||||||||||
| >15 (363) | Parasym 10 | Le fort III 8 | ||||||||||
| Albeshir et al [15] (n= 865) [High] | <12 | 531 | 334 | Madinah | 776 | 4 | 71 | 12 | Gunshot 1 | Mandible 60 | 85 | |
| Maxilla 4 | ||||||||||||
| Animal 1 | Orbital 10 | |||||||||||
| Zygoma 6 | ||||||||||||
| Frontal 3 | ||||||||||||
| Nasal 2 | ||||||||||||
| Almasri et al [14] (n= 1130) [Moderate] | <16 (n=135) | 904 | 226 | Makkah | NR | Mandible 523 | ||||||
| Orbital floor 25 | ||||||||||||
| >16 (n=995) | ZMC 399 | |||||||||||
| NOE/frontal 18 | ||||||||||||
| Ahmed Jan et al [18] (n= 853) [High] | <20 (n=109) | 728 | 125 | Jeddah | 77 | 60 | 570 | 17 | Occ. 68 | Body 264 | DenAlv 183 | 1650 |
| Angle 247 | Le Fort I 32 | |||||||||||
| Animal 51 | Ramus 122 | Le Fort II 74 | ||||||||||
| >20 (n=744) | Sym 176 | Le Fort III 28 Zygoma 116 Fronto-NE 18 | ||||||||||
| Gunshot 8 | Condyle 390 | |||||||||||
| Alanazi et al [6] (n= 2160) [High] | <12 | 1490 | 670 | Qurayyat | 942 | 356 | 512 | 350 | DenAlv 308 Mandible 452 Zygoma 157 | 1191 | ||
| (n=1417) | Maxilla 143 | |||||||||||
| NOE 95 | ||||||||||||
| >12 (n=743) | Frontal 36 | |||||||||||
| Nwoku et al [13] (n= 986) [High] | <20 (n=140) | 828 | 158 | Riyadh | - | 48 | 1050 | - | Other 63 | Condyle 89 | 1522 | |
| Gunshot 9 | Coronoid 9 | ZMC 193 | ||||||||||
| >20 (n=846) | Occ. 36 | Angle 163 | Orbital 316 | |||||||||
| Body 79 | Lefort I 178 | |||||||||||
| Parasym 61 | Lefort II 214 | |||||||||||
| Sym 65 | Lefort III 155 | |||||||||||
| Sym: symphysis, Parasym: parasymphysis, DenAlv: Dento-alveolar, ZMC: Zygomatico-maxillary complex, NOE: Naso-Orbital-ethmoidal complex, Occ.: Occupational | ||||||||||||
Table 2: Descriptive data for the included articles.
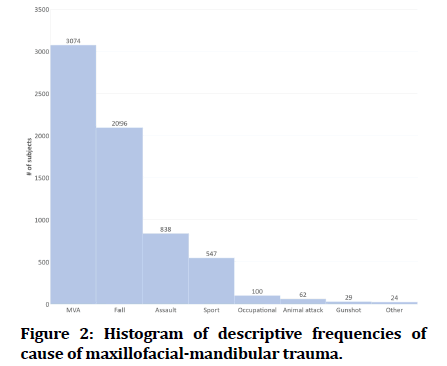
Figure 2: Histogram of descriptive frequencies of cause of maxillofacial-mandibular trauma.
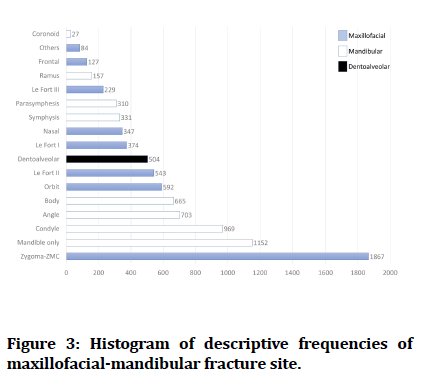
Figure 3:Histogram of descriptive frequencies of maxillofacial-mandibular fracture site.
