Review Article - (2022) Volume 10, Issue 11
Choice of Matrix System in Dentistry
Vaishnavi Rajendra Patekar*, Nikhil Mankar, Karuna Burde and Aparna Achanta
*Correspondence: Dr. Vaishnavi Rajendra Patekar, Department of Conservative and Endodontics, Sharad Pawar Dental College and Hospital, Datta Meghe Institute of Medical Sciences (Deemed to be University), Wardha, Maharashtra, India, Email:
Abstract
A fundamental goal of the dental practitioner is to restore surface cavities and replace tooth structure that has been lost due to caries, trauma, or decay, injury, and other causes to "normal" anatomical specifications. Cognitive interpretation of tooth morphology achieved with appropriate materials and resources, as well as the required psychomotor skills for proper design and completion, are regarded as critical restoration strategies. Furthermore, if present, the original tooth structure visualization should greatly assist the dentist in creating a clinically acceptable restoration. Form and function are concepts that must be understood as they relate in the oral realm, as well as a result of inadequate restorative dental care will be investigated. The matrix system is utilised to offer shape and contour to the restoration as well as to maintain form throughout placement and setting of the restoration. This page provides a brief overview of the restoration matrixes and procedures, as well as their current position in endodontic treatment.
Keywords
Matrix system, Matrix band, Restoration, Proximal surfaces
Introduction
Matrixing is a procedure that involves the formation of a short term wall contrary to the axial walls, encircling a tooth structure region that has been lost during the procedure. A dental matrix is a type of band that adheres to the surface of the to be restored tooth, replicating its anatomical features, while the repair is being completed, the lost walls will be replaced, thereby converting compound cavity into a straight forward cavity for quick repair. A matrix primarily is used when a proximal surface is to be restored.
The dentist has a lot of options when it comes to procedures and materials when treating missing tooth structures. Reconstruction of lost tooth structure caused by caries, injury, abrasion, erosion, attrition, or a combination of factors has long been a source of concern. There are benefits and drawbacks to both direct and indirect restorative methods. The reestablishment of optimal both form and function related with tooth anatomy on the proximal surface has presented several challenges in each case. Consequently, the periodontal apparatus is directly influenced in terms of protection and stimulation is brought back to origin. Visualization of the surviving tooth structure, thorough understanding of tooth anatomy, is required for effective odontogenic recovery [1-4].
Demand for cosmetic repair and a minimally invasive restorative technique are increasing. The usage of resin composite for posterior carious lesion repair has increased as a result of this. During the operation, the key issue is to restore an intact proximal surface, particularly good interproximal connections. A good matrix system offers a slew of advantages. Plane region where the locations of the proximal faces that are adjacent to each other come into contact is referred to as a "proximal contact.” Dentition support, arrangement and balance as well as care of interdental gingival papilla to avoid food impingement also development of approximate tooth decay, are all functions of a good (tight) proximal contact surface. The establishment of these criteria guarantees that the oral tissues are adequately protected and stimulated, resulting in an oral cavity having good health [5]. Contact is either absent or open, as well as planes of proximal contact having improper measurements, can lead to misaligned teeth and shift which can lead to food impaction, halitosis, caries formation, and periodontal disease [6-8].
Literature Review
During the restorative process, they isolate one tooth from another and contain composite material. Matrix methods assist build adequate interproximal contacts, shape, and keep flash at bay by forming a wall on the surface of a tooth where none previously existed. This not only saves practitioners time, but also protects patients from the risk of sub gingival irritation. Dental matrices, helps formation of interproximal planes with quick recovery have gained fame as dental composites have improved. There are many distinct sorts of matrices, sectional matrix systems, matrix bands, and other configurations are available, they intended and to be put between the repaired tooth and the neighbouring teeth, form the restorative materials outside shape.
Modern dentistry depend on tripartite method of restorative care that includes viewpoints such as enhancing tooth shape and basis, preserving dental building with little interference, and restoring teeth to their original state. Improvement in "aesthetic" technology proficiency and matter sciences they separate one tooth from another and contain composite material during the restorative process. By creating a wall on the surface of a tooth where none exists, matrix systems help to form proper interproximal contacts, help shape restorations, and keep flash at bay which not only saves clinicians clean up time, but also saves patients from the potential for sub gingival irritation [9].
