Case Report - (2022) Volume 10, Issue 12
ECG in ICH
Abhilash Nair*, V Padma, Sandhya, Kannan Meera Devi, Saketh Ramineni and Sarath Bhaskar
*Correspondence: Dr. Abhilash Nair, Department of General Medicine, Sree Balaji Medical College and Hospital, Chrompet, India, Email:
Abstract
ECG or the poor man’s angiogram is generally used to look into cardiac electrical abnormalities. However, it has been found to be useful in various other abnormalities like in electrolyte disorders, pulmonary embolism, CNS diseases, oesophageal disorders, hypothermia, and drug-related and other conditions. Thus, knowledge of the characteristic changes in various conditions can be a matter of life and death for the patient. Here we present a case of 61-year man who was bought to ER with restlessness and tachypnoea and was evaluated on clinical basis and along with basic investigation tools was diagnosed with Intra Cerebral Haemorrhage (ICH)
Keywords
ECG, ICH, Neurological lesions, Oesophageal disorders, Pulmonary embolism
Introduction
Neurological lesions like increased intracranial pressure or intracranial hemorrhage have been found to be associated with certain Electrocardiogram (ECG) changes. Disorders of the heart rhythm (e.g. arrthymias) or QT interval (e.g. prolonged), Osborn or U waves are some of the changes which may be associated in these senerios. In areas where all health care access is not available, there are higher chance of center having an ECG machine rather than a Computerised Tomography (CT) scan machine. Thus it may, in additional to the clinical skills of the medical personnel be a help to achieve or point towards a differential.
Case Presentation
A 61 years old man, a known case of diabetes mellitus, hypertension and chronic kidney disease on hemodialysis was bought to hospital in a state of restlessness, moving all four limbs, tachypnoeic and in a gasping state. Patient was apparently normal around 6 hours ago. He went to bathroom and after coming from bathroom felt giddy and sat on the bed. His wife felt as if he was having a hypoglycemic episode and so gave him sugar water to drink which apparently, he himself drank.
His response did not improve over time and he became tachypnoeic and was hence bought to our hospital. There was no history of vomiting, nausea, altered sensorium, loss of consciousness or headache. There was no history of chest pain, abdominal pain and decreased urine output. He is not known to have any drug allergy nor is he supposed to have had any unknown drug or other substances. There was no history of fever, cough, cold or diarrhea.
The patient was a known case of type 2 diabetes mellitus on irregular treatment. He was on hemodialysis for past 1 and half year 3 times a week and his last dialysis was 2 days ago. He was also a known case of hypertension and apparently was on regular medications. He was moderately built and nourished, diet was mixed, sleep was regular with normal bowel and a bladder habit was not a known smoker or a known alcoholic.
Examination
On examination patient was conscious, tachypnoeic, disoriented, responding to oral commands and afebrile. Cardiovascular and respiratory system examination was otherwise normal. Central nervous system examination initially revealed only equivocal plantar. His blood pressure was around 230/130 mmHg. His pulse was 150 per minute regular rhythm, normal volume and character, no radio or radio femoral delay. His respiratory rate was 29 per minute (Figure 1).

Figure 1: ICH bleed.
Investigation and management
Capillary blood glucose done revealed 380 mg/dl. He was provisionally suspected to have diabetic ketoacidosis, t2dm, dyselectronemia, accelerated hypertension, dyspnea for evaluation SHTN and probable sepsis. An ECG was advised (Figure 2). It showed a rate of around 60 per minute, regular rhythm, normal axis, P wave was followed by QRS wave, P wave was normal, QRS wave was normal but QT Prolongation was seen. T wave inversion was present in lead V1 to V6, lead AVL and lead I. U waves were seen in V3, V4, V5 and V6. Tall R waves were seen in V4 and V5. Deep S waves were seen in lead V1 and lead V2. High lateral wall ischemia involving the left main coronary artery along with left ventricular hypertrophy was suspected.
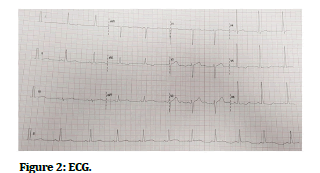
Figure 2: ECG.
However, the general condition of the patient deteriorated. An arterial blood gas analysis was advised earlier was put on hold. PT was started with oxygen and anti-hypertensive medications stat dose was given. Patients CNS examination was repeated and now his pupil was found to be unequal in size with right pupil constricted, 2 mm in size and left pupil 4 mm in size. His GCS was now 7/15. E4, M1, V2. Given the present circumstance the patient was advanced for CT scan. CT scan showed a large ganglion capsular bleed in left side along with mass shift of about 4 mm. Patient was started with anti convulsant therapy, anti-edema measures and advised for urgent neurosurgical intervention and shifted to neurosurgery. Unfortunately the patient later succumbed to the condition.
