Research - (2023) Volume 11, Issue 1
Feedback Of 2nd Year MBBS Students on Online Teaching Vs Classroom Teaching Methodology in Pharmacology: A Questionnaire Based Study
*Correspondence: Shailja Singh, Department of Pharmacology, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical sciences, India, Email:
Abstract
SARS-CoV-2 (severe acute respiratory syndrome) causing COVID-19 disease, has wreaked havoc in most of the nations all around the globe. Lockdowns of schools were seen in 172 countries in the initial half of the year 2020, compromising the education of about 1.5 billion students/pupils. All healthcare institutions had to close down onsite teaching leading to disruption of training of medical students. Offline teaching which is considered a more traditional style of guidance has been used as the primary modality for instruction for many years but due to pandemic a shift has taken place. In the above mentioned scenario, taking the classes online is the only feasible and most accessible option for continuing medical education/training. There are numerous benefits and drawbacks to this change from offline to online teaching which has been researched by many studies. Aim of the study is to study the perception of 2nd year MBBS students towards online learning versus the conventional offline leaning for the subject of pharmacology during the Cov-2 crisis. Type of study is questionnaire based cross sectional observational study. The locus of study is the Department of Pharmacology, DMIMS. Sample size of the study is100 and the study group is 2nd year MBBS students. The expected outcome of this study is hypothesized to be that students will report satisfaction with online teaching methods with ability to understand and connect the theoretical knowledge taught via recorded/live lectures together but will have trouble understanding practical and clinical knowledge taught via online platform as that requires a higher level of discussion.
Keywords
MBBS students, Feedback, online teaching, classroom teaching
Introduction
SARS-CoV-2 (severe acute respiratory syndrome) causing COVID-19 disease, has wreaked havoc in most of the nations all around the globe, giving rise to issues in many aspects of life. The government's numerous regulations amidst the pandemic have generated a slew of problems in a variety of areas [1].
Lockdowns of schools were seen in 172 countries in the initial half of 2020, compromising the tutoring of about 1.5 billion students/pupil (UN Educational, Scientific and Cultural Organisation, UNESCO 2020) [2]. The necessity to maintain a physical distance has been one of the measures with the biggest impact in controlling escalation of COVID-19. In the field of higher education, its more complex & difficult to carry out this measure while also maintaining the quality of education. Hence all healthcare institutions had to close down onsite teaching which led to disruption of training of medical students. All over the world, clinical rotations were halted as well as inter hospital residency rotations, joint teaching sessions also were stopped till any further notice. Most medical schools also had to delay their examination and postpone their evaluation schedule indefinitely due to the pandemic.
Most of the medical schools weren't prepared for such rapid changes, and most have tried to figure out alternatives to traditional teaching methods like as direct lecture in classes, on-site clinical examinations with direct patient interactions, and clerking. In the above mentioned scenario , taking the classes online is the only feasible and most accessible option for continuing medical education/training.
Offline teaching which is considered a more traditional style of guidance, has been used as the primary modality for instruction for many years. Now due to the changing times, more innovative alternative methods had to be developed which involved technology like online lectures, virtual stimulators, webcasting, video clinical vignettes and online chat rooms. However, in locations where technological advancement is still inadequate and underdeveloped, and online courses must still be continued, such a transfer may take longer, especially since the majority of medical faculty have been channeled and obliged to assist in the hospital and do their duties there to fight against the COVID-19 pandemic [3].
There are numerous benefits and drawbacks to this change from offline to online teaching. Considering the advantages of virtual education, we've discovered that online based formats provide pupils with consistent and seamless access to academic resources, which includes the largest international conferences, at their fingertips and in their favoured environment. In order to participate in offline learning, students had to travel to the training venue, which may be a lecture hall, college, or classroom; however, online learning allows students to participate in training from virtually anywhere in the globe [4,5]. Learning and teaching methods can be enriched by a diverse online education. Network interactions, which are efficient and convenient, can be used to complete teaching management. Furthermore, students could watch class recordings over and over again. But at the same time, one of the disadvantages of online learning is that it may undermine student monitoring, and it is more frequent for students to miss courses and pay less attention to the teachings [6]. This new system includes isolation due to a shift of medical education from offline setting to online setting, this causes problems like ruction in discussion with peers, increase in amount of dependance on emails and issues may arise with need of incessant access to the internet, also due to this integration there could be ill definition of boundaries between work and home. also it may be harder for the elder faculty to adapt to using new technology.
