Research - (2020) Advances in Dental Surgery
Effect of a Relaxation Training Exercise on Behaviour, Anxiety and Pain During Administration of Intra
Ivan Obadiah and EMG Subramanian*
*Correspondence: EMG Subramanian, Department of Pediatric and Preventive dentistry, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical sciences, Saveetha University Tamilnadu, Chennai, India, Email:
Abstract
Dental fear not only stands in the way of rendering proper care to the patient but also is stressful for the pediatric dentist as the treatment might require more time and resources. Because of these and many more reasons, behaviour guidance and management of the dental fear and anxiety is an essential part in rendering dental care to pediatric patients. The aim of the study is to evaluate the efficiency of this bubble breath exercise in improving the behaviour and in reducing the anxiety and pain perception in children of age 6 to 12 years, while injecting intraoral local anaesthesia. The study consisted of 60 children randomly allocated into two groups as 30 children in each group. The tools used to study the parameters were Frankl’s behaviour rating scale and Facial Index Scale (FIS) for behaviour and anxiety and Face Leg Activity Cry Consolability (FLACC) scale and Wong-Baker FACES pain scale for pain perception. The results were analysed statistically using SPSS Software version 23. Results of this study conclude that the bubble breath exercise is effective in improving the behaviour and reducing anxiety of the child but not much effective in reducing the pain perception during administration of local anaesthetic.
Keywords
Behaviour management, Breathing exercise, Dental anxiety
Introduction
Pediatric dentistry stands out from general dental practice by its exclusivity of having children as their patient population. Among various factors which challenges a pediatric dentist to render perfect dental treatment, the child’s behaviour and anxiety plays the chief role. A survey in Texas found that among a group of adult dental patients 12% of the people reported with high dental fear and 18% of them had moderate dental fear [1]. Another study conducted in south India has shown that more than 50% of the study population exhibited moderate to extreme dental anxiety [2]. When even adult patients are exhibiting a high range of anxiety towards dental treatment, children are no exception and rather they present with more dental fear and anxiety. In a study conducted among 400 south-indian children of 6 to 12 years old, more than 60% of the children had dental anxiety [3].
Dental fear not only stands in the way of rendering proper care to the patient but also is stressful for the pediatric dentist as the treatment might require more time and resources [4]. And because of these and many more reasons, behaviour guidance and management of the dental fear and anxiety is an essential part in rendering dental care to pediatric patients [5]. Some of the previously existing techniques for reducing the dental fear and perception of dental pain are distraction, relaxation strategies and coping mechanisms. The background of these techniques is the gate-control theory, which describes how ascending signals of pain are influenced by the descending signals due to thoughts and attention [6].
As the children are still developing their reasoning abilities and verbal skills, they feel anxious in even observing the dental arena and while trying to establish a conversation with the dentist. So, it is the clinician’s responsibility to modify and shape the emotions of the pediatric patient and help him receive the dental care without unnecessary fear and anxiety. A deep breathing exercise known as bubble breath is a highly effective ‘play therapy’ technique used by psychologists to communicate with anxious children. It is also used as a distraction technique for pain management in kids during vaccinations [7], and to decrease pain perception in chronic conditions like cancer [8]. Sridhar et al. in 2019 used this exercise as a cognitive behaviour modification technique and found positive results in reducing the pain perception in pediatric dental patients during buccal infiltration of local anaesthesia [9].
Our department is passionate about childcare, we have published numerous high-quality articles in this domain over the past 3 years [10-28]. With this inspiration we planned to pursue research on the effectiveness of this relaxation exercise. In this study, the aim is to evaluate the efficiency of this bubble breath exercise in improving the behaviour and in reducing the anxiety and pain perception in children of age 6 to 12 years, while injecting intraoral local anaesthesia.
Materials and Methods
This was a randomized controlled trial with a parallel group design and a 1:1 allocation ratio. Ethical approval was given by the Institutional review board and the study was conducted in the department of Paediatric and preventive dentistry over a period of 5 months from September 2019 to January 2020. The study population consisted of children of age 6 to 12 years, who were scheduled for a procedure which involves administration of local anaesthesia. Children whose behaviour rating is categorized under positive and negative during the dental examination at the first visit are excluded from the study.
