Research Article - (2021) Volume 9, Issue 12
Clinicopathological Study of Granular Cell Tumors: A 4 Year Retrospective Study from a Tertiary Care Centre in Kerala
*Correspondence: Rajasree varma, Department of Pathology, Government Medical College, Kozhikode, Kerala, India, Email:
Abstract
Background: Granular cell tumor is a rare, mostly benign neoplasm, which can affect a variety of body sites. The cell of origin is considered to be Schwann cells. Granular cell tumors can affect all ages and both genders, but it is classically found in middle aged females. They may be detected incidentally or may present as small solitary painless nodules. Most granular cell tumors behave indolently. However, they may pose diagnostic difficulties when they mimic malignancy radiologically and clinically. A minority of these lesions can be malignant and have worse prognosis. These malignant granular cell tumors can be diagnosed histopathologically or by identifying metastasis. Histopathological examination is the gold standard method for diagnosing the lesion and assessing malignant transformation in granular cell tumors.
Methods: This was a retrospective study done in the Department of Pathology, Govt. Medical College, Kozhikode during for a period of 4 years. The study subjects included all patients diagnosed as granular cell tumor in the Department of Pathology during this time period. Clinical details and histopathological features were assessed.
Results: A total of 38 subjects were included in this study. Mean age of the subject was 34.7 years. Majority of subjects were females. Most common site of the lesion was arm. Majority of lesions had conventional morphology. No malignant granular cell tumors were identified. The lesions were positive for S-100.
Conclusions: Granular cell tumors are mostly benign in nature. They can also mimic other malignancies clinically and radiologically. The gold standard method for assessing malignant changes in granular cell tumor is by histopathological examination. This study focusses on assessing clinical and histopathological assessment of granular cell tumors.
Keywords
Schwann cells, Arm, Female, Conventional, Benign, S100Background
Granular cell tumor is a rare tumor, which is mostly benign and can affect any organ in the body. It most commonly occurs in skin and soft tissue. Other organs commonly affected are tongue and breast and have very rarely been reported in the digestive and respiratory tracts, heart, pelvis, bladder and vulva. It can occur in both sexes, although a female predisposition is more common. Clinical presentation is variable and often depends on the location of the lesion. These lesions usually present as a skin coloured or reddish, solitary, non-tender, slow growing nodules. Many cases are detected incidentally. In visceral organs, these tumors can cause symptoms due to pressure effects on vital organs. Clinically granular cell tumors mimic neurofibroma, schwannoma, fibromas and lipomas.
Granular cell tumors were initially thought to have a muscular origin. These tumors are proposed to be originating from the Schwann cells. The typical histo-morphological features are diagnostic and when required can be supplemented with immunohistochemical markers. Majority of these tumors are positive for S-100. Many syndromic associations have been proposed, which includes Noonan’s syndrome and LEOPARD syndrome, PTEN hamartoma tumor syndrome and type 1 neurofibromatosis. A small subset of S-100 negative granular cell tumors (non-neural dermal granular cell tumors) have been identified and were found to harbour mutation in ALK fusion gene. However they are found to be consistently positive for NK1-C3 and are usually found to have a better prognosis.
Majority of granular cell tumors are benign and do not recur, unless excision is incomplete. Malignant granular cell tumors, however have a poor prognosis, has propensity for distant metastasis and is associated with reduced survival. Large tumor size, deep soft tissue location, necrosis, and distant metastasis are features commonly seen with its malignant counterpart.
The significance of identifying these tumors is that they can mimic cutaneous and mucosal malignancies. Moreover, identification of malignant granular cell tumors is very important. Hence proper diagnosis of the lesion using histopathology and immunohistochemical techniques is essential for identifying the malignant granular cell tumors and for excluding other mimickers of these lesions.
Objective
To describe the clinical and histo-morphological patterns of granular cell tumors.
Methods
LThis was a retrospective study done in the Department of Pathology, Govt. Medical College, Kozhikode during the time period of Jan 2013 to May 2017. Convenient sampling was employed and the study subjects included all patients diagnosed as granular cell tumor in the Department of Pathology during this time period. All the cases in which slides or blocks could not be retrieved were excluded from the study.
The case sheets and slides of all diagnosed patients were retrieved. Formalin fixed paraffin embedded blocks were studied and Hematoxylin & Eosin staining were done for the study. The cases were studied for age, sex, site of lesion, duration of lesion, size of tumor, invasion, mitosis, necrosis and atypical nuclear features. IHC staining for S100 was done for confirmation.
