Research - (2022) Volume 10, Issue 2
Evaluation of Stability with Early Loading Utilizing Blx Sla and Slactive Dental Implants: A Clinical Comparative Study
Ahmed Amer Ibrahim* and Thair A Lateef Hassan
*Correspondence: Ahmed Amer Ibrahim, Department of Oral and Maxillofacial Surgery, University of Baghdad, Iraq, Email:
Abstract
Background: The use of a conventional implant loading protocol to replace missing teeth has been recorded for a longer period of time. Through developments in clinical techniques and implant surface modification, the treatment modalities have switched to shortening the healing time after surgery and regaining normal function in order to meet the functional and cosmetic needs of patients. So, many implant companies have designed implants with the intent of achieving a higher level of primary stability to allow for immediate and early loading protocols in which the prosthetic connection is made at the time of implant placement or few weeks after implantation. One of these implant designs is the Straumann bone level X. Aim: Evaluation of the primary and secondary stability of dental implant with early loading utilizing the bone level x (sand blast large grit acid etches) and (modified sand blast large grit acid etch) dental implants. Materials and methods: A total of 20 patients aged from 18-63 years met the eligibility criteria enrolled in this study receiving 40 dental implants. These cases were located into two groups, group A (20 bone level x sand blast large grit acid etch), group B (20 bone level x modified sand blast large grit acid etch). At the time of surgery, the primary stability was checked while secondary stability was measured 12 weeks after early loading of prosthesis. The analysis of results statistically was performed by employing (Wilcoxon signed rank and Mann-Whitney U test.) at P<0.05. Results: Twenty patients 12 females and 8 males’ patients contributed to this study with an average age of 45.7 years. The mean of implant stability quotient values for secondary stability of group A and B was significantly increased as compared with primary stability base line value (68.62 vs. 72.9) (69.42 vs. 73.72) respectively. Conclusion: The study revealed a significant increase in implant stability quotient values of secondary stability when compared with initial base line measurement in both types of dental implants with no clinical difference between the two groups.
Keywords
SLA, SLActive implants, BLX, Early loading, Stability
Introduction
The installation of endosseous dental implants to reestablish lost dentition is a progressively common treatment option for attaining good aesthetic and functional results [1].
Initially, Brå�� nemårk proposed that during a period of 3-6 months, the implants should be submerged and unloaded [2]. Because of this relatively long period, there was a need to adopt another protocol of loading to reduce time. One of these was early loading protocol when the connection of the prosthesis occurs from 2 to 3 weeks after implant placement [3].
Implant stability is considered as a clinical condition of absence of mobility [4]. It is generally divided into primary stability (mechanical engagement) and secondary stability (biological Osseo integration). Primary stability is defined as the firmness that results from mechanical contact between the implant and the bone. Secondary stability is defined as a result of the formation of new bone cells surrounding the biocompatible implant lead to Osseo integration [5].
Many implant manufacturers have designed implants with the goal of having a better level of primary stability [6]. One of these implants designs is the Straumann BLX. This type of dental implants excel by a fully tapered implant, good level of primary stability even in poor bone quality. It is made from the material Roxolid® and according to the surface treatment of dental implant there are two types of BLX dental implant which are BLX sand blast large grit acid etched surface (BLX SLA) and BLX modified sand blast large grit acid etched surface (BLX SLActive) [7].
The SLA surface is formed using a large grit sandblasting technique with corundum particles that generates a macro-roughness on the titanium surface. This is then followed by a strong acid-etching bath at raised temperature for some minutes. The resulting topography offers an ideal structure for cell attachment [8].
The chemically modified sandblasted, large grit, and acid etched surface (SLActive) was introduced in the same way as SLA, but with the addition of rinsing under protective N2 situations and storage in isotonic solution (NaCl), which improved surface chemistry and greatly increased hydrophilic properties, resulting in about 60% more bone growth than SLA implant [9].
