Research - (2021) Volume 9, Issue 7
Evaluation of Facial Nerve Function Following Preauricular and Submandibular Approaches by using the House-Brackmann Facial Nerve Grading System
Yousif Jabbar Jiheel* and Najwa Jamil Al-Chalabi
*Correspondence: Yousif Jabbar Jiheel, Department of Oral and Maxillofacial Surgery, University of Baghdad, Iraq, Email:
Abstract
Background: The functional and cosmetic integrity of the facial nerve is critical that should be preserved by the surgeons. Clinically, facial nerve function is evaluated by using the House-Brackmann grading scale, which also allows physician to improve the patient’s facial nerve recovery during follow up periods. Aims of study: The purpose of this study was to assess the facial nerve function following preauricular and submandibular surgical approaches by using the House–Brackmann facial nerve grading system as a means of classifying and measuring the degree and type of injury. Patients and methods:- a prospective study included fifty patients (18 male, 32 female) patients’ age ranged from 18 to 75 years with a mean of 45.16 years were underwent for preauricular approach for parotidectomy and submandibular approach for reduction and fixation of the fracture mandible & excision the submandibular tumor, Facial nerve function was evaluated of all patients preoperatively, postoperatively at 24 h, 1 week, 1 month, 3 months, 6 months by using House-Brackmann Facial Nerve Grading Scale. Statistical analysis was done using SPSS 25. Results: From fifty patients, marginal mandibular branch of facial nerve was seen in 34 patients seen a slightly weakness and the House- Brackmann grade II, complete recovery of a marginal mandibular branch of facial nerve after one-month post-operative and the House –Brackmann grade I. Conclusions: The marginal mandibular branch of facial nerve injury weakness may be occurred in preauricular and submandibular surgical approaches and the transient weakness of marginal mandibular &temporal branches of facial nerve can be evaluate by using the House- Brackmann scale.
Keywords
Facial nerve, Preauricular incision, Otolaryngology, Embryology.
Introduction
Preauricular incision is made along the natural crease anterior to the tragus almost invisible scars are main advantages of a preauricular approach. This surgical technique provides access to the superior part of the TMJ and anteromedially displaced mandibular condyle [1].
The House-Brackmann grading system has been extremely helpful in standardizing reporting of facial nerve paralysis Dr. House classified facial nerve scales as gross, regional, or specific [2].
Gross scales make an overall assessment of facial motor function. regional scales, in contrast, ascribe independent scores to different areas of facial nerve function, sometimes with weighting to reflect the greater or lesser importance of given areas of the face, such as eye closure or mouth movement. In regional systems, forehead scores may have lower impact due to less impact on cosmesis, relatively less associated functional disability [3].
The scale that Dr. House introduced in 1983 is a gross scale was soon modified by Dr. Brackmann in 1985 to give rise to the current six-level House-Brackmann scale based on their degree of facial nerve dysfunction. This scale, which was formally adopted as the universal standard of the American academy of otolaryngology–head and neck surgery on recommendation of the facial nerve disorders committee sought to group together patients with similar degrees of disability [4].
The measurement of facial nerve function in a consistent, reliable manner is an important but elusive goal due to the inherent complexity of facial nerve physiology. Not only does the nerve control multiple motor regions of the face but also it controls special functions such as lacrimation, salivation, and taste. The major problem in evaluating the results of facial nerve injury lies in the subjective methods of assessment and reporting. the House-Brackmann grading system is a gross subjective scale that considers overall facial functions and assigns patients to six categories. This system intentionally considers facial expression at rest and in motion as well as the presence of secondary defects [5,6].
In our study, we used the House –Brackmann scale in evaluation the facial nerve dysfunction after preauricular and submandibular surgical approaches after one day, one week, one month, three months and six months, and assessment improvement.
Embryology of facial nerve
In the third week of intrauterine development appears the facio-acoustic primordium, this structure originates from the rhomb encephalon and develops in the rostral sense to the otic placode [7].
The primordium splits in an around 4 weeks into a caudal main trunk and a rostral sensory (chorda tympani) trunk which enters the first mandibular arch.
The majority development anatomy of the facial nerve is takes place within the first 3–4 months of fetal life [8].
The peripheral motor divisions appear by the eighth week when development of the second arch progresses to individual muscle groups. At this time, the horizontal and vertical portions of the facial nerve run anterior to the external auditory canal and have started to demarcate. The weeks following the eighth week are characterized by extensive arborization of the peripheral facial nerve and the corresponding development of the muscles of facial expression.