Data analysis
The data was entered in the spread sheets of Microsoft Office Excel and the variables were analysed using standard analytic techniques with SPSS version 16.0 for Windows. The results were tabulated and analyzed statistically. The quantitative variables were expressed as mean and qualitative variables were expressed as percentages.
Results
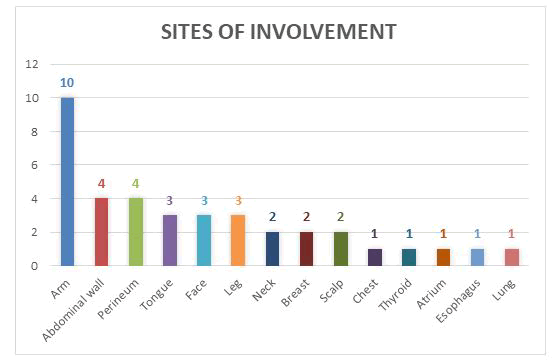
In this study, a total of 38 subjects were included. The subjects had an age range from new born to 74 years, with a mean age of 34.7 years (SE- 3.17). Majority of subjects belonged to the age group of 40 to 50 years. Of all the study subjects, 25 (65.8%) were females and 13 (34.2%) were males. The most common site of the lesion was arm, seen in 10 subjects (26%). This was followed by followed by abdominal wall (10.5%), perineum (10.5%), tongue (7.9%) and face (7.9%). The other sites of involvement are illustrated in Fig-1
Figure 1: Sites of involvement of the tumor (n=38).
Duration of lesion varied from 3 months to 4 years. The size of lesions vary from 0.1 cm to 4 cms, with a mean size of 1.7 cms (SD- 0.89).
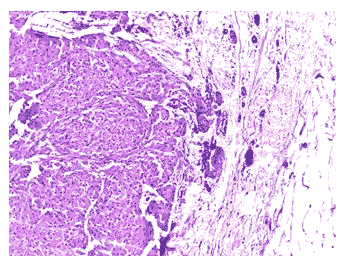
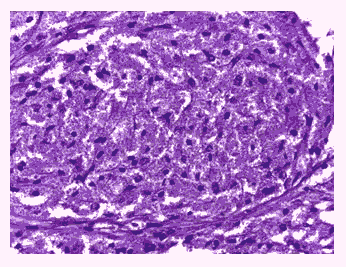
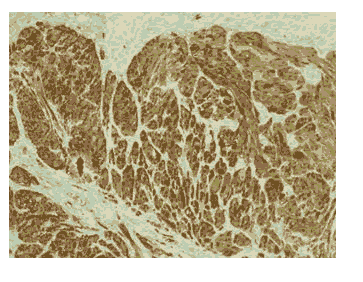
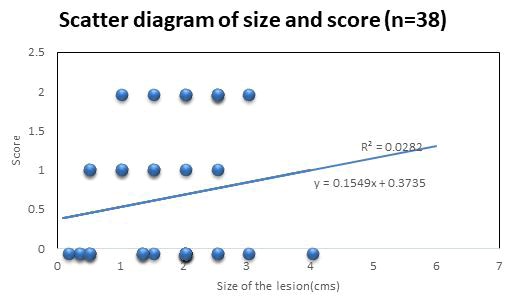
The histopathological features including mitotic activity, necrosis, invasion into adjacent normal structures and peritumoral lymphocytic infiltration are summarized in Table 1. Higher mitotic activity were seen only in 3 cases (7.9%) and all cases were females. 22 subjects (57.8%) had invasion into adjacent normal structures. Of these, 17 subjects (77%) were females. Necrosis was seen only in 2 cases (5.3%). The morphological features of the tumor cells were studied and is tabulated in Table 2. Predominant lesions (92%) had polygonal cells with typical eosinophilic granular cytoplasm and round nuclei (Fig 2 & 3). 3 subjects (8%) had a spindle cell morphology. These tumours showed PAS positive diastase resistant granules in the cytoplasm. Majority of cases showed only mild to moderate nuclear atypia. Severe cytological and nuclear atypia were not observed. Majority of tumors (65.8%) had hyperchromatic nuclei with no nucleoli. Others had vesicular nuclei with small to distinct nucleoli. Prominent nucleoli were not seen in any tumor. The tumors were positive for S100 by IHC (Fig-4). No lesions showed perineural or vascular invasion. Pseudoepitheliomatous hyperplasia was not seen. Each case was assessed for features of malignancy and was scored from 0-6 according to Fanburg- Smith criteria. 8 cases had a score of 2, 8 had a score of 1 and 22 cases had a score of 0. The score was studied for any association with size of the tumor. It was found that there was no significant linear association between size and malignant features (Fig-5) and correlation coefficient (r) =0.16 was obtained. No cases had sufficient findings to be classified as malignant granular cell tumor.
