Review Article - (2023) Volume 11, Issue 1
Gingival Health Status among Pregnant Women in Urban and Rural Areas in Al-Karkh-Baghdad
Maimonah Tariq Abed* and Nada Jafer MH Radhi
*Correspondence: Maimonah Tariq Abed, Department of Pedodontics and Preventive Dentistry, College of Dentistry, University of Baghdad, Baghdad, Iraq, Email:
Abstract
Background: Pregnancy is a stressful disorder that causes significant changes in metabolic and physiological functions extent. Pregnancy may aggravate inflammatory response of the gingiva to plaque. The impact of systemic circumstances on the host's cellular and immunologic activities appear to be the cause of this altered response, while microbial plaque remains the key causative component. Even in the presence of minimal quantities of plaque, the incidence and severity of gingival inflammation can increase during pregnancy, which is an example of an altered host response due to systematic influences. Increased estrogen and progesterone levels in pregnant women during the third trimester have been linked to increased gingivitis severity by replacing nutritional demands for particular oral bacteria and promoting their proliferation.
Materials and methods: comparative cross sectional study, all women participating in this study were attending the primary health care centers in Baghdad city in AL-Karkh sector, they were with the age ranged from (15-44) years old. The first group consists of all pregnant women attendance seeking dental treatment in urban areas, the second group consists of all pregnant women attendance seeking dental treatment in rural areas. Oral examination and the oral assessment were done according to the World Health Organization WHO (2013). Gingival condition conducted according to Loe and Silness (1963).
Results: The mean value of the gingival index was found to be statistically non-significant differences between pregnant women in urban and rural areas.
Conclusion: The gingivitis was slightly higher in urban than rural pregnant women, but the mild score was reported to be the most common.
Keywords
Pregnant women, Urban, Rural, Gingivitis
Introduction
Pregnancy is a stressful disorder that causes significant changes in metabolic and physiological functions extent [1]. As a result, the most significant physiological and hormonal changes in a woman's life occur during pregnancy [2] and one of the focus areas for these changes is the oral cavity [3]. Hormonal changes caused by fluctuations in estrogen and progesterone levels in the body during pregnancy make women more susceptible to oral infections and gum disorders, which impact not only expecting mothers but also their developing babies [4,5]. Periodontal disease is one of the two major dental diseases that have a high prevalence rate in human populations around the world. Furthermore, it encompasses a series of conditions that are thought to be common in kids, teenagers, and adults. Other factors, such as genetic, neoplastic, traumatic, metabolic and developmental factors, may also contribute to the development of these diseases [6]. There are two types of periodontal diseases: Destructive and nondestructive. Gingival diseases induced by dental plaque: These disorders may emerge on a periodontium with no attachment loss or with stable and not progressive attachment loss as a result of an interaction between the microorganisms present in the dental plaque biofilm and the inflammatory host response, a classic experiment indicating that the poor oral hygiene regularly leads to the emergence of gingivitis within two to three weeks in healthy persons has clearly revealed a cause and effect relationship between microbial plaque and gingivitis. Nonplaque induced gingival lesions is another type of gingivitis: Plaque induced gingivitis is more common than oral symptoms of systemic conditions that cause lesions in periodontal tissues. This category primarily includes gingival lesions that are autoimmune or idiopathic in origin [7]. Pregnancy may aggravate inflammatory response of the gingiva to plaque. The impact of systemic circumstances on the host's cellular and immunologic activities appear to be the cause of this altered response, while microbial plaque remains the key causative component. Even in the presence of minimal quantities of plaque, the incidence and severity of gingival inflammation can increase during pregnancy, which is an example of an altered host response due to systematic influences. Increased estrogen and progesterone levels in pregnant women during the third trimester have been linked to increased gingivitis severity by replacing nutritional demands for particular oral bacteria and promoting their proliferation. Prevotella intermediate, a kind of prevotella, is one species that has been linked to gingivitis during pregnancy. Gingivitis was present in 40% of pregnancies [8-11]. Good gingiva, on the other hand, is said to be unaffected by pregnancy, and is just a response to increased plaque and gingivitis [12]. Many studies have shown that during the second trimester of pregnancy, provetella inter media sub-gingival development increases, possibly causing increased inflammation. Other studies, on the other hand, have shown that the seriousness of the condition gradually worsens until the 36th week of pregnancy, with gingival condition recovers spontaneously after labor [13]. More Iraqi studies found the gingival indices were higher in pregnant women than in non-pregnant women [14-22].