Materials and Methods
This clinical prospective comparative study was conducted from January 2021 to November 2021 in the College of Dentistry Teaching Hospital, Department of Oral & Maxillofacial Surgery/Dental Implant Unit/ University of Baghdad and Napoli private dental clinic. The sample registered patients aged ≥ 18 years presented with missing teeth in either maxilla, mandible or both and requested implant supported restoration utilizing Roxolid, BLX SLA or BLX SLActive, Straumann, AG implant. An entire of 20 Iraqi patients aged 18-63 years, 8 males and 12 females encountered the eligibility criteria were registered in this study receiving 40 DI. These cases were located into two groups, group A 20 DI (BLX SLA implant), and group B 20 DI (BLX SLActive implant). For both, the surgical site of DI was inspected for the hard and soft tissue clinically and radiographically by orthopantomography (OPG).
Eligibility criteria
Good general health without any systemic diseases or local conditions that may compromise bone healing potential like heavy smoking, hyperparathyroidism, fibrous dysplasia etc.…. Patient’s age ≥ 18 years of both genders. Partially edentulous maxilla or mandible (short span – one or two teeth loss) dealt with it as a delayed implant placement protocol (at least 6 months after extraction of teeth) and straightforward cases according to SAC clåssificåtion.
Exclusion criteria
If any of the following conditions present, patients were excluded: Current pregnancy, psychosis, or unrealistic expectations, uncontrolled systemic diseases like uncontrolled diabetes, irradiation of the head and neck region or chemotherapy in the previous 5 years, or patients treated with Bisphosphates are all examples of systemic conditions that could interfere with normal healing or inability to withstand surgery. Local conditions such as the presence of acute/chronic infection or poor oral hygiene and local pathological conditions in the implant zone. Advanced and complex cases according to SAC clåssificåtion, and history or clinical evidence of Para functional habits (bruxism or clenching).
Surgical procedure
Local anesthesia of the planned surgical field with Lidocaine 2% (Septodent) commencing one tooth before and after the implantation site using infiltråtion technique was accomplished. The operation of implantation was carried out for both groups by one of two techniques either flåpped or flåpless according to the available criteria and surgeon assessment. Both implant types shared the same drilling protocol that recommended by the manufacturer. The implant bed was prepared with the use of spiral drills with profuse normal saline irrigation and serial drilling technique according to the recommendations of BLX implant system until reaching the requested diameter, as shown in (Figure 1). The implants were introduced by a surgical micro-motor headpiece with a torque of 35 Ncm and speed of 15 rpm, as presented in (Figure 2). With the use of a torque ratchet up to 50 Ncm, DI was manually seated into its finål position. The ISQ was measured immediately utilizing the PenguinRFA device with smartpeg type 38. The measurements were done in buccopalatal and mesiodistal directions and the average was registered, as illustrated in (Figure 3). For the flåpped procedure, interrupted 3/0 braided black silk sutures were used to wound closure. Finally, the gingival former was introduced with the aid of hex driver. The prescribed medications were (Amoxicillin 500 mg+Clavulanic acid 125 mg) 3 times a day for 5 days, and Metronidazole 250 mg tablet 3 times a day for 5 days. Paracetamol 500 mg +Caffeine 65 mg tab is administered as a good choice of pain killer on need. The patients were subjected to the early loading protocol 2-3 weeks following implantation with screw retained restoration in non-functional occlusion, as demonstrated in (Figure 4).
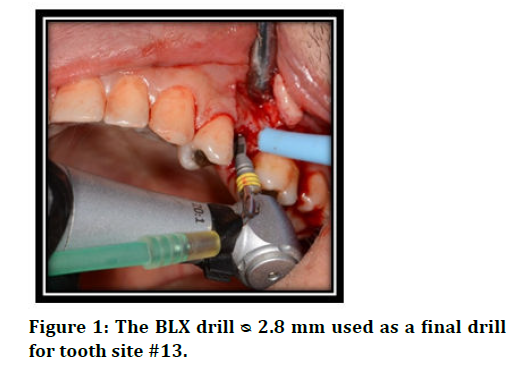
Figure 1. The BLX drill ᴓ 2.8 mm used as a final drill for tooth site #13.
