Review Article - (2021) Volume 9, Issue 12
Evaluation of Perinatal Hypoxic Encephalopathy with Advanced MR Sequences
Imtiyaz Khan1, Nadia Khurshid2*, Irshad Paul3, Feroze Shaheen3 and Mushtaq Bhat4
*Correspondence: Nadia Khurshid, Department of Obstetrics and Gynecology, Government Medical College, Baramulla , Jammu and Kashmir, India, Email:
Abstract
Background
Perinatal hypoxic encephalopathy among important causes of neurological morbidity and mortality in full-term neonates. Identifying ischemic injury clinically usually is difficult in the immediate postnatal period, nonspecific clinical features are present and considerations regarding initiation of active life preserving therapies are needed. MR imaging is the most sensitive and specific imaging technique available for the assessment of perinatal birth asphyxia related brain injury in term-born neonates. This study investigates the utility of MR spectroscopy peak ratios, ADC values along with conventional MRI.
Objectives
To compare the association of encephalopathy following hypoxia in term neonates with proton MRS ratios and ADC values.
Materials and Methods
Conventional MRI (T1 and T2) along with DWI followed by MR Spectroscopy was done in 25 term neonates with clinical and neurological features of encephalopathy following perinatal asphyxia. MRS peak ratios, DWI with ADC values and conventional MRI findings were compared with each grade of HIE.
Results
Among 25 patients suspected cases of hypoxic encephalopathy, 15 patients had early positive conventional MR findings, 16 patients had late positive conventional MR findings, 19 patients had positive DWI, and 22 patients had positive MRS with high lactate/choline and lactate/NAA ratio. Higher association was found between spectroscopy findings and hypoxic ischemic injury compared to MR imaging and ADC.
ConclusionThe combination of MRS, DWI with ADC values and conventional MRI may assist in localizing and predicting the severity of ischemic injury in HIE patients.
Keywords
Perinatal hypoxia, Term, Pre-term, Encephalopathy, HIEIntroduction
Perinatal Hypoxic Ischemic Encephalopathy (HIE), is defined by clinical and laboratory evidence of subacute to acute neurological insult in neonates. It manifests as impairment in initiation and maintenance of respiration, impaired consciousness, depressed reflexes and tone, and occasionally seizures. HIE is among the most compelling factors responsible for neonatal neurological mortality and morbidity resulting in an estimated 23% out of 40 lac worldwide neonatal deaths.
Timely diagnosis of this condition is critical postnatally when consideration for initiation of therapeutic hypothermia may be made. Identification of ischemic brain injury is by clinical examination is often tough and inaccurate at this time, as the clinical features are lack specificity. Numerous modalities for the diagnosis of hypoxic brain injury include electrophysiological tests like amplitude Electroencephalography (EEG), Somatosensory Evoked Potentials (SEP), Brain stem Auditory Evoked Potentials (BAEP) etc. Imaging-wise, MR imaging is the most sensitive and specific imaging modality available for the assessment of hypoxic brain injury secondary to perinatal asphyxia in term-born neonates [1]. Notwithstanding that routine MRI sequences have a lower sensitivity as compared to more recently developed techniques in identifying sequel of a hypoxic insult in neonates within initial hours and days subsequent to the inciting event, these continue to ave a role in excluding other differential diagnoses of perinatal encephalopathy e.g. cerebral infarction, intracranial bleeds, or various malformations. Apparent Diffusion Coefficient (ADC) maps along with corresponding Diffusion Weighted Imaging (DWI) when performed between first to eighth day of life has a higher sensitivity for identifying cytotoxic edema prior to development of abnormal signal intensities on conventional T2, FLAIR or T1 weighted images.
DW imaging becomes “pseudo-normalised” around 7 to 10 days after the hypoxic-ischemic injury which implies a false negative DWI. MRS is a quantitative, non-invasive method of detecting energy metabolism disturbances and quantifies cerebral metabolites levels non-invasively. Its usefulness in early diagnosis of HIE and accurate prediction of adverse outcome has been established especially if performed close to the hypoxic event and has been shown to be more predictive of long-term neurodevelopment outcome than conventional MR and DWI. Utility of 1H MRS for diagnosis of Hypoxic Ischemic Brain injury is well known however comparative analysis of 1H MRS with DWI in assessment of HIE and simultaneous comparison with clinical grades of encephalopathy is a less studied domain, which is the main motive of this study.
Material and Method
This prospective longitudinal study was conducted over 2 years at our institute after proper approval by institutional ethical committee. Term neonates with gestational age ≥ 37 weeks, suspected of having peri-partum hypoxic-ischemic injury and requiring admission for intensive neonatal care were enrolled in the study. Neonates with evidence of central nervous system infections or severe brain malformations were excluded from the study [2]. Parental consent was taken for participation in the study.