Materials and Methods
Before starting the study, approval was achieved from ethical committee at university of Baghdad, college of dentistry. Verbal consents were obtained from all pregnant women. The present research was carried out between 13th of April and the 8th of September (2021). In this comparative cross sectional study, all women participating in this study were attending the primary health care centers in Baghdad city in AL-Karkh sector, They were with the age ranged from (15-44) years old. The first group consists of all pregnant women attendance seeking dental treatment in urban areas, the second group consists of all pregnant women attendance seeking dental treatment in rural areas. Exclusion criteria include women with systemic diseases, smokers and that receiving any multivitamins, calcium and vitamin D3 supplements. As any questionnaire format, routine questions about personal name, age and trimester are required to take from the pregnant women. Oral examination and the oral assessment were done according to the World Health Organization (WHO) [23]. The Gingival Index (GI) criteria were used for the assessment of gingival condition conducted according to Loe and Silness [24]. This is screening only six index teeth that will be used to represent the whole dentition. For pregnant women, these teeth were the upper right six and two, upper left four, lower left six and two, lower right four. The index teeth were scored on all 4 surfaces (buccal, mesial, lingual and distal).
Results
The sample of present study consists of 140 pregnant women; their ages range (15-44). Most of the interviewed pregnant women (74.3%) aged (15-29) and (25.7%) aged (30-44) with mean age (24.96 ± 0.540) year. They were divided into two groups: First group which consisted of 77 pregnant women in urban area and second group which consisted of 63 pregnant women in rural area. Totally the percentage of pregnant women in urban area was higher than that in the rural area. According to the trimesters: Higher percentage was found in the second trimester, followed by the third, and then the first. The distribution of pregnant women by age, area and trimesters is shown in Figure 1.
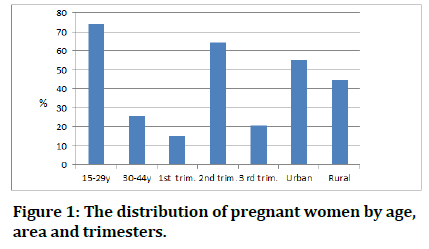
Figure 1: The distribution of pregnant women by age, area and trimesters.
Mean value of gingival index was found to be higher in urban than rural areas and the difference was statistically not significant. While in the urban and total higher mean values of gingival index were found among first trimester, in the rural observed the second trimester get the highest value although there is no significant difference (Table 1).
| Area | 1st trimester | 2nd trimester | 3rd trimester | Total | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | ± SE | Mean | ± SE | Mean | ± SE | F | P value | Mean | ± SE | ||
| Urban | GI | 1.25 | 0.236 | 0.837 | 0.088 | 0.921 | 0.128 | 2.07 | 0.133 | 0.922 | 0.072 |
| Rural | GI | 0.667 | 0.162 | 0.795 | 0.075 | 0.72 | 0.212 | 0.268 | 0.766 | 0.765 | 0.065 |
| Total | GI | 1 | 0.162 | 0.817 | 0.058 | 0.852 | 0.11 | 0.823 | 0.441 | 0.851 | 0.05 |
Table 1: Descriptive and statistical test of GI among trimester by area.
Mostly in all trimesters the gingival index is higher in the urban than rural and there are statistically non significant (p>0.05) (Table 2).
| Pregnancy | Area | ||||||
|---|---|---|---|---|---|---|---|
| Urban | Rural | ||||||
| Mean | ± SE | Mean | ± SE | T test | P value | ||
| 1st trimester | GI | 1.25 | 0.236 | 0.667 | 0.162 | 1.9 | 0.073 |
| 2nd trimester | GI | 0.837 | 0.088 | 0.795 | 0.075 | 0.357 | 0.722 |
| 3rd trimester | GI | 0.921 | 0.128 | 0.72 | 0.212 | 0.863 | 0.396 |
| Total | GI | 0.922 | 0.072 | 0.765 | 0.065 | 1.578 | 0.117 |
Table 2: Descriptive and statistical test of GI among area by trimester.
The severity of gingivitis according to the age and area are as follow: The values of healthy pregnant women are equal, the mild values are higher than those moderate and severe. However, severe type was absent in the age range (30-44) and rural areas (Figure 2). Regarding to the trimester the second trimester get the highest values of healthy, mild and moderate than those other trimesters.