Discussion
ECG in additional to its cardiac uses, can be useful in many non-cardiac conditions like in esophageal abnormalities, pulmonary embolism, electrolyte disorders, CNS diseases (massive hemorrhage), hypothermia and drug related and other conditions [1]. The electrocardiogram changes observed in patients with raised intracranial pressure include ST-T segment changes, notched T waves, prominent U waves and shortening and prolongation of Q-T intervals [2]. In 1947 Byer, et al. first called attention to the association of abnormal ST-T deflections and central nervous system disease. The most widely accepted view is that the autonomic nervous system, via its connections with the ventricular myocardium, is directly responsible for alterations in ventricular recovery properties [3].
Raised ICP is associated with various ECG changes like widespread giant T wave inversions, QT prolongation, bradycardia (which may indicate the cushing reflex i.e. imminent brainstem herniation). Other possible ECG changes that may be seen include ST segment elevation/ depression which may mimic myocardial ischemia (as in this patient) or pericarditis, increased U wave amplitude, sinus tachycardia, functional rhythms, premature ventricular contractions or may be even atrial fibrillation [4].
ECG changes in case of CNS pathologies can occur due to raised intra cranial pressure and are most commonly seen with massive intracranial hemorrhage like intraparenchymal hemorrhage (hemorrhagic stroke), traumatic brain injury, subarachnoid hemorrhage or massive ischemic stroke causing cerebral edema (e.g. MCA occlusion). The differentials for inverted T waves on the electrocardiogram include both cardiac as well as non-cardiac pathologies like myocardial ischemia and infarction, bundle branch block, ventricular hypertrophy, pulmonary embolism, hypertrophic cardiomyopathy and increased intracranial pressure [5-7]. It is important to note that the findings of deep, inverted T waves on the 12 lead ECG are not diagnostic of ICH but can occur in the appropriate clinical setting and that further diagnostic imaging (e.g. noncontract computed tomography scan of the brain) is required for the diagnosis of ICH.
Conclusion
The changes seen in ECG in patients with SAH maybe non-specific however there always exists the risk of developing serious and lethal issues involving the health of the individual. These patients may develop arrthymias, blocks or even arrests and so it is imperative they be kept under continuous scrutiny and monitoring.
References
- Adams HP, Brott TG, Crowell RM, et al. Guidelines for thrombolytic therapy for acute stroke: A supplement to the guidelines for the management of patients with acute ischemic stroke. A statement for healthcare professionals from a special writing group of the stroke council, American heart association. Circulation 1996; 94:1167–1174.
- Van Mieghem C, Sabbe M, Knockaert D. The clinical value of the ECG in non-cardiac conditions. Chest 2004; 1:1561-1576.
- Abildskov JA, Miller K, Burgess MJ, et al. The electrocardiogram and the central nervous system. Prog Cardiovasc Dis 1970; 1:210-216.
- Gregory T. Cardiovascular complications of brain injury. Contin Educ Anaesth Crit Care Pain 2012; 12:67-71.
- Levis JT. ECG diagnosis: deep T wave inversions associated with intracranial hemorrhage. Perma J 2017; 21.
- Chatterjee S. ECG changes in subarachnoid hemorrhage: A synopsis. Neth Heart J 2011; 19:31-34.
- Milewska A, Guzik P, Rudzka M, et al. J wave formation in patients with acute intracranial hypertension. J Electrocardiol 2009; 42:420-423.
Author Info
Abhilash Nair*, V Padma, Sandhya, Kannan Meera Devi, Saketh Ramineni and Sarath Bhaskar
Department of General Medicine, Sree Balaji Medical College and Hospital, Chrompet, IndiaCitation: Abhilash Nair, V Padma, Sandhya, Kannan Meera Devi, Saketh Ramineni, Sarath Bhaskar, ECG in ICH, J Res Med Dent Sci, 2022, 10 (12): 167-169.
Received: 13-Oct-2022, Manuscript No. JRMDS-22-57354; , Pre QC No. JRMDS-22-57354(PQ); Editor assigned: 17-Oct-2022, Pre QC No. JRMDS-22-57354(PQ); Reviewed: 25-Oct-2022, QC No. JRMDS-22-57354; Revised: 16-Dec-2022, Manuscript No. JRMDS-22-57354(R); Published: 23-Dec-2022