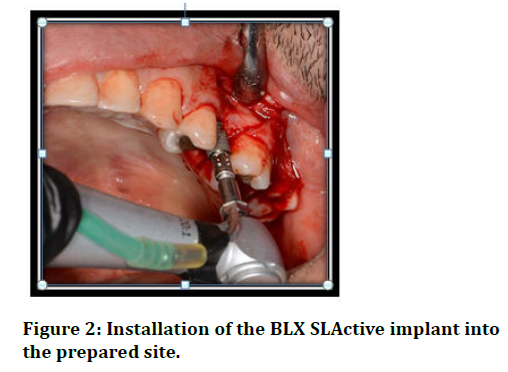
Figure 2. Installation of the BLX SLActive implant into the prepared site.
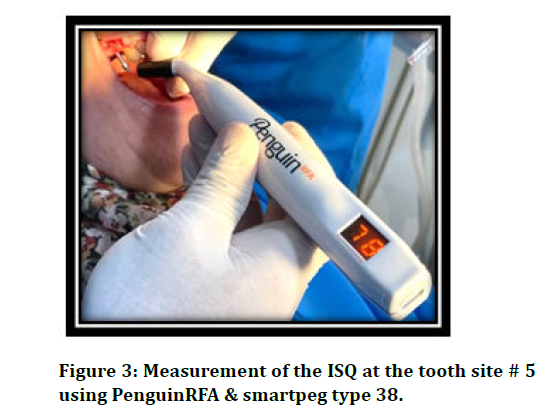
Figure 3. Measurement of the ISQ at the tooth site # 5 using PenguinRFA & smartpeg type 38.
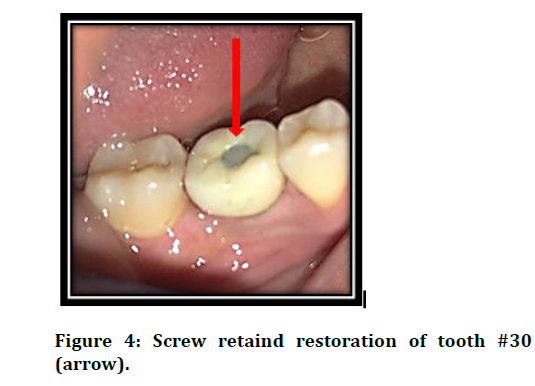
Figure 4. Screw retaind restoration of tooth #30 (arrow).
Follow up and measurement of secondary stability
The screw retained restoration disconnected 12 weeks after loading for measurement of the secondary stability in a similar way as measured previously for the primary one and the screw retained restoration reapplied and tightened by screw driver and ratchet of 35 Ncm torque. A piece of Teflon was placed inside the screw hole and filled with the light cure composite filling material with functional occlusion.
Statistical analysis
Data descriptive and analysis were performed with the use of IBM SPSS (Statistical Package for Social Sciences), software version 26. Wilcoxon signed rank and Mann- Whitney U test were used to test these data. Significånt at P<0.05 not significånt at P>0.05.
Results
Twenty patients contributed to these study 12 females and 8 male’s patients (60% vs 40%) respectively with a female to male ratio of 1.5:1. Those patients aged from 18-63 years with an average of 45.7 years ± 11.92. Age of 50 percentage of patient’s ≤ 45 year. Sixteen DI were installed in maxillary jaws and 24 DI in the mandible. From statistical point of view the mean of ISQ values for secondary stability of group A 12 weeks after loading was significåntly increased as compared with primary stability base line value (68.62 vs 72.90). Also, there was a significånt increase in the mean of ISQ values from primary to secondary stability in group B (69.42 vs. 73.72). This insured that the secondary stability of implants in both groups was significåntly increased, as in (Figure 5) and (Table 1). As well as, there was a significånt difference between the means of this stability of both groups, while there was no significånt difference regarding the primary one. Comparing the means of primary stability with the means of the secondary stability values in females patients and also in patients aged >45 year in both groups a significånt increase in the means of secondary stability value P<0.05 was found. However, there was no significånt change in stability values of DI in males and in patients aged ≤ 45. Also, there was a significånt increase P<0.05 in stability value with DI that were installed in maxillary jaw with SLA DI, and also in mandible with SLActive DI, as documented in (Table. 2). The study registered 100 % survival rate for both groups 15 weeks following surgery for DI managed with early loading.