Food impaction and associated periodontal disease can be avoided with a properly reconstructed proximal surface that considers both anatomical and obstructive considerations. Correctly implemented principles of contemporary, evidence based techniques are used to stimulate tissues of the mouth and stabilize the teeth within an arch and the obstructive close up [10]. Anatomically accurate contoured restorations that allow for the preservation of functional functions depend on tried resources, armoury, and methods in current restorative dentistry. The degree of constraint and location of point at which adjacent teeth come into contact, as well as shape of the proximal planes, are important element in periodontal tissue strength [11]. The contact power is affected by a variety of elements such as tooth kind and position, alteration in positions, periodontal disease of the tooth, and individual variability [12].
Three things are required of a matrix system
• Recreate the natural tooth form and interproximal contact.
• Seal the prep's proximal and gingival walls.
• Get around the band's thickness.
Any system that meets these three criteria will be successful.
Characteristics of dental matrixes
• Rigidity
• Minimal thickness
• Flexibility
• Compatibility
• Stability
• Optimal transmittance
Matrix retainer
Depending upon the mode of retention
• With retainer-ivory no.1, ivory no.8
• Without retainer-auto matrix
Depending on the cavity preparation for which it is used
• Class I cavity with buccal and lingual extension- Double banded tofflemire.
• Class II cavity single banded tofflemire, ivory no.1, ivory no.8, copper band matrix, T band matrix, and pre countered sectional matrix.
• For other type’s cavity preparations-Auto matrix, clear plastic matrix.
Tofflemire universal matrix band retainer
Also known as universal matrix. A Tofflemire matrix system results in which a temporary wall is constructed on the opposite side of the axial partitions to build up the tooth structure around the missing portions during preparations. Tofflemire or universal matrix system is a metallic circumferential type of matrix that provides a good barrier in class II restorations.
Functions of tofflemire matrix systems
• Create a temporary barrier to the pressure required for the restoration.
• Give the restoration some shape and contour.
• Form preservation during the placement and setting of the repair (amalgam or composite) (Figure 1).

Figure 1: Tofflemire universal matrix system.
Indications
• Mesiooccluso distocavity construction of posterior teeth.
• Only mesioocclusal/distoocclusal class II recovery.
Types of tofflemire matrix
• Straight: Buccal positioned
• Contra angled: can be put lingual as well
Advantages
• When the retainer and band are properly secured, they are more stable.
• The retainer from the band may be readily separated, allowing for easy removal from the band.
• It takes less time to place the item.
• Assist with maintaining the cotton roll's position.
Disadvantages
• When restoring utilize the matrix to create proximate surfaces, more sculpting is required as compared while using complex supported matrix.
• Matrix band outline is necessary.
• Does not produce the best outcomes with resin restorations.
Ivory matrix no. 1
A stainless steel band is wrapped around one proximal surface of a posterior tooth. A wedge shaped protrusion on the retainer connects this to the retainer. The band is adapted to the prepared tooth's proximal shape via an adjustment screw at the retainer's end. For unilateral class II tooth preparations, ivory matrix holder no.1 is the widely used. The matrix holder has two arms in the shape of a semicircle with slanted positions at one arm and a claw at the other. There's a screw in the opposite direction of the matrix band holder that, when tightened, draws the claws' ends closer together. One of the margins in the middle of the band used with this matrix is slightly projected. On the side of tooth preparation, this anticipated margin is kept in the direction of gingiva. Appropriate size band is picked out and ringed close to the tooth. The retainer's screw is tightened while the matrix band is kept around the tooth, ensuring fitting of band exactly close to the tooth. Following this, a wedge is used to help the matrix band fit more snugly around the tooth (Figure 2).
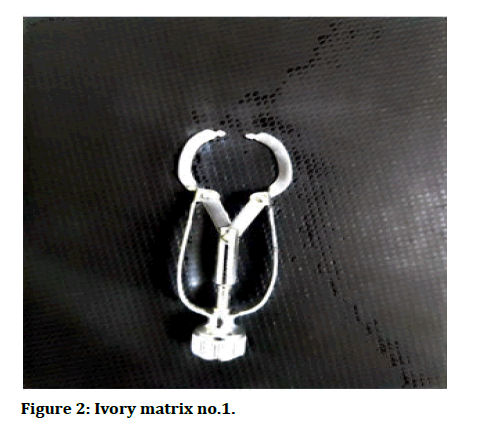
Figure 2: Ivory matrix no.1.
Indications: For the repair of class II cavities, particularly when the contact on the unprepared side is quite limited.
Ivory matrix no.8
The ivory matrix band retainer secures the matrix band, which encircles the teeth and fills in the gaps on both proximal sides. The matrix band is constructed of a thin sheet of metal for easy passage through the contact region of the tooth's unprotected proximal side. The band's outline may be modified using the screw included with the matrix band retainer (Figure 3).