The facial nerve finally exits the stylomastoid foramen in its usual position by week 30, but it continues to lie superficial until the development of the mastoid tip between 1 and 3 years of age [9].
Anatomy of facial nerve
The facial nerve has the longest and most tortuous course in the skull of any cranial nerve. There are four brainstem nuclei to cranial nerve VII, the facial motor nucleus, which controls muscles of facial expression; the superior salivatory nucleus, which sends fibres for lacrimal gland secretion and salivary secretion; the nucleus solitarius, which receives fibres of taste for the anterior two-thirds of the tongue; and the trigeminal sensory nucleus, which receives sensory fibers for a small portion of the external ear [10].
The facial nerve arises in the pons as 2 roots: A larger medial motor root and a smaller lateral sensory root, also called the (nervus intermedius) which contains fibres arising from both the sensory nucleus and the salivatory nuclei. both roots exit the lower lateral aspect of the pons between the inferior cerebellar peduncle and the olive [11].
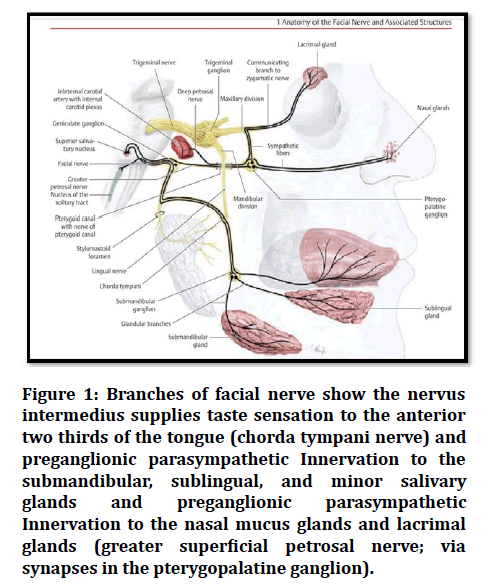
The efferent branchial motor (special visceral efferent) to supply the muscles derived by the mesoderm of II branchial arch which are stapedius, stylohyoid, posterior belly of digastric, and muscles of facial expression, including the buccinator, platysma, and occipitals, occipitofrontalis muscles see Figure 1 [12].
Figure 1: Branches of facial nerve show the nervus intermedius supplies taste sensation to the anterior two thirds of the tongue (chorda tympani nerve) and preganglionic parasympathetic Innervation to the submandibular, sublingual, and minor salivary glands and preganglionic parasympathetic Innervation to the nasal mucus glands and lacrimal glands (greater superficial petrosal nerve; via synapses in the pterygopalatine ganglion).
The visceral motor (general visceral efferent somatic) originates in superior salivatory nucleus and parasympathetic innervation of the lacrimal, submandibular, and sublingual glands and glands within the mucous membrane of the nose and hard and soft palates see Figure 1 [7].
The general sensory (general somatic afferent) component of the facial nerve is complex and consists of, sensory fibres from the skin of portions of the auricle and external auditory canal See Figure 1 [13].
The special sensory (special visceral afferent) innervate the taste sensation from the anterior two third of tongue and hard and soft palates see Figure 1 [14].
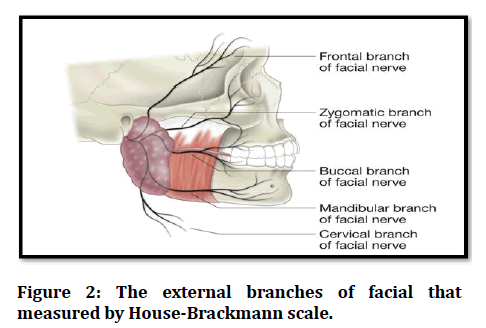
There are 5 main branches of the facial nerve in the face with direct clinical relevance to the House-Brackmann scale: temporal, zygomatic, buccal, marginal mandibular and cervical branches (Figure 2) [15].
Figure 2: The external branches of facial that measured by House-Brackmann scale.
The functionality of these 5 branches is the main concern in the of grading facial nerve recovery after surgery by using the House-Brackmann scale [16].