First visit
Dental examination and provision of the soap bubble toy.
In the first visit, children who were 6 to 12 years of age were selected for the study. During the dental examination, the behaviour of the child was categorized using Frankl’s behaviour rating scale. Children who were exhibiting negative and positive behaviour were included in the study. After dental examination, if the child doesn’t require any procedure that involves administration of local anaesthesia they were excluded from the study. Once the patient is included in the study, they were randomly allocated into two groups (Group 1 and 2) which were Case group and Control group. The children who were categorized under the case group were provided with a ‘commercially available fancy soap solution’ which they commonly refer to as the ‘Bubble toy’ (Figure 1).
Figure 1: Fancy soap bubble toy.
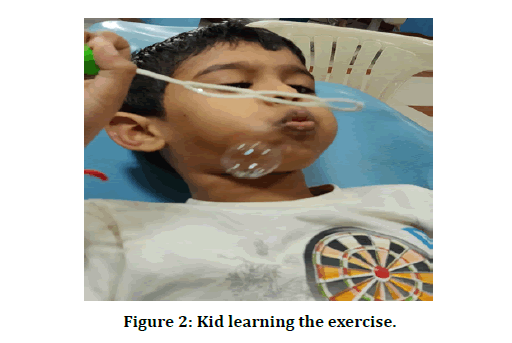
Deep breathing exercise was taught to the children as to inhale deep breaths from the stomach and slowly exhale as if blowing the air out until asked to stop. After repeating this several times till the child got used to the breathing exercise, the subjects were made to blow the bubble blower using the same breathing pattern, blowing a large bubble without breaking it. The children were encouraged to blow big bubbles by inhaling deeply and exhaling them into bubbles which were repeated for 10 times (Figure 2). The parents were made to observe this learning and a one-week chart was given to the parent. The parent had to make the child do this exercise daily at home for ten times for a minimum of four continuous days before the next appointment. The children who were allocated in the control group were not taught about this breathing exercise and were not provided with any soap solutions.
Figure 2: Kid learning the exercise.
Second visit
Procedural visit.
In the second visit in which the procedure was going to be done, the chart given to the parent was checked for the completion of the breathing task. After confirming that the children under the case group followed the instructions of the breathing exercise properly, they were made to settle on the dental chair for their treatment. The procedures to be done were pulp therapy or extraction. Topical anaesthetic (Nummitlignocaine spray) was sprayed on the injection site for 30 seconds prior to the injection of local anaesthetic solution (2% lignocaine with adrenaline). The behaviour, pain perception and anxiety of the child were monitored during the administration of local anaesthesia. For children who became uncooperative and started refusing treatment out of fear and anxiety, conventional behaviour management techniques such as tellshow- do, modelling, voice control were used.
The study consisted of 60 children randomly allocated into two groups as 30 children in each group. The tools used to study the parameters were Frankl’s behaviour rating scale and Facial Index Scale (FIS) for behaviour and anxiety and Face Leg Activity Cry Consolability (FLACC) scale and Wong-Baker FACES pain scale for pain perception. The results were analysed statistically using SPSS Software version 23. The level of significance was set at 5% (P<0.05). The difference in the behaviour rating and the pain perceptions were statistically analysed between the groups using Mann-Whitney test and intra group comparison by Wicoxon signed-rank test.