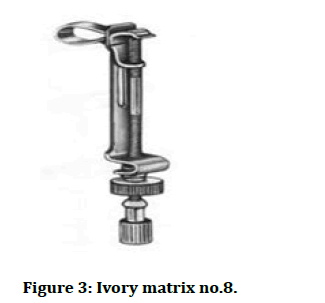
Figure 3: Ivory matrix no.8.
Indications
• Class II preparations can be done unilaterally and bilaterally (MOD)
• Class II complex tooth preparations with more than two missing partitions
Advantages of ivory matrix system
• Economical
• Class II tooth preparations are restored with this material
• Can be purify
Disadvantages of ivory matrix system
• Difficult to put on and take of
Auto matrix
The auto matrix technology enables matrix positioning and maintenance without the usage of bulky retainers, resulting in easier placement, improved access, a clearer perspective on the operative field, increased patient satisfaction. The circumferential auto matrix system bands, which are only used once, enable proper sub gingival and proximal adaptation (Figure 4).
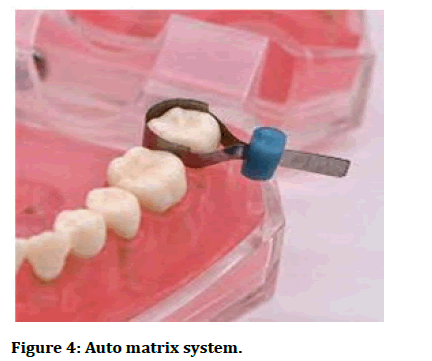
Figure 4: Auto matrix system.
Indications: When one or more cusps need to be changed in a complex amalgam restoration.
Advantages
• It is simple to use due to the lack of interference from a retainer, visibility has improved
• Quick implementation
Disadvantages
• Because the bands are not pre-contoured, proximal contouring is challenging
• Expensive
Copper bands
A continuous band is recommended for MOD and sophisticated restorations. It can be retained till the restorations are completed. Amalgam fillings with more than two surfaces are commonly used.
Indications
• For severely decayed teeth, particularly those requiring pin amalgam restorations
• If you have a complicated condition, such as a class II cavity with a big buccal or lingual extension
Advantages: It provide excellent contour
Disadvantages: Time consuming
Pre-countered matrix strips: Pre contoured matrix strips, such as the palodent and Darvag, are now widely available.
Prefabricated plastic matrices
• Available in a variety of sizes
• A handle is included to help keep the matrix in place while the material cures
• It's best to use with light cure restorations
Discussion
Sectional matrix
Proximal caries is one of the most common pathologies we see in our everyday restorative treatment. It is critical to restore the class II cavities properly as well as to achieve a functioning associated surface in the middle of teeth. In two planes class II cavities, the sectional matrix system produces statistically substantially proximal connections are more tightly packed than in the circumferential matrix system. When class II composite resin restorations marginal ridge fracture strength having a matrix band that is either straight or curved employing composite resins is compared, the ridge at the edge of a class II composite resin restoration used in conjunction along contoured matrix band has a stronger marginal ridge.
It is critical to have a decent tooth preparation in order to use this matrix properly and achieve a satisfactory result. Because the matrix must be applied passively, it is usually required to arrange the preparation margin outside the contact site, in a safer and easier to clean zone. Otherwise, the matrix will always be at risk of deformation. We can get a pretty good shape if the matrix is put passively. Another requirement for a suitable contact surface is a space within the mouth to make up for the matrix width and composite polymerization shrinkage. The majority of important tools for this purpose are separation rings. If the gingival edge of the preparation is not too sub gingival, powerful stiff wedges can be used to achieve tooth separation.
Using modern rings, matrix, and wedge technologies, a sectional matrix system provides easy, predictable, and accurate contact formation. It has precise junction and a close fitting marginal seal, minimal overhang and final touches, is simple to install and remove (Figure 5).
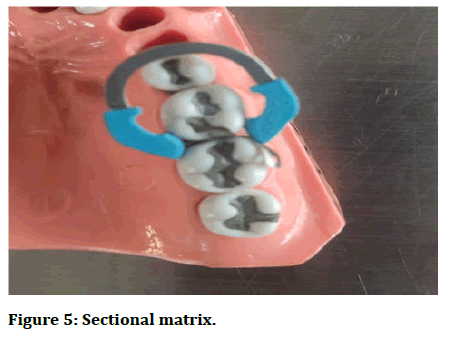
Figure 5: Sectional matrix.