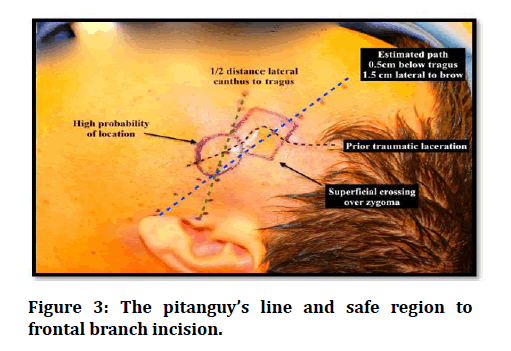
The trajectory of the frontal branch is classically defined by (Pitanguy’s line) (Figure 3) a line drawn from a point 0.5 cm inferior to the tragus to a point 1.5 cm superior and lateral to the eyebrow, although this has been widely criticized as reliant on soft landmarks and therefore inconsistent [17].
Figure 3: The pitanguy’s line and safe region to frontal branch incision.
Figure 4 presents the extracranial branches of facial nerve with relation to the facial layers.
Figure 4: The extracranial branches of facial nerve with relation to the facial layers.
Patients and Methods
The sample
A prospective study for fifty patients for assessment a facial nerve dysfunction after preauricular and submandibular surgical approaches by using a House– Brackmann grade scale in group of patient’s ages between (18-75) years old those arrived at maxillofacial surgery department at AL-Shaheed Gazzi AL-Hariri Hospital, Medical City–Baghdad, from January 2020 until April, 2020.
The inclusion criteria
- The selected patients which are treated by preauricular approach for treatment of.
- Examples: Benign parotid tumour, sub condylar fracture of mandible bone, temporomandibular joint (TMJ) ankylosis.
- The patients who treated the submandibular salivary gland tumor or in case of angle and body fracture of mandible by using by submandibular incision approach.
Exclusion criteria
- Patients who with congenital conditions such as Möbius syndrome, hemifacial microsomia, dystrophia myotonica or patients had neurologic deficits before surgery Such as Guillain-Barre syndrome.
- In patients have malignant tumor that facial nerve should be scarified.
- The patients had history of trauma (temporal bone fracture, penetrating injury to the face, facial laceration).
General evaluation and assessment for the patients
A standardized case sheet was used for each patient and used for evaluation, assessment improvement of facial nerve physiological action.
The general formula of the patient’s case sheet was:
- Patient personal data which include name, age, sex, and occupation.
- Chief complaint, nature, the past medical history.
- Clinical examination for the defect side, and facial symmetry.
- The preoperative and postoperative photographs were taken to the surgical or prospective surgical site illustrated the patient’s defect, The photographic views were taken in the frontal view with neutral head position in each follow up visit after 24 hours, one week, one month, 3 months and 6 months and records in case sheet.
- The case sheet used in our study in appendix of our study.
Measurement procedures
Assessment of facial nerve function was done pre-and post-operatively at 24 h, 1 week, 1 month, 3 months, and 6 months by using House-Brackmann facial nerve grade system.
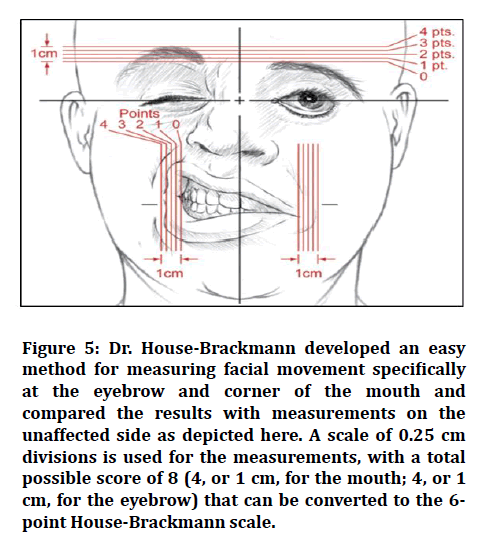
The pre and postoperative photographs were taken by the same photographer using the same camera I phone max pro mobile (2x to 2.5x) and magnification. The patients were photographed facing the camera in the following positions: At rest, raising the eyebrows, closing the eyes with minimum effort and with maximal efforts, blowing the mouth (Figure 5) The patients were assessed by using House-Brackmann scale and the data were statistically analysing according to branch of facial nerve its effect (Figure 5).
Figure 5: Dr. House-Brackmann developed an easy method for measuring facial movement specifically at the eyebrow and corner of the mouth and compared the results with measurements on the unaffected side as depicted here. A scale of 0.25 cm divisions is used for the measurements, with a total possible score of 8 (4, or 1 cm, for the mouth; 4, or 1 cm, for the eyebrow) that can be converted to the 6- point House-Brackmann scale.