Other disadvantages include a scarcity of real patient interactions, a shortage of one on one peer interactions, shortfall in the technical skillset of the trainers, & exam delays, which has harmed students' motivation to study and has also elevated distress and uncertainty levels, among other things, which has in turn caused serious psychological consequences like dépression as well as anxiety disorders. Modern learning has taken on a different meaning as a result of this transformation (Figure 1) [5].
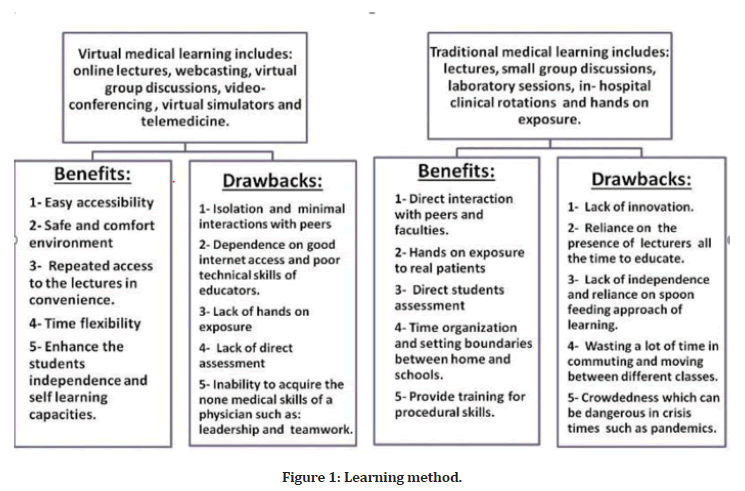
Figure 1. Learning method.
The subject of Pharmacology itself is a continually changing field, with new medications being researched and synthesized all the time and old drugs being phased out. This curriculum provides a solid foundation for MBBS students' future clinical practice. Traditionally, medical schools have used a traditional theory-based and classroom-based methodology for teaching pharmacology, with a greater prominence on possessing factual knowledge about medications [7].
In recent years, undergraduate pharmacology instruction has been transformed by the adoption of novel teaching methods that emphasize supporting learning through small peer-gathering discussions, role plays, technology assisted learning, audio-visual aids, and clinical & community pharmacology research [8,9].
Aim and Objectives
Aim
To study the perception of 2nd year MBBS students towards online learning versus the conventional offline leaning for the subject of pharmacology during the Covid-19 pandemic.
Objectives
To assess the problems faced by students due to the shift to online learning method.
Portray the attitude of the students towards online learning method.
Materials and Methods
Type of study
Questionnaire based cross sectional observational study.
Locus of study
Department of Pharmacology, DMIMS.
Sample size
100.
Study group
2nd year MBBS students.
Study duration
3 months.
Data sources
Answers of responders to the questionnaire.
Study Design
The following steps are included in the study design.
Step 1
Preparation of the synopsis for the research project as per the guide’s instructions in the first contacted session conducted from 29th June 2021.
Step 2
Synopsis submission to be done.
Step 3
Approval of synopsis to be done.
Step 4
Identification of study sample: The sample for this study is 2nd year MBBS students of Jawaharlal Nehru medical college, Datta Meghe institute of medical sciences, Sawangi, Wardha.
Step 5
preparation and validation of questionnaire to be done.
Details of questionnaire
The questionnaire will include closed ended questions only.
Total number of questions are 12.
All 12 questions are closed ended questions
Out of the 12 closed ended questions 10 are multiple choice questions while 2 are dichotomous type of questions.
Care will be taken for the questionnaire to be kept as simple as possible.
Step 6
Interactive sessions on various aspects of online and classroom teaching for the subject of pharmacology to be done.
Utility index: Will be discussed.
Risk benefit profile: Will be explained.
Freedom index: Will be assured.
Confidentiality: Will be assured.
Data collection
This step will be done by distribution of questionnaire and collection of responses of 2nd year MBBS students. The questionnaire itself will be an online type.
Step 7
Analysis of collected data to be done, Multiple-choice set of closed ended questions to be analysed by rating of response-rate.