Example: Palodent, garrison, dentsply
Indications
• For minor to average class II cavities affecting one or both proximal surfaces of backside tooth
• This applies to both amalgam and composite materials restorations
Advantages
• It's simple to use and has a lot of visibility
• The bands' anatomical contour ensures ideal contact points and indentation
• Appropriate functional proportions and anatomical site is correct
Disadvantages
• Matrix bands can easily dent, particularly when continuity of beside dentition is very close, obstruct the band from being inserted easily
Circumferential matrix system palodent 360
• Palodent 360 matrix bands can be put in a variety of configurations to address field of view, tooth structure loss, and instrument accessibility. Palodent 360 is a ground breaking innovative circumferential matrix system. Without the need of an inconvenient retainer or applicator, tight contacts with anatomically natural curves can be achieved with just a twist of your fingers.
• The integrated lightener/retainer allows for matrix placement and retention without the use of bulky retainers or accessory placement and lightener instruments, resulting in increased efficiency (no set up required), ease of placement, better access, a clearer view of the operating field, and patient comfort.
• For superior restorations that are quicker and easier than you ever imagined. The cycle of success is complete (Figure 6).
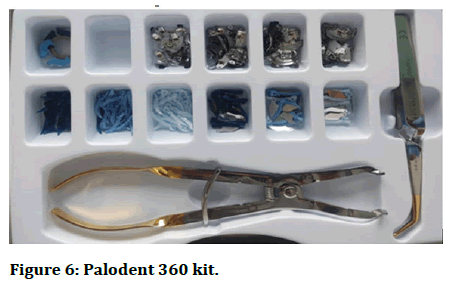
Figure 6: Palodent 360 kit.
Indications
• Palodent 360 circumferential matrix bands can be used for all class II restorations, but they are particularly beneficial in challenging class II cases when there is no next tooth, too much dental structure is lost to use a sectional matrix, or a misaligned or severely rotated tooth
• Palodent 360 matrix bands work with palodent plus retention rings, which can be utilized to gain temporary space in interproximal gaps. They can be used with palodent plus wedges for a better fit
Advantages
• System that is simple to utilize
• Natural looking curves
• Contact point that is tight and anatomically accurate
• Interproximal finishing is kept to a bare minimum
Wedges and wedging
• A wedge is a piece of wood, metal, or other material with a sharply angled border created by double covering surfaces that is used to tighten or impart tension in a variety of ways.
• Nowadays, a wedge is frequently used in conjunction with matrices for the purpose of putting plastic restoration materials in.
• Wedges, when properly selected and applied, can make a significant contribution to the initial quality and longevity of some restorations, as well as greatly simplifying a variety of clinical procedures (Figure 7) [13].
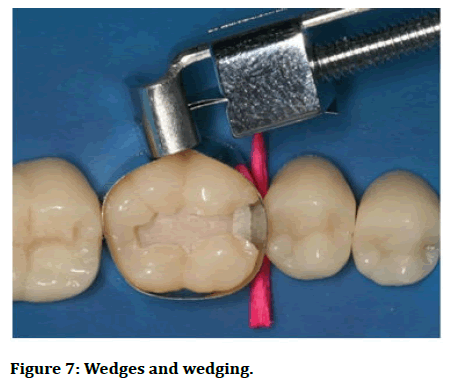
Figure 7: Wedges and wedging.
Functions of wedges
• Prevents gingival extrusion of restorative material
• Defines gingival range of contact area
• Creates partition to make up for band thickness
• A traumatic retraction of rubber dam along with gingiva
Piggy back wedging
• When the wedge is substantially high to the gingival border, a smaller wedge is piggybacked in addition to the first
• This approach is useful in patients with interproximal tissue level recession
Double wedging: For wide proximal restorations, two wedges were employed, one from the lingual and the other from the face embrasure.
Wedge wedging: A second sharpened wedge is kept between the first and second wedges and the band if there is a concavity on the proximal surface [14-18].
Conclusion
The major goal of operative dentistry is to safeguard the tissue and maintain the health of the teeth. The goal of a restoration is to rebuild missing tooth structure while also providing sufficient strength and protection for the pulp against external shocks. The sciences of restorative technology has advanced due to advancements in material formulations, refinements in insertion techniques and arm a mentarium, and the gradual replacement of missing tooth structures with appropriate materials and resources. The occlusion of the matrix band to the remaining healthy tooth structure of the gingival cavo surface line angle should be achieved solely by the correct application of the wedges; the effect of the wedges on the proximal contour and prior to inserting the restorative material, the contact area should be thoroughly readdress; various sizes and forms of wedges, as well as a cutting tool to cut, should be freely accessible. When paired with a contact matrix separation ring, the use of circumferential matrices or sectional pliable matrices result in small marginal extends. The use of more traditional restorative methods may result in clinical failure and a reduction in the durability of these repairs. As a result of the challenges inherent in placement, innovative advances in matrix system technology, changes in matrix plan and interdental separation procedures, have evolved. The advancements have enabled dentists in order to produce the best proximal contact surfaces and anatomically accurate shapes, which are critical for best dentition shape and purpose, as well as activation and defence of the periodontal complex. The occlusion of the matrix band to the remaining living tooth planes of the gingival cavo surface line angle should be accomplished entirely by the proper placement of the wedges.