Figure 2: Distribution of GI severity among age, area and trimester.
Discussion
This study looked at pregnant women's gingival health status in urban and rural areas. Oral alterations may arise as a result of physiological changes that occur during pregnancy [11,13]. Pregnancy gingivitis, benign gingival lesions, tooth mobility, erosion, dental caries and periodontitis are all linked to these alterations [25]. Regarding the personal characteristics, more than 70% of pregnant women with a mean age of under 30 years had a mean age of (24.96) years, which matched with the Gupta, et al. and Khalaf, et al. [27,28]. According to the area of residence, the highest proportion of pregnant women was found in the urban area, which conformed to Gaszynska, et al. and Nagi, et al. [29,30]. In reference to the trimester, a higher percentage was found in the second trimester. The increased secretion of gestational hormones (especially estrogen and progesterone) during pregnancy has been linked to pregnancy gingivitis is an increased inflammatory reaction of the gums to bacterial plaque [31]. The immune system, as well as the rate and patterns of collagen production in the gingiva, have been demonstrated to be affected by changes in progesterone and estrogen levels. Both of these conditions impair the body's ability to maintain and repair gingival tissues [32]. In the present study, it was found that the gingival mean value was found to be slightly greater in urban areas than in rural areas. Although statistically non-significant and this study agreed with Siddiqui, et al. [33] and disagreed with other studies where gingivitis was higher in rural than urban pregnant women [25,34]. This may be related to the sample size where the pregnant women in the urban area higher than those in the rural area. Regarding the trimester, the present study reported that the level of gingival index value was higher in the first trimester, contrary results were reported by previous studies where the highest gingival index value was found in the second trimester [17,21,35-38] and this may be related to the dental plaque where increased plaque may be to blame for nausea and vomiting during the first trimester of pregnancy and most pregnant women indicated that teeth brushing was almost impossible, especially in the premolar and molar areas, due to pregnancy related nausea [39].
Conclusion
The present study concluded that the gingivitis was slightly higher in urban than rural pregnant women, but the mild score was reported to be the most common, and this may be an indication of increased awareness of pregnant women in urban and rural areas of the Baghdad governorate.
Conflict Of Interest
No conflicts of the interest.
Ethical Clearance
This study is exempt (no new materials were used).
Acknowledgements
Thank you to everyone who supported me to complete this research.
References
- Soulissa AG. Relationship of pregnancy and periodontal disease. PDGI J 2014; 63:72.
- Laine MA. Effect of pregnancy on periodontal and dental health. Acta Odontologica Scandinavica 2002; 60:257-264. [Crossref][Googlescholar][Indexed]
- Amar S, Chung KM. Influence of hormonal variation on the periodontium in women. Periodontol 2000. 1994; 6:79-80. [Crossref][Googlescholar][Indexed]
- Barak S, Oettinger Barak O, Oettinger M, et al. Common oral manifestations during pregnancy: A review. Obstet Gynecol Surv 2003; 58:624-628. [Crossref][Googlescholar][Indexed]
- Kandan PM, Menaga V, Kumar RRR. Oral health in pregnancy (guidelines to gynaecologists, general physicians and oral health care providers). J Pak Med Assoc 2011; 61:1009. [Googlescholar][Indexed]
- Van Dyke TE, Dave S. Risk factors for periodontitis. J Int Acad Periodontol 2005; 7:3. [Googlescholar][Indexed]
- Carranza F. Newman and Carranza’s clinical periodontology. China: WB Saunders Elsevier, 2019.
- George A, Dahlen HG, Reath J, et al. What do antenatal care providers understand and do about oral health care during pregnancy: A cross-sectional survey in New South Wales, Australia. BMC Pregnancy Childbirth 2016; 16:1-10. [Crossref][Googlescholar][Indexed]
- Pinto GdS, Costa FdS, Machado TV, et al. Early life events and developmental defects of enamel in the primary dentition. Community Dent Oral Epidemiol 2018; 46:511-7. [Crossref][Googlescholar][Indexed]
- Sharma A, Mathur VP, Sardana D. Effective Management of a pregnancy tumor using a soft tissue diode laser: A case Report. Laser Therapy 2014; 23:279-282.