Meta-analysis for trauma causes excluded: Aldwsari et al [9] (for exclusively reporting MVA cases), Alqahtani [22] (for exclusively reporting assault cases), Almasri et al [14] and Nwoko et al[13] (did not report the cause), and Shalhoub et al [8] (n=2 work-related injuries in the mandible). The four most common causes of trauma were taken into consideration for the meta-analysis i.e., MVA, fall, sports, and assault. Metanalysis for trauma sites excluded: AlArfaj et al[10] (exclusively reported nasal bone fracture), Samman et al [16] (exclusively reported mandibular bone fracture), Alsuliman et al [11] (exclusively reported zygomatic bone fracture), and Shalhoub et al [8] (n=2 work-related injuries in the mandible). Since dentoalveolar site was not consistently reported nor specifically excluded in the studies, metaanalysis of this site was not carried-out. For the metanalysis, the trauma sites were classified to four large categories: Mandibular, zygomatico-maxillary-orbital complex (ZMOC), nasal, and Lefort.
The data was heterogeneous, accordingly random effects model was chosen. The pooled prevalence of MVAs in KSA was 55.5% (95% CI 39-71.3%), 17.2% (95% CI 5.3-34.1%) for falls, 6.8% (95% CI 3.5-11.3%) for assaults, and 5.5% (95% CI 2.5-9.7%) for sports. The prevalence and 95% CI for each etiology are presented in Figure 4.
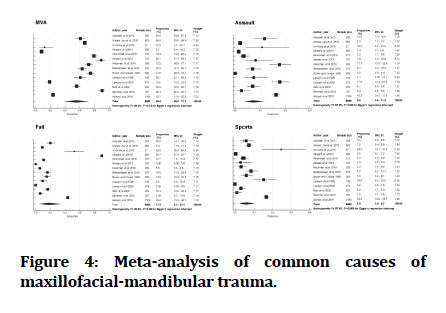
Figure 4:Meta-analysis of common causes of maxillofacial-mandibular trauma.
The pooled prevalence of mandibular fracture in KSA was 45.2% (95% CI 35.5-551%), 21.9% (95% CI 14.0-31.1%) for ZMOC, 4.3 % (95% CI 1.8-8.0%) for nasal bone, and 5.5% (95% CI 1.1-13.0%) for Lefort fractures. The prevalence and 95% CI for each site are presented in Figure 5.
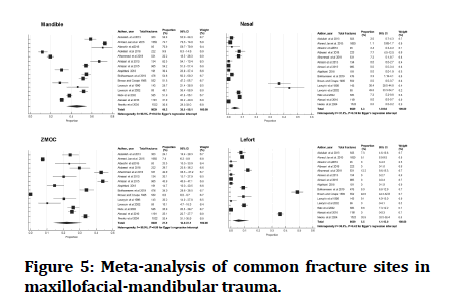
Figure 5:Meta-analysis of common fracture sites in maxillofacial-mandibular trauma.
Publication bias was analyzed by Egger's regression which was found non-significant for all etiology and site outcomes, p>0.05, except for sports (p<0.001).
Discussions
The Kingdom of Saudi Arabia consists of 13 regions with 46 main cities, yet only 10 cities were covered by this systematic review. The most frequent reports were from the capital city of Riyadh and the second largest metropolitan city of Jeddah. Frequent studies emerged from the two holy cities of Makkah and Madinah that house two Holy Mosques to which millions of Muslim pilgrims visit every year. This added traffic is likely associated with higher road traffic accidents. The lack of reports from other cities in KSA should not be misinterpreted as low levels of trauma; rather it means a lack of research either due to small university, hospital, or medical centres.