References
- Zarean P, Roozbeh R, Zarean P, et al. In vitro comparison of shear bond strength of a flow able composite resin and a single component glass ionomer to three different pulp capping agents. Dent Med Probl 2019; 56:239-244.
- Loomans BA, Opdam NJ, Roeters FJ, et al. Comparison of proximal contacts of class II resin composite restorations in vitro. Oper dent 2006; 31:688-693.
- Raghu R, Srinivasan R. Optimizing tooth form with direct posterior composite restorations. J Conserv Dent 2011; 14:330.
- Nelson SJ. Wheeler's Dental Anatomy, Physiology and Occlusion: 1st Edition Sae-E-Book. Elsevier India, 2015.
- Eissmann HF, Radke RA, Noble WH. Physiologic design criteria for fixed dental restorations. Dent Clin North Am 1971; 15:543-568.
- Keogh TP, Bertolotti RL. Creating tight, anatomically correct interproximal contacts. Dent Clin North Am 2001; 45:83-102.
- Koral SM, Howell TH, Jeffcoat MK. Alveolar bone loss due to open interproximal contacts in periodontal disease. J Periodontol 1981; 52:447-450.
- Kampouropoulos D, Paximada C, Loukidis M, et al. The influence of matrix type on the proximal contact in Class II resin composite restorations. Oper Dent 2010; 35:454-462.
- Ferracane, Jack. Resin composite state of the art. Dent Mat 2011; 27:29-38.
- Staehle HJ. Minimally invasive restorative treatment. J Adhes Dent 1999; 1:267-284.
- Kampouropoulos D, Paximada C, Loukidis M, et al. The influence of matrix type on the proximal contact in Class II resin composite restorations. Oper dent 2010; 35:454-462.
- Qualtrough AJ, Wilson NH. The history, development and use of interproximal wedges in clinical practice. Dent Update 1991; 18:66-70
- Klein F, Keller AK, Staehle HJ, et al. Proximal contact formation with different restorative materials and techniques. Am J Dent 2002; 15:232-235.
[Googlescholar][Indexed].
- Chandak PG, Ghanshyamdasj M, Chandak C, et al. Nanoparticles in endodontic-A Review. J Evol Med Dent Sci 2021; 10:976-982.
[Crossref]
- Chandak M, Rathi C, Madhulika, et al. Pushout bond strength of MTA as root canal sealer: A systematic review. J Clin Diag Res 2020; 14:ZE01-ZE04.
[Crossref]
- Chandak M, Rathi C, Madhulika, et al. Comparative evaluation of micro leakage of three different sealers using vertical compaction technique under stereomicroscope: An in vitro study. Med Sci 2020; 24:2067-2073.
- Chandak MS, Chandak M, Nikhade PP, et al. Role of liners in restorative dentistry. J Evo Med Dent Sci 2020; 9:1881-1886.
[Crossref]
- Eli I, Weiss E, Kozlovsky A, et al. Wedges in restorative dentistry: principles and applications. J Oral Rehabil 1991; 18:257-264.
Author Info
Vaishnavi Rajendra Patekar*, Nikhil Mankar, Karuna Burde and Aparna Achanta
Department of Conservative and Endodontics, Sharad Pawar Dental College and Hospital, Datta Meghe Institute of Medical Sciences (Deemed to be University), Wardha, Maharashtra, IndiaCitation: Vaishnavi Rajendra Patekar, Nikhil Mankar, Karuna Burde, Aparna Achanta. Choice of Matrix System in Dentistry, J Res Med Dent Sci, 2022, 10 (11): 120-126.
Received: 12-Sep-2022, Manuscript No. JRMDS-22-49497; , Pre QC No. JRMDS-22-49497(PQ); Editor assigned: 14-Sep-2022, Pre QC No. JRMDS-22-49497(PQ); Reviewed: 28-Sep-2022, QC No. JRMDS-22-49497; Revised: 15-Nov-2022, Manuscript No. JRMDS-22-49497(R); Published: 28-Nov-2022