Results and Discussion
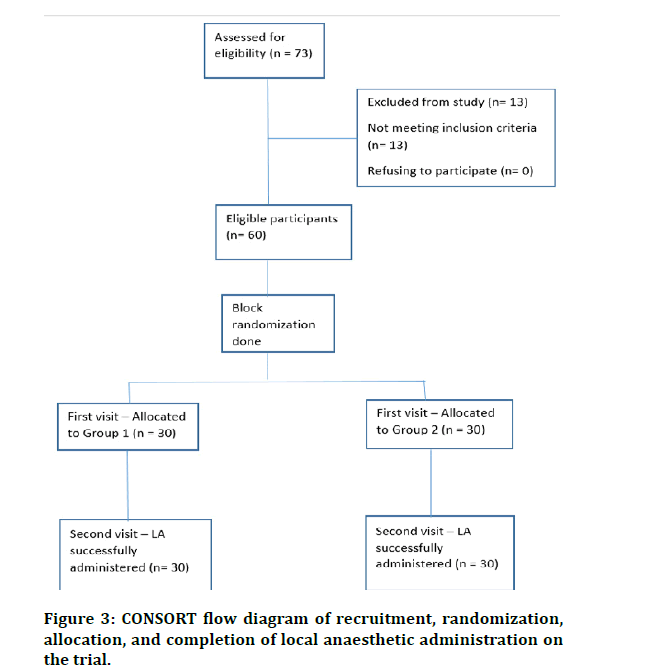
The sample selection, randomization, allocation and performing the scheduled procedure which is administration of local anaesthetic to the children of both groups are represented in the CONSORT flow diagram (Figure 3). A total of 60 children with a mean age of 8.43 +1.54 years (37 males and 23 females) were involved in the study.
Figure 3: CONSORT flow diagram of recruitment, randomization, allocation, and completion of local anaesthetic administration on the trial.
Intergroup comparison using Mann-Whitney U test for dental anxiety as measured using the FIS score showed no significant differences in the first appointment, but there was a significant difference between the groups in the second visit (Table 1). Intragroup comparison using the Wilcoxon signed-rank test showed a significant difference between the FIS score of the case group (P-value=0.042). Behaviour as measured by the Frankl scale was clinically observed to be improved in the second visit in children of the case group. Pain perceived as measured by the WBFPRS showed no statistically significant difference between the groups (Table 2). And no significant differences were noticed between the FLACC scores of two groups (P-value= 0.061).
| FIS | Groups | Mean ± SD | Median | Mean rank | P Value |
|---|---|---|---|---|---|
| First visit | Group 1 | 1.84 ± 0.69 | 2 | 34.56 | 0.421 |
| Group 2 | 1.68 ± 0.63 | 2 | 30.52 | ||
| Second appointment | Group 1 | 1.92 ± 0.69 | 2 | 35.18 | 0.367* |
| Group 2 | 1.63 ± 0.62 | 2 | 27.65 |
*P<0.05 Significant
Table 1: The intergroup comparison of the dental anxiety measured using the FIS. Statistical analysis was done using Mann- Whitney U test. There was a significant difference between the groups in the second visit (p value=0.367).
| Groups | Mean ± SD | Median | Mean rank | P Value |
|---|---|---|---|---|
| Group 1 | 2.41 ± 0.52 | 1 | 41.44 | 0.673 |
| Group 2 | 1.47 ± 0.63 | 1 | 18.56 |
*P>0.05 Not Significant
Table 2: Inter group comparison of pain perceived, as measured by the Wong-Baker FACES pain scale. Statistical analysis was done using Wilcoxon signed rank test. The difference between the control group and the intervention group regarding the pain perception is statistically not significant ( P value=0.673).
In this current study we compared the dental anxiety, behaviour of children between the visits, and pain perception during administration of local anaesthetic thereby evaluating the effectiveness of the breathing exercise using the soap bubble toy. Clinically, children of both the groups (case and control) seemed calmer and more comfortable in the second visit when compared to their first visit. This is because of the desensitization that occurred in the dental set up during initial examination in the first visit. However no statistically significant difference was obtained between the pain perception during the administration of local anaesthetic which is contradictory to the results observed in a similar study by Sridhar et al. [9]. The breathing exercise we made the children to carry out by blowing bubbles using the soap solution, prevents the holding of breath because of the pain stimulus, thereby preventing the exaggeration of the pain sensation, thus promoting relaxation [6]. Factors like inherent coping ability of the child, personality, complexion, however, may have influenced the dental anxiety thereby serving as confounding factors in the study [4,29]. Other considerable factors which can influence the dental anxiety and behaviour of a child are socio-economic status of the family, influence of the siblings and the anxiety of the parents [30,31]. The Facial Image scale used as a tool to measure dental anxiety in this study as a self-reported measure has been proven to have good validity [9]. This scale is most commonly used as it gives an immediate feedback on the child’s state of anxiety to the observer [32]. However as mentioned earlier, cognitive, social and contextual influences may have influenced the responses, thereby affecting the outcome of this study [33]. There is also trait anxiety which is the inherent vulnerability of an individual during an anxious situation which might have influenced the results of Facial image scale as it is a self-reported state of anxiety [34]. In future studies regarding dental anxiety and behaviours there significant factors must be taken into consideration. In this study pulse rate of the child is not measured to determine the anxiety of the child during administration of local anaesthetic. In a similar study done by Sridhar et al, the pulse rate served as an effective tool as it is the reflection of the physiological changes that can occur in the body in response to stress and dental treatments [34]. In that study, there were increased mean pulse rate values in both the groups during the local anaesthetic administration, with the relaxation exercise group showing higher increase in the mean pulse rate values, than the control group [9]. This is partially due to the endogenous epinephrine release owing to emotional stress [35].