The demographic analysis in this systematic review revealed that most MM trauma was sustained by males (77.9%) and adults (52.3%), which is in line with previous studies across the globe [24-28]. The age and gender distribution will be affected by the cause of trauma and demographic of the studied society. For example, the Saudi cohort was younger than the Australian, median age 36 vs. 50 years, in a study of MM of injuries caused by MVA [29]. Abdullah at el[3] showed how MM trauma in KSA differs in adult vs. pediatric MVA (37% vs. 25%) and assault (8.6% vs. 3%). Conceptually, sustaining trauma to the MM structures due to MVAs, sports, occupational, physical and armed assaults are likely to occur in the adult and male cohort. In the KSA, the employment rate of women between the age of 25 to 34 years old has risen to 53.3% and the ban of women driving has been lifted since 2018. The studies included in this review did not compare the frequency of MM trauma between male and female across the years. Even if they did, it is possible that not enough years have passed to detect such a change.
MVA was the leading cause of fracture in this review, pooled prevalence 55.5%, similar to reports from China, Iran, Greece, and Brazil (range 45- 72%)[26-28, 30, 31]. North America, Europe, and Australia showed a decrease in MVA (8.4- 19.2%); attributed to increased road safety laws[24, 32-34]. In a five-region hospital study in KSA, the prevalence of non-use of a car seat or seatbelt was 44.0- 56.1%, 24.4% of children were seated in the front seat, 20% of 14 -16-year-olds were drivers, and 21.7% of <4-year-olds were sitting on the passengers’ lap[35]. Moreover, it was only in 2010 and 2018 that the KSA launched one of the largest automated speed enforcement cameras in the world “Saher”, and applied electronic surveillance of seatbelts and cell phone use while driving [36]. In the recent Saudi Vision 2030 progress report, the number of traffic accident fatalities per 100,000 population showed a 53% decrease from 2010 to 2020, and head injuries from 16.4% to 3.6% [37,38]. Future studies reporting MM trauma due to MVA sustained after 2018 could analyze the possible effect of the newly implemented road surveillance system.
The next leading etiologies of MM fractures in KSA were fall (pooled prevalence 17.2%), assault (pooled prevalence 6.8%), then sports (pooled prevalence 5.5%), figure 4. Occupational, animal related, and gunshot injuries were minimally reported, figure 2. The prevalence of MM trauma due to fall is bimodal; high in children and old subjects, and that of sports is usually higher in active youth populations. The studies by Alarfaj and Albeshir [10, 15] (exclusively reported MM trauma in children) showed higher frequencies of fall and sport injuries over MVAs with visible asymmetries in the forest plots (figure 4), as well as publication bias in the 5.5% pooled prevalence of sports. In a recent study in Najran, KSA, falls accounted for most of the etiology in the 1-5- year group whereas in the 16-20-year group, MVA was the main reason [39].
Fall was the leading cause of MM trauma in USA, China, and Europe (30.9-46%)[24, 26, 40]. Assaults, interpersonal violence, or gunshot injuries were the leading cause in USA, Brazil, Europe, Australia (26-60.5%) [24,25,28,41]. Generally, alcohol consumption was a significant contributor to the increased incidence and severity of MM trauma in MVA, fall, and assault [25,33,40]. Unlike the USA, the possession of firearm in KSA is permitted only with reason (sport shooting license or proving danger to life). Furthermore, the possession and consumption of alcohol are not permitted in KSA due to religious rules. Collectively, this may explain the lower provenances of trauma due to assault. MM trauma due to sports is generally low throughout the world except for Europe; explaining 10% of MM fractures [40].
Reporting the site of trauma was not consistent throughout the studies. For example, fractures of the mandible were detailed by sub segment and in others were reported as “Mandible” only. Of the 8,981 fractures, the most common site was in the mandible at pooled prevalence of 45.2%, figure 5. The ZMOC was the next common site of fracture at pooled prevalence of 21.9%.
Lefort fractures and fractures of the nasal bone were not frequently counted in the included articles. The pooled prevalence was 4.3% for nasal bone fracture and 5.5% for Lefort fractures. Both rates are possibly inflated due to two studies by Lawoyin et al [20] for nasal fracture, and Brown and Cowpe [12] for Lefort fractures; one a tertiary trauma centre and the other a military hospital.