Formula used for this purpose will be
X1W1+X2W2+X3W3 … XnWn/Total number of samples
Here, X=No. of responses
W=weight of the option
Total number=100
Dichotomous type of close-ended questions to be been analysed by the formula : Z=(Y-π) ÷ square root of π (1- π)/n
Z=Value of opinion (Significant it is >5)
Y=No. of response
π=Null hypothesis ( It will be 50 for sample size of 100)
n=Total number
Observation
Parameters for observation will be the mentioned advantages/disadvantages of virtual learning versus classroom learning in the subject of pharmacology for 2nd year MBBS students during the COVID pandemic.
Expected outcome
The study sample is consisting of second year MBBS students only as they were the ones who experienced teaching of pharmacology via online method. Most of the students are well versed with technical knowledge with at least one device from which they could've attended the classes that were being held online.
The expected outcome of this study is hypothesized to be that students will report satisfaction with online teaching methods with ability to understand and connect the theoretical knowledge taught via recorded/live lectures together but will have trouble understanding practical and clinical knowledge taught via online platform as that requires a higher level of discussion. It is also hypothesized that students will express the need for face-to-face rapport formation and peer interaction/ group discussion.
Discussion
There have been various meta-analysis studies and cross-sectional research examining the effectiveness, preference, and comparison of online and traditional teaching methods since the pandemic first began. An extensive structured review and meta-analysis study which was conducted in 2008 done by Cook et al. Online versus offline learning 76 articles were selected which compared online and offline based interventions and also130 articles which contained no-intervention control for health professional trainees. The conclusion of this study was that when compared to no interventions, internet-based interventions had beneficial impacts, but the consequences and numerical variability’s were often little when compared to offline education.
In a study conducted by Pei L, Wu H seven researches found insignificant distinction between the two educational techniques, whereas 9 articles found considerable advancement in the virtual learning groups. They mention that the fruitfulness of online education is dictated by numerous factors. Directorial challenges, social contact, academic expertise, technical dexterity, motivation of the learner, time and support for academic work, technical problems, money and accessibility to quality uninterrupted internet connection can all be impediments to online learning. Other variables that may contribute to poor online learning include improper design and layout of multimedia assets. According to their findings, there was frequently no substantial difference between online and offline learning for virtual learning that comprised mostly of unvarying, non-interactive learning materials that mirrored traditional classroom learning [10].
Another cross-sectional study by Song Y, Wang S, Liu Y, Liu X, Peng A found a few benefits, which included a lower chance of coronavirus infection due to population flow and the possibility for the students to structure their study time more conveniently and effectively. The following are some of the drawbacks of online education: firstly, objective long distance reduced teacher-student engagement, altered educator’s personal styles and pupil’s attentiveness in class, and made student tuition more difficult to regulate; and secondly long-term usage of electronic items may harm eyesight and overall physical wellbeing. A study by Dost, et al. corroborated the above conclusion. Family distraction (indicated by 26.76 percent of learners) and a poor internet connection (reported by 21.53 percent of learners) were the most frequently mentioned impediments to adopting online education platforms [11].
According to a study by Motte-Signoret, et al. the large number of learners concurred that virtual teaching was an acceptable style of education during the medical crisis, but less than fifty percent of the students expressed that they received schooling of the same quality and effectiveness as compared to traditional classes, and only one-third believed this type of curriculum should be carried on post covid emergency. Learner attendance was often low, with 22 percent to 54 percent of students failing to complete or completing less than half of the online courses. Their study also showed that the medical students were the ones who most strongly opposed or strongly disputed that online and classroom instruction was similar [12].
From the start of medical school, developing right attitude and interpersonal skillfulness to engage with patients, evaluate patient care delivery with coworkers, and display theoretical knowledge and work is a critical skill. Even though video teaching has a lot of potential for engagement in learning of pre-clinical knowledge, there would surely be a gap present in this domain if only online methodology is used [13]. Another study indicated that during the restrictions, pupils found online study to be near to the nature of their educational setting. One of the most significant detrimental effects of the cover crisis on learner’s online learning during the curfew time was the loss of the classroom social interaction and environment [14].
Study by Kyam, et al. discovered relatively low-quality evidence suggesting internet based education is equally successful as conventional classroom learning in the training of medical pupil’s ability to communicate. For communication dexterity and knowledge, mix of digital education is seen to be at least as efficacious as, if not better than, orthodox offline learning. There was no difference found in post-intervention expertness between more engaging and less interactive modes of virtual education, either [15-19].