In this study as all the participants belonged to the age group of 6 to 12 years, the children were inherently seemed to be capable of coping to the dental treatments and were seemed to understand the treatment process as explained by the dentist. Only those patients who are categorized under negative and positive behaviour according to Frankl behaviour scale were included and those exhibiting extremely cooperative behaviour and extremely uncooperative behaviour were not included in the study. The results suggest the needs to explore various other factors which alter the behaviour of a child towards dental treatments despite dental anxiety, hence allowing the clinician to select and use the appropriate behaviour management techniques.
Measuring the intensity of pain and presenting them quantitatively is a very tedious process for the clinician, as it is an internal expression of the stimuli. Hence quantifying pain is usually presented with a great range of variation especially among anxious children. A self-report by the patient can be considered as a reliable way of measuring pain. One easy method preferred by the children to quantify pain is through pictorial pain scales depicting faces [33]. In this present study, WBFPRS, a face pain scale was used as a self-reported measure of pain. This scale is simple and also had good acceptability among the children, clinician and the parents [36]. Any self-reported scale has the drawbacks as however, the developmental, cognitive and situational issues may affect the child’s report of pain. Hence, an additional behaviour rating scale or a psychological evaluation scale will be helpful in approximating the actual measure of pain [33]. FLACC scale is used as an adjunct to WBFPRS in this study.
In this study, no statistically significant difference was noticed between the two groups regarding the measure of pain perception during administration of local anaesthesia. However, clinically children belonging to the intervention group seemed calmer and more capable of bearing pain during the infection of the needle. Statistically significant differences were obtained between the behaviours of the children in the intervention group, between the visits. These results contrast with previous similar studies. These breathing relaxation exercises were known to enhance vagal activity and produce serotonin which is an anti-pain neurotransmitter and also decrease the levels of stress hormones. This series of events resulting in relaxing the body in response to the regular practise of the exercise are collectively referred to as relaxation response [37]. Though anxiety is an important determinant of pain it may be altered by psychological factors and coping abilities of the individual [29]. One of the main confounding factors in this study is that the child gets used to the dental set up and establishes a good rapport with the dentist on the first visit while receiving the soap solution as a toy. This thereby improves the behaviour and reduces the anxiety in the next visit regardless of the relaxation exercise. The exercise was not only practiced between the visits but also, the child was asked to breathe deeply as blowing big bubbles which served as an effective distraction method during administration of local anaesthetic.
In another similar study conducted earlier, similar results were obtained where the dental anxiety and behaviour of the patient improved by the relaxation exercise whereas the pain perception of the child showed no significant difference between the groups [38]. Further studies involving relaxation exercises as a behaviour shaping and anxiety management technique should be carried out to analyses its efficiency and in comparison, with other behaviour shaping techniques.
Conclusion
Use of bubble breath exercise is effective in improving the behaviour of children of age 6 to 12 years.
Dental anxiety can be reduced by use of bubble breath exercise in children of age 6 to 12 years.
No significant difference was observed between the children who used bubble breath exercise and the children who didn't regarding the pain perception during administration of local anaesthetic.
Acknowledgement
The authors of the current study acknowledge the Saveetha University for providing ethical clearance as required for the successful completion of the study
Conflict of Interest
No conflict of interests was declared by the authors.