Studies in China, Greece, Brazil, and Romania were similar to the KSA in having mandibular fracture as the most common type of fracture (40.0-67.1%)[26, 30, 31, 34]. Studies in USA, Australia, and Iran reported fractures of the ZMC as the leading site and at a much higher proportion than the KSA (50.2-68.4%)[24, 27, 32].
The magnitude and direction of force are important factors in determining the site of fracture. Fracture of the mid-face, Lefort-types and Comminuted fractures are expected in high velocity impacts such as MVA and gunshot wounds compared to falls and assaults[25, 41]. Almasri et al[19] recorded a high frequency of MVA, 89.1%, relative to other causes within their study, figure 4, yet did not record any Lefort fractures, figure 5. It is accepted that high forces of MVA would result in debuckling of the facial buttresses seen in Lefort fractures, so the lack of such fractures was likely due to the authors’ decision not to include such fractures. Brazil and China report similar frequencies of Lefort fractures (6-8%), Romania and USA reported lower numbers (1.7-2%), and Greece reported 13.6%[24, 26, 30, 31, 34]. Nasal bone fractures reported in USA, Greece, and Romania are similar to the KSA (1-6.9%) whereas Australia, Brazil, and Iran showed higher numbers (16.2-43.9%)[24, 27, 30-32, 34].
The results may vary depending on the geographic area, population density, socioeconomic status, specific period, governmental laws of the region, and the source i.e. the hospital or centre [4,33].
None of the studies in this review attempted to relate the fracture site to the etiology of trauma.
In the KSA, and across the globe, there is variability in sample sizes, inconsistency in reporting certain MM fracture etiologies or sites, and substantial heterogeneity is often observed across studies resulting in large confidence intervals.
To remedy this, data collection for MM trauma studies should be collected from a nation-wide registry. The Saudi Trauma Registry (STAR) was established in 2017 and fully operational by 2018[42]. STAR offers large sample sizes, covers major parts of the KSA, and consistent reporting of variables (demographics, cause and site of trauma, treatment offered, days in hospital etc.). Interested researchers are encouraged to utilize this nationwide database and avoid cross-sectional or retrospective analyses of single centres. Applying this in the KSA, and in other countries, will allow robust global studies on MM trauma.
Conclusion
The majority of the subjects sustaining MM fractures in KSA were young adult males. The leading etiology of trauma was MVAs and the most common fracture site was in the mandible. KSA is showing a great shift in its motor-vehicle safety regulations and social structure however medical studies lag behind recently published non-medical reports on the same topic. Future studies using nationwide registry would enable rigorous reporting of the outcomes and detection of any changes in epidemiological trends of MM trauma in the KSA and globally.
References
- https://www.who.int/
- Jamal A, Rahman MT, Al-Ahmadi HM, et al. The dilemma of road safety in the eastern province of Saudi Arabia: Consequences and prevention strategies. Int J Environ Res Public Health 2020; 17.
- Abdullah WA, Al-Mutairi K, Al-Ali Y, et al. Patterns and etiology of maxillofacial fractures in riyadh city, Saudi Arabia. Saudi Dent J 2013; 25:33-38.
- AlQahtani FA, Bishawi K, Jaber M. Analysis of the pattern of maxillofacial injuries in Saudi Arabia: A systematic review. Saudi Dent J 2020; 32:61-67.
- Lo CK, Mertz D, Loeb M. Newcastle-ottawa scale: Comparing reviewers’ to authors’ assessments. BMC Med Res Method 2014; 14:45.
- Alanazi YM, Latif K, Alrwuili MR, et al. Incidence of maxillofacial injuries reported in Al-Qurayyat general hospital over a period of 3 years. Prensa Med Argent 2016; 102:1-4.
- AlHammad Z, Nusair Y, Alotaibi S, et al. A cross-sectional study of the prevalence and severity of maxillofacial fractures resulting from motor vehicle accidents in Riyadh, Saudi Arabia. Saudi Dent J 2020; 32:314-320.
- Shalhoub SY. An overview of industrial accidents with particular reference to facial trauma. Aust Dent J 1991; 36:445-450.