Table 1: Assessment of Histopathological findings (n=38).
| Histopathological feature | Present | Absent | ||
|---|---|---|---|---|
| Male | Female | Male | Female | |
| Mitosis (>/= 2/10 HPF) | 0 | 3 | 13 | 22 |
| Necrosis | 1 | 1 | 12 | 24 |
| Invasion | 5 | 17 | 8 | 8 |
| Lymphocytic infiltration | 1 | 5 | 12 | 20 |
Table 2: Assessment of cytological features (n=38).
| Features | Male | Female | |
|---|---|---|---|
| Tumor morphology | Conventional | 11 | 24 |
| Spindle | 2 | 1 | |
| Nuclear atypia | Minimal | 5 | 11 |
| Mild | 4 | 10 | |
| Moderate | 4 | 4 | |
| Nucleoli | Absent | 8 | 17 |
| Small indistinct | 1 | 3 | |
| Distinct | 4 | 5 |
Figure 2: Tumor shows a lesion composed of cells arranged as nests (H & E 100X).
Figure 3: Tumor shows tumor cells with abundant eosinophilic granular cytoplasm , oval vesicular nuclei (H & E 400X).
Figure 4: Tumor shows tumor cells which are diffusely positive for s-100 (IHC 100X).
Figure 5: Scatter diagram showing correlation of size of tumor with malignancy score.
Discussion
Granular cell tumors are very rare tumors and account for 0.5 % of all soft tissue tumors. These lesions were previously referred to as Abrikossof tumor and granular cell myofibroblastoma. They were initially believed to have a smooth muscle origin. However, immunohistochemical tests and ultrastructural studies have pointed to their origin from Schwann cells.
Granular cell tumors can occur anywhere in the body, but are most commonly seen in head and neck7, chest wall and arms. It is proposed that the higher frequency of these tumors in skin and tongue is due to the high concentration of peripheral nerves in these sites. The most common site of involvement in this study was arms (26.3%), followed by abdominal wall (10.5%), perineum (10.5%), tongue (7.9%) and face (7.9%). These tumors often present as painless slow growing nodules and are mostly seen in the subcutaneous tissue, sub-mucosal region or in deep soft tissues. They are usually asymptomatic,but can present with pressure effects on vital organs like bronchus and esophagus. They can also present as painful and pruritic plaque or nodule. The visceral tumors can also produce symptoms like hematuria and bleeding per rectum.
Granular cell tumors are most commonly seen in the age group of 4th to 6th decades, however, they may also occur in children. Studies done by Mobarki et al8 has also reported that the mean age of subjects was found to be 45.8 years. Similar results were also observed in this study, where the majority of subjects were in the age group of 40 to 50 years and the mean age of subjects was found to be 34.7 years.
Several studies have shown that these tumors were found to be more common in females9. However, studies done by An et al had shown male predominance in a study on 98 cases of granular cell tumors in GIT10. Singhi et al had demonstrated an equal distribution of cases in a study on colorectal granular cell tumors involving 26 subjects. In this study, two-thirds of the subjects were females.
Benign granular cell tumors are usually small and have a size less than 4 cm usually. In the study done by Dupuis et al on 130 cases, the size of the lesions ranged from 0.2 cm to 10 cms. The mean size of the lesion was 1.7 cms in this study, with a maximum size of 4 cms. Deeper lesions are often large and have yellow cut surface. According to Enzinger and Weiss, increased tumor size more than 5 cm is associated with poor prognosis, in addition to history of local recurrence and rapid recent growth.
No multifocal lesions were seen in this study, although in other studies approximately 5 to 16 % showed multiplicity. Multifocality is mainly described in association with a group of conditions termed RASopathies, which include Noonan syndrome, LEOPARD syndrome, Legius syndrome, Costello syndrome and type 1 neurofibromatosis. These genetic conditions are characterised by mutations in gene encoding Ras family proteins, which play pivotal role in cell proliferation and differentiation. Multiple granular cell tumors are usually common in skin and subcutaneous tissue. These may also be seen congenitally and can show a familial predisposition.