Conclusion
During the pandemic, there were numerous issues with the implementation of online teaching due to a lack of preparation time and a large number of teaching tasks. The following suggestions may be useful: (1) Maximizing the use of uploaded online courses to minimize wasting educational resources through recording duplication; (2) Optimizing & combining learning software to significantly enhance online learning abilities and environment; and (3) Enhancing teacher-student interaction in online courses.
References
- Khalifa SA, Swilam MM, El-Wahed AA, et al. Beyond the pandemic: COVID-19 pandemic changed the face of life. Int J Environ Res Public Health 2021; 18:5645.
- Ma K, Chutiyami M, Zhang Y, et al. Online teaching self-efficacy during COVID-19: Changes, its associated factors and moderators. Educ Inf Technol 2021; 26:6675-6697.
- Althwanay A, Ahsan F, Oliveri F, et al. Medical education, pre-and post-pandemic era: a review article. Cureus 2020; 12.
- Khan AM, Patra S, Gupta P, et al. Rapid transition to online teaching program during COVID-19 lockdown: Experience from a medical college of India. J Educ Health Promot 2021; 10.
- https://cpduk.co.uk/news/the-key-differences-between-online-learning-and-offline-learning
- Song Y, Wang S, Liu Y, et al. Online education at the medical school of Tongji University during the COVID-19 pandemic: A cross-sectional study. BMC Med Educ 2021; 21:1-6.
- Prasad SR, Ravi H, Santhosh R. A questionnaire based study on student's opinion on the teaching and learning methods in pharmacology in a medical school in India. Int J Basic Clin Pharmacol 2016; 5:2589-2593.
- Hariharan TS. Need for changes in the practical pharmacology curriculum of medical undergraduates. Indian J Pharmacol 2004; 36:181.
- Gitanjali B, Shashindran CH. Curriculum in clinical pharmacology for medical undergraduates of India. Indian J Pharmacol 2006; 38:S108-14.
- Pei L, Wu H. Does online learning work better than offline learning in undergraduate medical education? A systematic review and meta-analysis. Med Educ Online 2019; 24:1666538.
- Dost S, Hossain A, Shehab M, et al. Perceptions of medical students towards online teaching during the COVID-19 pandemic: A national cross-sectional survey of 2721 UK medical students. BMJ Open 2020; 10:e042378.
- Motte-Signoret E, Labbé A, Benoist G, et al. Perception of medical education by learners and teachers during the COVID-19 pandemic: A cross-sectional survey of online teaching. Med Educ Online 2021; 26:1919042.
- Raymond-Hayling O. What lies in the year ahead for medical education? A medical student’s perspective during the COVID-19 pandemic. Med Educ Online 2020; 25:1781749.
- Alghamdi AA. Impact of the COVID-19 pandemic on the social and educational aspects of Saudi university students’ lives. PLoS One 2021; 16:e0250026.
- Kyaw BM, Posadzki P, Paddock S, et al. Effectiveness of digital education on communication skills among medical students: Systematic review and meta-analysis by the digital health education collaboration. J Med Internet Res 2019; 21:e12967.
- Gupta RK, Deogade M. A critical review on ethnobotanical, phytochemical and pharmacological investigations of Martynia annua Linn. Int J Ayurvedic Med 2018; 9:136-143.
- Wadnerwar N, Deogade M. Future perspectives of therapeutic claims of an ethnopharmacological drug ipomoea carnea Jacq.-A critical review. Int J Ayur Med 12:177-84.
- Murray CJ, Abbafati C, Abbas KM, et al. Five insights from the global burden of disease study 2019. Lancet 2020; 396:1135-1159.
- Vos T, Lim SS, Abbafati C, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the global burden of disease study 2019. Lancet 2020; 396:1204-1222.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Department of Pharmacology, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical sciences, Sawangi, Wardha, Maharastra, IndiaReceived: 02-Dec-2022, Manuscript No. JRMDS-22-78473; , Pre QC No. JRMDS-22-78473(PQ); Editor assigned: 05-Dec-2022, Pre QC No. JRMDS-22-78473(PQ); Reviewed: 20-Dec-2022, QC No. JRMDS-22-78473 (Q); Revised: 27-Dec-2022, Manuscript No. JRMDS-22-78473(R); Published: 03-Jan-2023