- Aldwsari OM, Aldosari KH, Alzahrani MK, et al. Associated head injuries and survival rate of patients with maxillofacial fractures in road traffic accident: A prospective study in Saudi Arabia. J Family Med Prim Care 2018; 7:1548-1554.
- Arfaj A. Closed reduction of pediatric nasal bone fractures. J Kuwait Med Assoc 2015; 47:321-324.
- Ali-Alsuliman D, Ibrahim EH, Braimah RO. Patterns of zygomatic complex bone fracture in Saudi Arabia. J Emerg Trauma Shock 2018; 11:170-174.
- Brown RD, Cowpe JG. Patterns of maxillofacial trauma in two different cultures. A comparison between Riyadh and Tayside. J R Coll Surg Edinb 1985; 30:299-302.
- Nwoku AL, Oluyadi BA. Retrospective analysis of 1206 maxillofacial fractures in an urban saudi hospital: 8 year review. Pakistan Oral Dent J 2004; 13-16.
- Almasri M, Amin D, F AboOla, et al. Maxillofacial fractures in Makka city in Saudi Arabia: An 8-year review of practice. Am J Public Health Res 2015; 3:56-59.
- Albeshir H, Ahmed S, Awaji M, et al. Pediatric maxillofacial injuries in Madinah-a retrospective study. J Public Health Policy Plann 2018; 2:73-80.
- Samman M, Ahmed SW, Beshir H, et al. Incidence and pattern of mandible fractures in the madinah region: A retrospective study. J Nat Sci Biol Med 2018; 9:59-64.
- Rabi AG, Khateery SM. Maxillofacial trauma in Al Madina region of Saudi Arabia: A 5-year retrospective study. Asian J Oral Maxillofac Surg 2002; 14:10-14.
- Jan A, Alsehaimy M, Al-Sebaei M, et al. A retrospective study of the epidemiology of maxillofacial trauma in Jeddah, Saudi Arabia. J Am Sci 2015; 11:57-61.
- Almasri M. Severity and causality of maxillofacial trauma in the southern region of Saudi Arabia. Saudi Dent J 2013; 25:107-110.
- Lawoyin TO, Lawoyin DO, Lawoyin JO. Factors associated with oro-facial injuries among children in Al-Baha, Saudi Arabia. Afr J Med Med Sci 2002; 31:37-40.
- Al-Bokhamseen M, Salma R, Al-Bodbaij M. Patterns of maxillofacial fractures in Hofuf, Saudi Arabia: A 10-year retrospective case series. Saudi Dent J 2019; 31:129-136.
- Alqahtani AM. Patterns of maxillofacial fractures associated with assault injury in Khamis Mushait city and related factors. EJHM 2018; 70:289-292.
- Lawoyin DO, Lawoyin JO, Lawoyin TO. Fractures of the facial skeleton in Tabuk North West armed forces hospital: A five year review. Afr J Med Med Sci 1996; 25:385-387.
- Long S, Spielman DB, Losenegger T, et al. Patterns of facial fractures in a major metropolitan level 1 trauma center: A 10-year experience. Laryngoscope 2021; 131:E2176-E2180.
- Boffano P, Roccia F, Zavattero E, et al. Assault-related maxillofacial injuries: The results from the European maxillofacial trauma (EURMAT) multicenter and prospective collaboration. Oral Surg Oral Med Oral Pathol Oral Radiol 2015; 119:385-391.
- Xiao-Dong L, Qiu-Xu W, Wei-Xian L. Epidemiological pattern of maxillofacial fractures in northern china: A retrospective study of 829 cases. Medicine 2020; 99:e19299.
- Samieirad S, Tohidi E, Shahidi-Payam A, et al. Retrospective study maxillofacial fractures epidemiology and treatment plans in southeast of Iran. Med Oral Patol Oral Cirugía Bucal 2015; 20:e729-e736.