Granular cell tumors may have an infiltrative margin or may be circumscribed or well encapsulated lesion. In this study, infiltrative pattern was the predominant pattern and was found in 57.8 % of the cases. Studies done by Lack et al also demonstrated 43 % of cases with infiltration into normal tissue and positive resected margins. Infiltrative growth pattern cannot be used to differentiate benign and malignant granular cell tumors. Benign granular cell tumors also will not usually large areas of necrosis.
Classically granular cell tumors are composed of sheets, nests and cords of tumor cells separated by fibrous tissue. The tumor cells are mostly polygonal or rarely spindle in shape and have abundant granular eosinophilic cytoplasm and uniform hyperchromatic nuclei. Many tumors are also found to have large cytoplasmic granules surrounded by a clear halo and are named as Pustulo- ovoid bodies of Milian. Granularity of cytoplasm is due to accumulation of secondary lysosomes. The granules are PAS positive and diastase resistant.
Granular cells are also seen in a variety of tumors like rhabdomyoma, rhabdomyosarcoma, alveolar soft part sarcoma, granular cell dermatofibroma, granular ameloblastoma, paraganglioma, hibernoma and malignant peripheral nerve sheath tumor. Histopathological features, and ancillary tests like immunohistochemical tests and ultrastructural studies are necessary for proper diagnosis of the lesion.
As granular cell tumors are originated from Schwann cells, they are usually positive for S-100, vimentin, NSE and CD 68. They usually have low proliferative index, with Mib staining seen in <3%15. Proliferative markers like Ki67 and PHH3 were found to be a reliable predictors of atypical histology in some studies. Electron microscopy of granular cell tumors show intracytoplasmic dense membrane bound lysosomes.
A subset of granular cell tumors is negative for S-100 and is designated as non-neural granular cell tumors. These lesions are usually polypoid and are located in deep dermis. They lack pseudoepitheliomatous hyperplasia and often show attenuated ulcerated overlying epidermis. They are composed of spindle cells, round or polygonal cells with abundant granular cytoplasm. These lesions show cytologic atypia and increased mitotic activity.These tumors often show weak focal positivity for CD 68. The only consistent marker marker seen in this subset is NK1-C3 (CD 63)16. These lesions are usually indolent and have a good prognosis. Local recurrence can be seen and thus require complete excision. Some of these lesions were found to harbour a mutation in ALK fusion gene and so shows positivity for ALK by immunohistochemical techniques.
By histopathological examination, granular cell tumors can be categorized into benign, atypical and malignant subtypes. According to study done by Fanburg- Smith et al5, malignant granular cell tumors have at least three of the following six features- necrosis, spindling of tumor cells, vesicular nuclei with large nucleoli, increased mitotic rate (more than 2 /10 HPF), high nuclear to cytoplasmic ratio, and nuclear pleomorphism. Lesions with 1 or 2 of these features are considered as atypical granular cell tumors and those with none of these features are considered as benign granular cell tumors. Majority of granular cell tumors are benign, although some may be locally aggressive. Benign granular cell tumors have very good prognosis. Studies have shown that there is only very minimal chance of recurrence of these tumors after excision with wide margins17. However the chance of recurrence is higher, if the margins of excision are positive. Malignant granular cell tumors constitute only 2% of granular cell tumors18.They are more commonly seen in deep soft tissue, esophagus, larynx and peritoneal cavity. They have to be differentiated from other malignant soft tissue neoplasms including Alveolar soft part sarcoma, rhabdomyosarcoma, Dermatofibrosarcoma and melanoma. Malignant granular cell tumors have a poor prognosis, with local recurrence seen in 32% of cases and metastatic deposits seen in around 59% of cases5. Common sites of metastatic deposits were lymph nodes, lungs, liver and bones. Apart from Fanburg-Smith criteria, p53 upregulation and high Ki 67 values were also found to be associated with worse prognosis. In this study, majority of cases showed conventional polygonal cells with granular cytoplasm with minimal to mild nuclear pleomorphism and inconspicuous nucleoli. Spindle cells were found in a case each in breast, abdominal wall and perineum. Majority of cases had lower mitotic rate < 2/10 HPF. Higher mitotic rate was noticed only in 3 cases. Necrosis was seen only in 2 subjects. However, no cases had sufficient features to qualify as Malignant granular cell tumor.