| Variable | No. of DI | Primary stability ( Base line) mean ± SD | P value | Secondary stability mean ± SD | P Value | P Value |
|---|---|---|---|---|---|---|
| Type of DI | ||||||
| SLA | 20 | 68.62 ± 7.61 | 0.828 | 72.90 ± 2.84 | 0.019 | 0.02 |
| SLActive | 20 | 69.42 ± 7.49 | 73.72 ± 3.52 | 0.005 |
Table 1: Primary and secondary implant stability
| Variable | No. of DI | Primary stability ( Base line) mean ± SD | P Value | Secondary stability mean ± SD | P Value | P Value | |
| Jaw | Type of DI | ||||||
| Maxilla | SLA | 8 | 66.93 ± 6.08 | 0.118 | 71.81 ± 4.11 | 0.114 | 0.049 |
| SLActive | 7 | 71.57 ± 5.10 | 74.64 ± 2.01 | 0.176 | |||
| Mandible | SLA | 12 | 69.75 ± 8.55 | 0.288 | 73.62 ± 1.31 | 0.072 | 0.241 |
| SLActive | 13 | 68.26 ± 8.47 | 73.72 ± 3.52 | 0.01 | |||
Table 2: Correlation of recipient jaw with implant stability
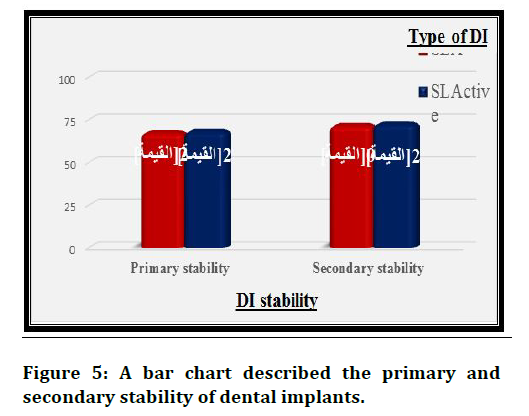
Figure 5. A bar chart described the primary and secondary stability of dental implants.
Discussion
In the current study, the means of ISQ values of secondary stability for both groups (SLA and SLActive) was significåntly increased as compared with the primary stability base line values. Also, there was a significånt difference between the means of secondary stability of both groups, while there was no significånt difference regarding the primary one that is with the same line of Guler et al [10] who reported no significånt differences for the primary stability of both groups. However, SLActive was significåntly higher for the 2nd measurement. The results illustrated a significånt increase in the means of secondary stability values in female patients with both types of DI, while there was no significånt increase in the means of secondary stability value regarding male patients. High ISQ values of female patients may be related to the increased female to male ratio which was 1.5:1 that may have a significånt role in the appearance of this increase related to gender. The explanation is similar to that of Patil et al. [11] who stated that implants with low ISQ values produced marked increase in those values with time than implants with high ISQ values. The study of Boeriu et al. [12] showed a higher ISQ value for the females compared to the ISQ value of male patients which is consistent with current study. Zix et al. [13] reported higher implant stability value in men than in women. Regarding the age, there was a significånt increase in the means of secondary stability values in patients >45 year while it was not in patient’s ≤ 45 year. The researcher didn’t have any logical explication regarding this issue. The result of current study regarding age was incompatible with the opinion of Manolagas et al. [14] who clårified that agerelated bone loss (with increasing age) is predominant in the cancellous compartment because of its underlying mechanisms such as increased oxidative stress which directly control osteoclast activity on the trabecular bone but with limited effect on cortical bone. Negri et al [15] confirmed that this decrease in bone mass has a negative effect on implant stability. Regarding jaws, there was a significånt increase in stability value with SLA DI installed in the maxilla, and also with SLActive DI in the mandible. The study performed by AL-Juboori et al. [16] reported that DI implanted in the lower jaws had higher ISQ values than implants placed in the upper jaws, with ISQ values ranging from 60 to 84 ISQ in the mandible and 53 to 75 ISQ in the maxilla at the time of implant placement and that in agreement with current study results. In this study, it was not necessary to consider every change in the statistical analysis being relevant from the clinical point of view because there is a special criterion that assesses the stability of the DI.