- Martins MMS, Homsi N, Pereira CCS, et al. Epidemiologic evaluation of mandibular fractures in the Rio De Janeiro high-complexity hospital. J Craniofac Surg 2011; 22:2026-2030.
- Alsenani M, Alaklobi A, Ford J, et al. Comparison of trauma management between two major trauma services in Riyadh, Kingdom of Saudi Arabia and Melbourne, Australia. BMJ Open 2021; 11:e045902.
- Kyrgidis A, Koloutsos G, Kommata A, et al. Incidence, aetiology, treatment outcome and complications of maxillofacial fractures. A retrospective study from Northern Greece. J Cranio-Maxillofac Surg 2013; 41:637-643.
- Brasileiro BF, Passeri LA. Epidemiological analysis of maxillofacial fractures in Brazil: A 5-year prospective study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006; 102:28-34.
- Cabalag MS, Wasiak J, Andrew NE, et al. Epidemiology and management of maxillofacial fractures in an Australian trauma centre. J Plast Reconstr Aesthet Surg 2014; 67:183-189.
- Boffano P, Kommers SC, Karagozoglu KH, et al. Aetiology of maxillofacial fractures: A review of published studies during the last 30 years. Br J Oral Maxillofac Surg 2014; 52:901-906.
- Juncar M, Tent PA, Juncar RI, et al. An epidemiological analysis of maxillofacial fractures: A 10-year cross-sectional cohort retrospective study of 1007 patients. BMC Oral Health 2021; 21:128.
- Suliman A, Ebaa J, Wedyan A, et al. The prevalence of head and facial injuries among children in Saudi Arabia following road traffic crashes. Ann Saudi Med 2020; 40:417-424.
- https://data.gov.sa
- Algahtany MA. Secular trend, seasonal variation, epidemiological pattern, and outcome of traumatic head injuries due to road traffic accidents in Aseer, Saudi Arabia. Int J Environ Res Public Health 2021; 18:12.
- https://www.vision2030.gov.sa
- Daniels JS, Albakry I, Braimah RO, et al. Maxillofacial bone fractures in children and adolescents: Overview of 247 cases in a major referral hospital, Najran, Kingdom of Saudi Arabia. Craniomaxillofac Trauma Reconstr 2021; 14:126-134.
- Lalloo R, Lucchesi LR, Bisignano C, et al. Epidemiology of facial fractures: Incidence, prevalence and years lived with disability estimates from the global burden of disease 2017 study. Inj Prev 2020; 26:i27-i35.
- Cunningham LL, Haug RH, Ford J. Firearm injuries to the maxillofacial region: An overview of current thoughts regarding demographics, pathophysiology, and management. J Oral Maxillofac Surg 2003; 61:932-942.
- Ford JE, Alqahtani AS, Abuzinada SAA, et al. Experience gained from the implementation of the Saudi TraumA registry (STAR). BMC Health Services Res 2020; 20:18.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at Google Scholar Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Noura Alsufyani1,2*, Rabab Bukhamseen3 and Majd Qadoumi3
1Department of Oral & Maxillofacial Radiology, Oral Medicine and Diagnostic Sciences, College of Dentistry, King saud university, Riyadh, Kingdom of Saudi Arabia2Department of Medicine and Dentistry, University of Alberta, Canada
3Dental University Hospital, King Saud University, Riyadh, Kingdom of Saudi Arabia
Citation: Noura Alsufyani, Rabab Bukhamseen, Majd Qadoumi,Causes and Patterns of Traumatic Mandibular and Maxillofacial Fractures in Saudi Arabia: Systematic Review and Meta-Analysis, J Res Med Dent Sci, 2022, 10(1): 237-245
Received: 17-Dec-2021, Manuscript No. JRMDS-21-47721; , Pre QC No. JRMDS-21-47721 (PQ); Editor assigned: 20-Dec-2021, Pre QC No. JRMDS-21-47721 (PQ); Reviewed: 03-Jan-2022, QC No. JRMDS-21-47721; Revised: 06-Jan-2022, Manuscript No. JRMDS-21-47721 (R); Published: 13-Jan-2022