Clinical data about Gestational Age, duration and progression of labor, Apgar score at 1 and 5 were obtained from hospital records. MRI Brain was performed within 72 hours (about 3 days) of life and included DWI and MR spectroscopy in addition to routine T1/T2 W sequences in coronal and axial planes. Adequate Sedation was given either by oral chloral hydrate or intravenous midazolam. Ears were adequately protected, pulse rate and oxygen saturation monitoring was done via a transcutaneous pulse oximeter.
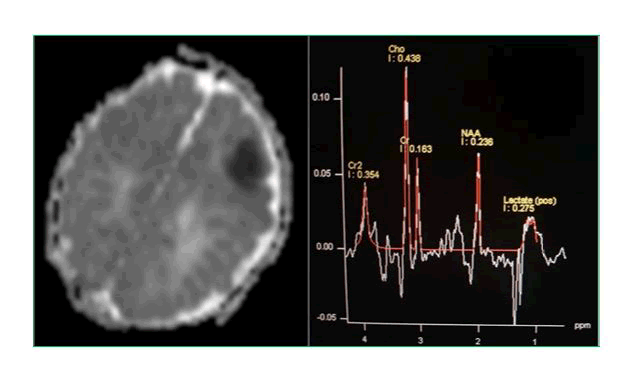
All the imaging was undertaken using a dedicated head coil on 1.5 T MRI systems (Siemens Medical System, Magnetom Avanto). The MR imaging protocol consisted of coronal and axial T2/T1 W sequences, FLAIR, and diffusion weighted imaging (TR=3200ms,TE=99ms). 180x180 mm FOV; 4 mm slice with no interslice gap, b factors of 0, 100 and 1000 sec/sq.mm. Average Apparent Diffusion Coefficient values were calculated on ADC maps at the two locations; putamen and thalamus and anterior and posterior subcortical watershed areas and mean ADC were calculated. ROI were circled with a mean area of 0.18 cm2 (Figure 1).
Figure 1: T1 axial image showing multiple punctate hyperintensities surrounding the ventricle and low signal intensity of corpus callosum. Corresponding MR spectroscopy with a positive lactate doublet peak at 1.3 ppm.
Spectroscopy was performed using 2D chemical shift point resolved spectroscopy. The Field of View (FOV) with voxel size of 7.5 × 7.5 × 15 mm included bilateral talami and basal ganglia as well as fronto–parietal intervascular boundary zone (watershed zone) without bone or CSF contact. Spectral post processing was analyzed on a dedicated application Luise (Siemens Avanto, Medical System). The peak areas were integrated for choline, N-Acetyl Aspartate (NAA), and lactate, and lactate/choline and lactate/NAA peak area ratios were calculated for each voxel. The metabolite ratios of right and left sides were averaged for statistical analysis.
Analysis between clinical and neurophysiological variables with spectroscopy, DWI, and conventional MR was done by Fischer’s exact test or chi square test. Association between clinical Grade of HIE and MRS ratios, DWI scores, ADC ratios, and conventional MR findings were compared by ANOVA test. The adopted significance level was 0.05. All the tests were analysed using statistical software SPSS (version 20.0).
Results
25 neonates (14 males and 11 females) were included in this study with Median Gestational Age of 37weeks 4days and median birth weight of 3200 grams. 17 neonates were born through caesarean section and 8 neonates were born through Normal vaginal delivery. Resuscitation was required in postnatal period in 18 neonates. With respect to encephalopathy grade, 14 were diagnosed with Grade 1, 7 had grade 2, and 4 were diagnosed with grade 3 encephalopathy.
Out of 25 patients who were suspected of hypoxic encephalopathy based on clinical, neurological and laboratory features, 15 patients had early positive conventional MR findings (T1 hyperintensity in basal ganglia/ thalami and watershed zone), 16 patients had late positive conventional MR findings (T1 hyperintensity in basal ganglia/ thalami and watershed zone, with T2 hypointensity), 19 patients had positive diffusion weighted imaging based on diffusion restriction with low ADC values, and 22 patients had positive MRS findings with high lactate/choline and lactate/NAA ratio.
The most common abnormality detected on DWI was diffusion restriction with low ADC values. Variable sized lactate doublet peak centered at 1.31 ppm was the most common finding on MR spectroscopy [3]. The lactate levels on MRS (calculated by lactate doublet integration) correlated closely with clinical severity of HIE.
Patients with central pattern of injury showed greater elevations of lactate in basal ganglia and thalami as compared to watershed zone. Higher lactate levels in the watershed zone as compared to basal ganglia or thalami regions were noted in patients with peripheral pattern of injury. The ratios of peak areas of lactate/NAA and lactate /choline in both basal ganglia and watershed zones were compared with the grade of HIE that showed a significant association with p value of <0.05. MRS didn’t reveal any new metabolite peak in the studied neonates.
Discussion
MRI is diagnostic modality of choice in diagnosis and prognostication of brain injury secondary to perinatal asphyxia in term infants. In addition MRI plays a vital role in identifying patients who may develop ischemic brain damage subsequent to perinatal asphyxia. This study we evaluated full-term infants having perinatal or birth asphyxia in the early neonatal period to assess the spectrum of changes on conventional MRI, DWI, and MR- spectroscopy. Visual analysis was done for T1, T2 W images, and DWI followed by measurement of ADC values and MRS peak ratios in basal ganglia /thalami and watershed zones. ADC values for both basal ganglia and watershed zones were compared with that of MRS peak ratios that showed significant association. Integration of visual evaluation and quantitative MRI data for accurate assessment of neonatal hypoxic- ischemic encephalopathy is the main domain of this study.