Marking and measuring
Mark point in midline of lower lip and another points in corners of mouth (commissure of lips) and measure 1cm for each side and subdivided into 0.25cm and measure from middle point to effected side point and compared result with measure of the normal side point and decrease in measurements in effected side given the description the House-Brackmann facial nerve grade (Figure 5).
The assessment for frontal branch of facial nerve by mark point in the mid-portion of the top of the eyebrow and measuring the is determined upwards (superior) movement from each reference point scores 1 point for each 0.25 cm movement, up to a maximum of 1 cm in comparison measurements with normal side giving the House-Brackmann facial nerve grade (Figure 5 and Table 1).
Table 1: The House-Brackmann scale. D=Distance between location of point on neutral image and that in the test image.
| Grade | Description | Measurement |
|---|---|---|
| I | Normal | D>1.0 |
| II | Slight | 1.0 |
| III | Moderate | 0.5 |
| IV | Moderately- sever | 0.25 |
| V | Sever | D>0.25 |
| VI | Total | D=0 |
Results
The total number of study patients was fifty of them were evaluated for frontal and marginal mandibular branches of facial nerve function after preauricular and submandibular incision.
Age and gender
The distribution of study patients by age and gender is shown in. Study patients’ age was ranging from 18to 75 years with a mean of 45.16 years and a standard deviation (SD) of ± 16.3 years.
We noticed that 36% of study patients were aged between 40– 49 years and 36%of them were aged ≥ 50 years, regarding gender, proportion of females was higher than males (64% versus 36%) with a male to female ratio of 1:1.7.
Clinical information
Table 2 shows the distribution of study patients by certain clinical information. In this study, 56% of study patients were operated by preauricular incision.
Table 2: Distribution of study patients by certain clinical information.
| Clinical Information | No. (n= 50) | Percentage (%) |
|---|---|---|
| Type of procedure | ||
| Preauricular incision | 28 | 56 |
| Submandibular incision | 22 | 44 |
| Type of lesion | ||
| Parotid pleomorphic adenoma | 26 | 52 |
| Submandibular gland tumor | 12 | 24 |
| Fracture body of mandible | 10 | 20 |
| Ankylosis | 2 | 4 |
The most common type of lesion was parotid pleomorphic adenoma (52%).
Table 3 shows the grades of house-brackmann scale for marginal mandibular branch of facial nerve.
Table 3: Grades of house-brackmann scale for marginal mandibular branch of facial nerve.
| House Brakmann Scale for Marginal mandibular branch of facial nerve | No. (n=50) | Percentage (%) |
|---|---|---|
| After one day | ||
| Grade I | 16 | 32 |
| Grade II | 34 | 68 |
| After one week | ||
| Grade I | 18 | 36 |
| Grade II | 32 | 64 |
| After one month | ||
| Grade I | 50 | 100 |
| After three months | ||
| Grade I | 50 | 100 |
| After six months | ||
| Grade I | 50 | 100 |
The association between grades of House- Brackmann Scale for marginal mandibular branch of facial nerve after one week is shown in table 4. Mean of time of operation was significantly (P= 0.001) higher in patients graded II than that in those graded I. No statistical significant associations detected (P ≥ 0.05) between grades of House Brackmann Scale and all of characteristics.
Table 4: Association between grades of House-Brackmann scale for marginal mandibular branch of facial nerve after one week.
| Variable | House Brakmann Scale after one week | Total (%) | P-Value | |
|---|---|---|---|---|
| Grade II (%) (n=32) | Grade I (%) (n=16) | n=50 | ||
| Age (Year) | ||||
| <20 | 8 (57.1) | 6 (42.9) | 14 (28.0) | 0.059 |
| 40–49 | 10 (55.6) | 8 (44.4) | 18 (36.0) | |
| ≥ 50 | 14 (86.9) | 4 (11.1) | 18 (36.0) | |
| Gender | ||||
| Male | 14 (77.8) | 4 (22.2) | 18 (36.0) | 0.266 |
| Female | 20 (62.5) | 12 (37.5) | 32 (64.0) | |
| Type of procedure | ||||
| Preauricular | 20 (71.4) | 8 (28.6) | 28 (56.0) | 0.558 |
| Submandibular | 12 (63.6) | 10(36.4) | 22 (44.0) | |
| Type of lesion | ||||
| Parotid P. adenoma | 18 (69.2) | 8 (30.8) | 26 (52.0) | 0.527 |
| Submandibular g. tumor | 8 (71.4) | 4 (28.6) | 12 (24.0) | |
| Fracture body of mandible | 4 (40.0) | 6 (50.0) | 10(16.0) | |
| Ankylosis of TMj | 2 (100.0) | 0 (0) | 2 (4.0) | |
| Mean ± SD | Mean ± SD | 0.001 | ||
| Time of operation (h) | 2.26 ± 0.43 H | 1.15 ± 0.22 | ||
Discussion
The identification and preservation of the facial nerve remains an important step in head and neck surgery and risk of iatrogenic injury is due to variability in the number of nerve branches, the varying positions [18,19].