15% of cases had tumor infiltrating lymphocytes, which indicates an immune response to tumor. This is lower than similar studies done by Stemm et al, who demonstrated tumor infiltrating lymphocytes in 35.3 % of cases. Lymphoid infiltrate were small, well circumscribed and had no germinal centre. No lesions showed perineural or vascular invasion. These can be seen even in benign granular cell tumors and have no impact in prognosis.
Pseudoepitheliomatous hyperplasia of overlying epithelium has been reported in 50-60% of cases in a study of laryngeal granular cell tumors21. This was also reported to be greater in oral, esophageal, perianal and laryngeal granular cell tumors22. Pseudoepitheliomatous hyperplasia is proposed to be due to interation of granular cells with the adjacent epithelial cells leading to basal cell proliferation. This can mimic Squamous cell carcinoma, especially in superficial biopsies. None of the cases in this study had pseudoepitheliomatous hyperplasia.
Radiological examination can also provide clues for identifying malignant granular cell tumors. Benign granular cell tumors are smaller in size and are usually hypo or isointense on T1 and T2 MRI. However, malignant granular cell tumors are larger and are often hyperintense on T2 MRI. They may also demonstrate perivascular invasion and often show infiltration into adjacent normal structures.
Fine needle aspiration cytology (FNAC) is often helpful in diagnosing these lesions. Cytology smears show clusters of histiocytoid cells with abundant granular eosinophilic cytoplasm, central round hyperchromatic nuclei. Some lesions may also have eccentric nuclei or fine vesicular nuclei with prominent nucleoli. Cytological atypia is often mild. The cytoplasm will show PAS positive Diastase resistant granules. In FNAC, the differential diagnosis includes histiocyte rich lesions, metastatic lesions, rhabdomyoma, epithelioid sarcoma and melanoma. Judicious use of immunocytochemical techniques is useful in diagnosing the disease.
In visceral organs, granular cell tumors can present as solid masses with infiltrative margins and ulcerated or thickened overlying mucosa and can masquerade as malignant neoplasms. The visceral lesions can also have a verrucous appearance due to pseudoepitheliomatous hyperplasia.
Benign granular cell tumors are treated by excision with a negative margin status. These usually donot recur, if the margins are negative. They also will not show lymph node or distant metastasis. Malignant granular cell tumors require wide local excision. Chemotherapy and or radiotherapy are often given for these cases. They usually have an aggressive course and a reduced overall survival.
Conclusion
Granular cell tumors are rare neoplasms with schwannian origin. They are more common in middle aged women and are common in arms and head and neck area. These lesions can occur in skin and subcutaneous tissue and visceral organs. The tumors can be sub classified into benign, atypical and malignant granular cell tumors according to Fanburg- Smith criteria. Additional factors which warn a poor prognosis are large size, high Ki67 and upregulation of P53. Majority of granular cell tumors are benign. However, even benign granular cell tumors can cause pseudoepitheliomatous hyperplasia and can mimic squamous cell carcinoma in superficial biopsies. Thus it is critical to identify these lesions to prevent overtreatment. Malignant granular cell tumors are rarer, and proper identification of malignant granular cell tumors is essential. Malignant granular cell tumors behave aggressively like Malignant peripheral nerve sheath tumors. They also have high rates of distant metastasis and overall low survival. So proper identification of granular cell tumors and assessing malignant changes in granular cell tumors is very important. In this study, no cases had sufficient features to qualify as Malignant granular cell tumor.
References
- Morrison, JG, Gray Jr GF, Dao AH, and Adkins Jr RB. "Granular cell tumors." Am surg53, (1987): 156-160.
- Ordóñez, Nelson G. "Granular cell tumor: a review and update."Adv Anat Pathol6, (1999): 186-203.
- rdóñez, Nelson G. "Granular cell tumor: a review and update."Adv Anat Pathol6, (1999): 186-203.
- Kamal, Syed Akhtar, and Othman Eyas Osama. "Granular cell tumour of the larynx." J Laryngol Otol112, (1998): 83-85.
- Garin, L, Barona R, Basterra J, Armengot M, and Alemany P, et al. "Granular cell tumor (Abrikossoff's tumor). A review and our experience."An otorrinolaringol ibero-am 19, (1992): 249-264.
Author Info
Department of Pathology, Government Medical College, Kozhikode, Kerala, IndiaCitation: Rajasree varma Clinicopathological Study of Granular Cell Tumors: A 4 Year Retrospective Study from a Tertiary Care Centre in Kerala, J Res Med Dent Sci, 2021, 9(11): 1-6
Received: 01-Dec-2021 Accepted: 15-Dec-2021 Published: 22-Dec-2021