References
- Gatchel RJ. The prevalence of dental fear and avoidance: Expanded adult and recent adolescent surveys. J Am Dent Assoc 1989; 118:591–593.
- Appukuttan D, Subramanian S, Tadepalli A, et al. Dental anxiety among adults: an epidemiological study in South India. North Am J Med Sci 2015; 7:13–18.
- Kumar V, Goud ES, Turagam N, et al. Prevalence of dental anxiety level in 6- to 12-year- old South Indian children. J Pharm Bioallied Sci 2019; 11:S321–S324.
- Klingberg G, Broberg AG. Dental fear/anxiety and dental behaviour management problems in children and adolescents: A review of prevalence and concomitant psychological factors. Int J Paediatr Dent 2007; 17:391–406.
- American academy on pediatric dentistry clinical affairs committee-behavior management subcommittee and american academy on pediatric dentistry council on clinical affairs. Guideline on behavior guidance for the pediatric dental patient. Pediatr Dent 2008; 30:125–133.
- Jacobs A, Price HN, Popenhagen MP. Blowing away the pain: A technique for pediatric pain management. Pediatr Dermatol 2014; 31:757–758.
- French GM, Painter EC, Coury DL. Blowing away shot pain: A technique for pain management during immunization. Pediatr 1994; 93:384–388.
- Kuppenheimer WG, Brown RT. Painful procedures in pediatric cancer. A comparison of interventions. Clin Psychol Review 2002; 22:753–786.
- Sridhar S, Suprabha BS, Shenoy R, et al. Effect of a relaxation training exercise on behaviour, anxiety, and pain during buccal infiltration anaesthesia in children: Randomized clinical trial. Int J Paediatr Dent 2019; 29:596–602.
- Govindaraju L, Jeevanandan G, Subramanian EMG. Comparison of quality of obturation and instrumentation time using hand files and two rotary file systems in primary molars: A single-blinded randomized controlled trial. Eur J Dent 2017; 11:376–379.
- Govindaraju L, Jeevanandan G, Subramanian EMG. Knowledge and practice of rotary instrumentation in primary teeth among Indian dentists: A questionnaire survey. J Int Oral Health 2017; 9:45.
- Panchal V, Gurunathan D, Shanmugaavel AK. Smartphone application as an aid in determination of caries risk and prevention: A pilot study. Eur J Dent 2017; 11:469–474.
- Ravikumar D, Jeevanandan G, Subramanian EMG. Evaluation of knowledge among general dentists in treatment of traumatic injuries in primary teeth: A cross-sectional questionnaire study. Eur J Dent 2017; 11:232–237.
- Jeevanandan G, Govindaraju L. Clinical comparison of Kedo-S paediatric rotary files vs manual instrumentation for root canal preparation in primary molars: A double blinded randomised clinical trial. Eur Archives Paediatr Dent 2018; 19:273–278.
- Nair M, Jeevanandan G, Vignesh R, et al. Comparative evaluation of post-operative pain after pulpectomy with k-files, kedo-s files and mtwo files in deciduous molars: A randomized clinical trial. Br Dent Sci 2018; 21:411.
- Ravikumar D, Gurunathan D, Gayathri R, et al. DNA profiling of Streptococcus mutans in children with and without black tooth stains: A polymerase chain reaction analysis. Dent Res J 2018; 15:334.
- Dhanalakshmi Ravikumar SN, Ramakrishna M, Sharna N, et al. Evaluation of McNamara’s analysis in South Indian (Tamil Nadu) children between 8-12 years of age using lateral cephalograms. J Oral Biol Craniofac Res 2019; 9:193–197.
- Ravindra V, Rekha V, Annamalai S, et al. A comparative evaluation between dermatoglyphic patterns and different terminal planes in primary dentition. J Clin Exp Dent 2018; 10:e1149–e1154.
- Ravindra V, Rekha CV, Annamalai S, et al. (2019) A comparative evaluation between cheiloscopic patterns and the permanent molar relationships to predict the future malocclusions. J Clin Exp Dent 2019; 11:e553–e557.
- Subramanyam D, Gurunathan D, Gaayathri R, et al. Comparative evaluation of salivary malondialdehyde levels as a marker of lipid peroxidation in early childhood caries. Eur J Dent 2018; 12:67–70.