The facial nerve injury causes a weakness of innervation of the circumoral musculature, leading to asymmetry of facial expression and imbalance of the lower lip and inability to move it laterally and downward, or enable raise eyebrows has a great impact on the patient’s quality of life and self-appearance and might lead to legal claims [20,21].
The marginal mandibular nerve runs almost historically described above the lower border of the mandible; various authors noted a submandibular course of the marginal mandibular nerve. The marginal mandibular nerve almost always crosses the posterior facial vein (retromandibular vein) superiorly and the anterior facial vein superficially, although its intersection with the facial artery can vary [22].
Demographic data
In this research, the age of patients ranged from 14 to 80 years. We noticed that 72% of study patients were aged between 40–75 years and agree with study reported that by [23] that found 80% of the patients in same ranged group have tumours.
The patients aged between 40-75 years see 18 cases 69% from 26 patients after parotidectomy (superficial ,deep lobe parotidectomy) and see slightly facial nerve weakness and the House-Brackmann grade II in first week and recovery after one month and (P value 0.527).
This agrees with study reported by [23] that found 70% of the patients after surgery have weakness of marginal mandibular branch of facial nerve and recovery of nerve at after one month.
Similar results are reported by [24] in whose study 40% of patients had some degree of postoperative facial nerve dysfunction and agree with study of which compares well with the 30–60% reported incidence postoperative facial nerve dysfunction after parotidectomy [25].
On the other hand, this study disagreed with study [26] after parotidectomy postoperative facial nerve dysfunction occurred in 33.3% of the patients in all branches of facial nerve Regarding gender, proportion of females was higher than males (64% versus 36%) with a male to female ratio of (1:1.7.) no evidence of a difference in incidence between the sexes was reported.
Conclusion
- A transient weakness of marginal mandibular branch of facial nerve in preauricular approach was seen depend on tumor size, position, type, relation of tumor to marginal mandibular branch nerve, long operative time, tight retraction of flap.
- In submandibular surgical approach should be carefully in dissection and retraction because transient weakness in marginal mandibular branch of facial nerve due to nerve elongation cause perineurium tears with disturbance of the interfascicular homeostasis, no disruption of the endoneurium that cause by neural stretching during the dissection neuropraxia or axonotmesis.
- In our study, we adopted certain precautions to lower the incidence of temporary facial nerve paresis. One of these precautions is vertical retraction to reduce the risk of traction injury. Once the nerve trunk was identified we did not use diathermy at all; haemostasis was performed with surgical ligatures (5/0 polygala tin).
References
- Mohajerani H, Esmaeelinejad M, Jafari M, et al. Comparison of Envelope and modified triangular flaps on incidence of dry socket after surgical removal of impacted mandibular third molars: A double-blind, split-mouth study. J Contemporary Dent Practice 2018; 19:836-41.
- Harris MM. Role conflict and role ambiguity as substance versus artifact: A confirmatory factor analysis of house, schuler, and levanoni's (1983) scales. J Applied Psychol 1991; 76:122.
- Kurihashi K, Yanagihara N, Honda Y. A modified Schirmer test: The fine-thread method for measuring lacrimation. J Pediatr Ophthalmol 1977; 14:390-397
- Andreeva A, Howorth D, Brenner SE, et al. SCOP database in 2004: refinements integrate structure and sequence family data. Nucleic Acids Res 2004; 32:D226-9.
- Bae KH, Kang JK, Kim JM. Tunneling or value added? Evidence from mergers by Korean business groups. J Finance 2002; 57:2695-740.