Proton MRS spectroscopic measurements were compared with clinical and neurological findings in term neonates with HIE. Similar comparative association was analysed with conventional MRI findings and DWI/ADC images. Combined MR imaging score and ADC showed a better correlation with clinical grades of HIE as compared to MR imaging alone [4]. Association between ADC of basal ganglia and thalami and/or watershed zone with clinical and neurological findings in our study are in agreement with those of several other studies (Figure 2).
Figure 2: ADC image with low ADC level showing infarct in the watershed zone. Corresponding spectroscopy image showing positive lactate peak at 1.33 ppm.
Our study reveals high association between results of proton MRS performed in the early neonatal period and clinical HIE grades of term neonates. Lactate/choline and lactate/NAA ratios were strongly associated with grades of HIE in our study consistent with Cady’s discovery of reduced choline and increased lactate levels in infants with hypoxic- ischemic injury. Lactate levels in HIE brain increases within first 24 hours and continues to remain elevated in subsequent 24 hours likely due to cellular energy failure and continuos anaerobic metabolisation of glucose. Our present data of increased lactate in basal ganglia/watershed zone of patients with HIE (increased lactate/choline and lactate/NAA ratio) is in concordance with several other studies [5]. The results of our study for lactate and NAA are in agreement with recent meta-analysis of MRS studies, indicating that Lactate/NAA is the best possible biomarker for prognostication after HIE. Higher association was found between spectroscopic findings and hypoxic ischemic injury compared to MR imaging and ADC. Although our study was limited with less number of patients, the data support that Proton MRS combined with ADC values performed within the first week of life, can be used to identify high risk neonates who are likely to develop encephalopathy following hypoxic ischemic insult despite having normal conventional MRI findings (Tables 1 and 2) [6].
| HIE | N | Basal Ganglia/Lactate/Choline Ratio | Basal/Ganglia/Thalami ADC Ratio | P-value |
|---|---|---|---|---|
| Grade | ||||
| Normal | 3 | 0.0167 | 1.3000 | 0.002 |
| 1 | 11 | 0.0727 | 1.0509 | |
| 2 | 7 | 0.1514 | 0.9714 | |
| 3 | 4 | 0.5250 | 0.7375 |
Table1: Association of basal ganglia/ thalami lactate/choline ratios with mean ADC values.
| HIE | N | Watershed Zone Lactate/Choline Ratio | Watershed Zone ADC Ratio | P-value |
|---|---|---|---|---|
| Grade | ||||
| Normal | 3 | 0.1633 | 1.9267 | 0.003 |
| 1 | 11 | 0.2582 | 1.1236 | |
| 2 | 7 | 0.1286 | 1.2886 |
Table2: Association of watershed zone lactate /choline ratios with mean ADC values.
References
- Nelson KB, Leviton A. How much of neonatal encephalopathy is due to birth asphyxia? Am J Dis Child 1991; 145;1325-1331.
- Lawn JE, Cousens S, Zupan Lancet Neonatal Survival Steering Team.4 million neonatal deaths: when? Where? Why? Lancet 2005; 365:891-900.
- Hill A. Current concepts of hypox- ic-ischemic cerebral injury in the term newborn. PediatrNeurol 1991; 7:317–325.
- Evans DJ, LeveneMI,Rennie JM et al. Textbook of Neonatology. 3rd ed. Edinburgh: Churchill Living- stone, 1999;1231-1251.
- Barkovich AJ. The encephalopathic neonate: choosing the proper imag- ing technique. AJNR Am J Neuro Radiol 1997; 18:1816-1820.
- acity on anti-sickling activity. South Asian Res J Natural Products 2019; 2:1-16.
Author Info
Imtiyaz Khan1, Nadia Khurshid2*, Irshad Paul3, Feroze Shaheen3 and Mushtaq Bhat4
1Department of Radiology, Government Medical College, Srinagar , Jammu and Kashmir, India2Department of Obstetrics and Gynecology, Government Medical College, Baramulla , Jammu and Kashmir, India
3Department of Radiology, Sher I Kashmir Institute of Medical Sciences, Srinagar, Jammu and Kashmir, India
4Department of Pediatrics, Sher I Kashmir Institute of Medical Sciences, Srinagar, Jammu and Kashmir, India
Citation: Imtiyaz Khan, Nadia Khurshid, Irshad Paul, Feroze Shaheen, Mushtaq BhatEvaluation of Perinatal Hypoxic Encephalopathy with Advanced MR Sequences, J Res Med Dent Sci, 2021, 9(9): 378-381
Received: 01-Dec-2021 Accepted: 15-Dec-2021 Published: 22-Dec-2021