- Vishnu Prasad S, Kumar M, Ramakrishnan M, et al. Report on oral health status and treatment needs of 5-15 years old children with sensory deficits in Chennai, India. Special Care Dent 2018; 38:58–59.
- Jeevanandan G, Ganesh S, Arthilakshmi. Kedo file system for root canal preparation in primary teeth. Indian J Dent Res 2019; 30:622–624.
- Ramadurai N, Gurunathan D, Samuel AV, et al. Effectiveness of 2% Articaine as an anesthetic agent in children: randomized controlled trial. Clin Oral Investigations 2019; 23:3543–3550.
- Ramakrishnan M, Dhanalakshmi R, Subramanian EMG. Survival rate of different fixed posterior space maintainers used in paediatric dentistry-A systematic review. Saudi Dent J 2019; 31:165–172.
- Panchal V, Jeevanandan G, Subramanian E. Comparison of instrumentation time and obturation quality between hand K-file, H-files, and rotary Kedo-S in root canal treatment of primary teeth: A randomized controlled trial. J Indian Society Pedodont Preventive Dent 2019; 37:75–79.
- Vignesh R, Ditto Sharmin C, Annamalai S, et al. Management of complicated crown-root fracture by extra-oral fragment reattachment and intentional reimplantation with 2 years review. Contemporary Clin Dent 2019; 10:397–401.
- Panchal V, Jeevanandan G, Subramanian EMG. Comparison of post-operative pain after root canal instrumentation with hand K-files, H-files and rotary Kedo-S files in primary teeth: A randomised clinical trial. Eur Archives Paediatr Dent 2019; 20:467–472.
- Samuel SR, Acharya S, Rao JC. School Interventions-based prevention of early-childhood caries among 3-5-year-old children from very low socioeconomic status: Two-year randomized trial. J Public Health Dent 2020; 80:51–60.
- Marsac ML, Funk JB. Relationships among psychological functioning, dental anxiety, pain perception, and coping in children and adolescents. J Dent Children 2008; 75:243–251.
- Gustafsson A, Arnrup K, Broberg AG, et al. Psychosocial concomitants to dental fear and behaviour management problems. Int J Paediatr Dent 2007; 17:449–459.
- Wu L, Gao X. Children’s dental fear and anxiety: Exploring family related factors. BMC Oral Health 2018; 18:100.
- Buchanan H, Niven N. Validation of a facial image scale to assess child dental anxiety. Int J Paediatr Dent 2002; 12:47–52.
- Tomlinson D, Von Baeyer CL, Stinson JN, et al. A systematic review of faces scales for the self-report of pain intensity in children. Pediatrics 2010; 126:1168–1198.
- Han HR. Measuring anxiety in children: a methodological review of the literature. Asian Nursing Res 2009; 3:49–62.
- Brand HS, Abraham-Inpijn L. Cardiovascular responses induced by dental treatment. Eur J Oral Sci 1996; 104:245–252.
- Garra G, Singer AJ, Taira BR, et al. Validation of the wong-baker FACES pain rating scale in pediatric emergency department patients. Academic Emergency Med 2010; 17:50–54.
- Jacobs GD. The physiology of mind–Body interactions: The stress response and the relaxation response. J Alternative Complementary Med 2001; 7:83–92.
- Peretz B, Gluck GM. Assessing an active distracting technique for local anesthetic injection in pediatric dental patients: Repeated deep breathing and blowing out air. J Clin Pediatr Dent 1999; 24:5–8.
Author Info
Ivan Obadiah and EMG Subramanian*
Department of Pediatric and Preventive dentistry, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical sciences, Saveetha University Tamilnadu, Chennai, IndiaCitation: Ivan Obadiah, EMG Subramanian, Effect of a Relaxation Training Exercise on Behaviour, Anxiety and Pain During Administration of Intra-Oral Local Anaesthesia in Children of Age 6 to 12 years: Randomized Controlled Trial, J Res Med Dent Sci, 2020, 8 (7): 364-370.
Received: 23-Sep-2020 Accepted: 05-Nov-2020 Published: 12-Nov-2020