- Kumar VV, Kumar MP, Thiruvenkadaravi KV, et al. Preparation and characterization of porous cross linked laccase aggregates for the decolorization of triphenyl methane and reactive dyes. Bioresource Technol 2012; 119:28-34.
- García-Peñalvo FJ. Technological ecosystems for enhancing the interoperability and data flows. 2018.
- Johnson A, Wang X, Kong F, et al. Object-based evaluation of the impact of horizontal grid spacing on convection-allowing forecasts. Monthly Weather Review 2013; 141:3413-25.
- Schoeff S, Nicholas B, Mukherjee S, et al. Imaging prevalence of sigmoid sinus dehiscence among patients with and without pulsatile tinnitus. Otolaryngol Head Neck Surg 2014; 150:841-6.
- Alayoglu S, Nilekar AU, Mavrikakis M, et al. Ru–Pt core–shell nanoparticles for preferential oxidation of carbon monoxide in hydrogen. Nature Materials 2008; 7:333-8.
- Kamruzzaman M, ElMasry G, Sun DW, et al. Non-destructive prediction and visualization of chemical composition in lamb meat using NIR hyperspectral imaging and multivariate regression. Innovative Food SciEmerging Technol 2012; 16:218-26.
- Tam V, Patel N, Turcotte M, et al. Benefits and limitations of genome-wide association studies. Nature Reviews Gen 2019; 20:467-84.
- Sonne C, Ok YS, Lam SS, et al. First predatory journals, now conferences: The need to establish lists of fake conferences. Sci Total Environ 2020; 715:136990.
- Fuller T, Warren L, Rahman M. Business model innovation in a global digital economy, an anticipatory perspective to researching rural enterprises. 2015.
- Topalian SL, Drake CG, Pardoll DM. Immune checkpoint blockade: A common denominator approach to cancer therapy. Cancer Cell 2015; 27:450-61.
- Santos MI, Araujo-Andrade C, Tymczyszyn EE, et al. Determination of amorphous/rubbery states in freeze-dried prebiotic sugars using a combined approach of near-infrared spectroscopy and multivariate analysis. Food Res Int 2014; 64:514-9.
- Song S, George PM. Conductive polymer scaffolds to improve neural recovery. Neural Regeneration Res 2017; 12:1976.
- Al-Hayani A. Anatomical localisation of the marginal mandibular branch of the facial nerve. Folia Morphol 2007; 66:307-13.
- Collins SE, Eck S, Torchalla I, et al. Decisional balance proportion: Quantifying qualitative data to represent motivation to change among treatment-seeking smokers. Drug Alcohol Dependence 2010; 111:82-8.
- Batstone DJ, Tait S, Starrenburg D. Estimation of hydrolysis parameters in full‐scale anerobic digesters. Biotechnol Bioeng 2009; 102:1513-20.
- Al-Qahtani FS, Zhong C, Alnuweiri HM. Opportunistic relay selection for secrecy enhancement in cooperative networks. IEEE Transactions Communic 2015; 63:1756-70.
- Ferraro Petrillo U, Roscigno G, Cattaneo G, et al. FAST doop: A versatile and efficient library for the input of FASTA and FASTQ files for mapreduce hadoop bioinformatics applications. Bioinformatics 2017; 33:1575-7.
- Sterman DH, Mehta AC, Wood DE, et al. A multicenter pilot study of a bronchial valve for the treatment of severe emphysema. Respiration 2010; 79:222-33.
- Bahrami H, Sadatsafavi M, Pourshams A, et al. Obesity and hypertension in an Iranian cohort study; Iranian women experience higher rates of obesity and hypertension than American women. BMC Public Health 2006; 6:1-9.
- Bron LP, O'Brien CJ. Facial nerve function after parotidectomy. Archives Otolaryngol Head Neck Surg 1997; 123:1091-6.
- Fareed M, Afzal M. Evidence of inbreeding depression on height, weight, and body mass index: A population‐based child cohort study. Am J Human Biol 2014; 26:784-95.
Author Info
Yousif Jabbar Jiheel* and Najwa Jamil Al-Chalabi
Department of Oral and Maxillofacial Surgery, University of Baghdad, IraqCitation: Sabreen Sabah Rasheed, Hussien A Jawad,Evaluation of Facial Nerve Function Following Preauricular and Submandibular Approaches by using the House-Brackmann Facial Nerve Grading System, J Res Med Dent Sci, 2021, 9(7): 197-203
Received: 16-Jun-2021 Accepted: 12-Jul-2021