Conclusion
The statistical results revealed a significånt increase in ISQ values of secondary stability when compared with initial base line measurement in both types SLActive & SLA DI. The study demonstrated that ISQ values in female patients significåntly increased in both groups. There was no significånt difference in primary stability between SLA and SLActive implants.
References
- Manzano-Moreno, F., Herrera-Briones, F., Bassam, T., et al. Factors Affecting Dental Implant Stability Measured Using the Ostell Mentor Device. Implant Dent  2015; 24:565-577.
- Sommer, M., Zimmermann, J., Grize, L. et al. Marginal bone loss one year after implantation: a systematic review of different loading protocols. Int J Oral Maxillofac Surg  2020; 49:121-134.
- Resnik R. Misch's contemporary implant dentistry e-book. Elsevier Health Sciences; 2020:33.
- Andreotti, A., Goiato, M., Nobrega, A., et al. Relationship Between Implant Stability Measurements Obtained by Two Different Devices: A Systematic Review. J Periodontol 2020; 88:281-288.
- Kittur, N., Oak, R., Dekate, D.,et al. Dental implant stability and its measurements to improve osseointegration at the bone-implant interface: A review. Materials Today: Proceedings. 2021; 43:1064-1070.
- Cooper, L., De Kok, I., Reside, G., et al. Immediate Fixed Restoration of the Edentulous Maxilla After Implant Placement. JÂ Oral Maxillofac Surg 2005; 63:97-110.
- Kordusky, Benjamin Andrew. Accuracy of BLX and BLT guided implants in the edentulous maxilla: an in vivo study. Graduate Theses, Dissertations, and Problem Reports. 2020; 7544.
- Preshaw, P. Summary of: Implant surface characteristics and their effect on osseointegration. Br Dent J 2015; 218:292-293.
- Nicolau P, Guerra F, Reis R, et al.10-year outcomes with immediate and early loaded implants with a chemically modified SLA surface. Quintessence Int J 2019; 50: 114-124.
- Guler AU, Sumer M, Duran I, et al. Resonance frequency analysis of 208 Straumann dental implants during the healing period. J Oral Implantol. 2013; 39: 161-167.
- Patil, R. and Bharadwaj, D. Is primary stability a predictable parameter for loading implant?. J Int Clin Dent Res Organ  2016; 8:84.
- Boeriu, S. Resonance Frequency Analysis of Dental Implant Stability During the Healing Period (A Clinical Study). Acta Med. Marisiensis 2011; 57.
- Zix, J., Kessler-Liechti, G., & Mericske-Stern, R. Stability measurements of 1-stage implants in the maxilla by means of resonance frequency analysis: a pilot study. Int J Oral Maxillofac Implants 2005; 20.
- Manolagas SC, From estrogen-centric to aging and oxidative stress: A revised perspective of the pathogenesis of osteoporosis. Endocr Rev 2010; 31: 266-300.
- Negri M, Galli C, Smerieri A, et al. The effect of age, gender and insertion site on marginal bone loss around endosseous implants: Results from a 3-year trial with premium implant system. Biomed Res Int 2014; 1-7.
- Al-Juboori MJ, Ab Rahman S, Hassan A, et al. What is the effect of initial implant position on the crestal bone level in flap and flapless technique during healing period?. J Periodontal Implant Sci. 2013; 43: 153-159.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Ahmed Amer Ibrahim* and Thair A Lateef Hassan
Department of Oral and Maxillofacial Surgery, University of Baghdad, Bab-Almoadham, Baghdad, IraqDepartment of Oral and Maxillofacial Surgery, University of Baghdad, Bab-Almoadham, Baghdad, Iraq
Received: 25-Jan-2022, Manuscript No. JRMDS-22-52370; , Pre QC No. JRMDS-22-52370 (PQ); Editor assigned: 27-Jan-2022, Pre QC No. JRMDS-22-52370 (PQ); Reviewed: 10-Feb-2022, QC No. JRMDS-22-52370; Revised: 14-Feb-2022, Manuscript No. JRMDS-22-52370 (R); Published: 21-Feb-2022