- Silk H, Douglass AB, Douglass JM, et al. Oral health during pregnancy. American family physician 2008; 77:1139-1144. [Googlescholar][Indexed]
- Association AD. Oral health during pregnancy. J Am Dent Assoc 2011; 142:574.
- Boggess KA. Maternal oral health in pregnancy. Obstet Gynecol 2008; 111:976-986. [Crossref][Googlescholar][Indexed]
- Al Najjar SN, Hussein B. Oxidative status among a group of pregnant women in relation to gingival health condition. J Baghdad Coll Dent 2019; 31.
- Al-Guboory I. Evaluation of dental health, Knowledge, attitude and oral health status of pregnant women in Baghdad city. A master thesis, College of Dentistry, University of Baghdad, 1999.
- AL-Sultani HFF. Prevalence and severity of dental caries, periodontal diseases and dental erosion among (20–40) year’s old pregnant women in Hilla city, Babylon governorate-Iraq. Med J Babylon 2013; 10:413-420. [Googlescholar]
- Al-Zaidi W. Oral immune proteins and salivary constituents in relation to oral health status among pregnant women. Ph. D thesis, College of Dentistry, University of Baghdad, Iraq, 2007.
- Baydaa Hussein B. Oxidative status among a group of pregnant women in relation to gingival health condition. J Baghdad College Dentistr 2019; 31:25-30. [Googlescholar]
- Hassan LS. Correlation between periodontal health status and some salivary parameters in pregnancy. College of Dentistry at the University of Baghdad 2013. [Googlescholar]
- Issa Z. Oral health status among groups of pregnant and lactating women in relation to salivary constituents and physical properties. Master thesis submitted to the College of Dentistry, University of Baghdad, Baghdad-Iraq, 2011.
- Mutlak NQ. Selected salivary physicochemical characteristics in relation to oral health status for a sample of pregnant women. University of Baghdad, Iraq, 2016.
- Leka'a S, Ibrahim LaM. Periodontal health status and salivary parameters in pregnancy. J Baghdad College of Dentistry 2014; 26:128-133.
- World Health Organization (WHO). Oral health surveys: Basic methods. 5th edition, 2013.
- Loe H, Silness J. Periodontal disease in pregnancy I. Prevalence and severity. Acta Odontol Scand 1963; 21:533-551. [Crossref][Googlescholar][Indexed]
- Mital P, Agarwal A, Raisingani D, et al. Dental caries and gingivitis in pregnant women. Age 2013; 25:166. [Crossref][Googlescholar]
- Gupta S, Jain A, Mohan S, et al. Comparative evaluation of oral health knowledge, practices and attitude of pregnant and non-pregnant women and their awareness regarding adverse pregnancy outcomes. J Clin Diagn Res 2015; 9:ZC26. [Crossref][Googlescholar][Indexed]
- Khalaf SA, Osman SR, Abbas AM, et al. Knowledge, attitude and practice of oral healthcare among pregnant women in Assiut, Egypt. Int J comm Med Public Health 2018; 5:890-900. [Crossref][Googlescholar]
- Gupta P, Gupta N, Pawar AP, et al. Role of sugar and sugar substitutes in dental caries: A review. ISRN Dent 2013; 2013. [Crossref][Googlescholar][Indexed]
- Gaszynska E, Klepacz Szewczyk J, Trafalska E, et al. Dental awareness and oral health of pregnant women in Poland. Int J Occup Med Environ Health 2015; 28:603-611. [Crossref][Googlescholar][Indexed]
- Nagi R, Sahu S, Nagaraju R. Oral health, nutritional knowledge and practices among pregnant women and their awareness relating to adverse pregnancy outcomes. J Indian Academy Oral Med Radiol 2016; 28:396. [Crossref][Googlescholar][Indexed]
- Ortiz Sanchez BJ, Legorreta Herrera M, Rodriguez Sosa M. Influence of gestational hormones on the bacteria induced cytokine response in periodontitis. Mediators Inflamm 2021; 2021:5834608. [Crossref][Googlescholar][Indexed]
- Hey Hadavi J. Women’s oral health issues: Sex differences and clinical implications. Women’s Health Prim Care 2002; 5:189-199.
- Siddiqui TM, Akram S, Wali A, et al. Dental caries and gingivitis amongst pregnant women: A sample from urban and rural areas of karachi. Pakistan Oral Dent J 2018; 38:88-91. [Googlescholar]
- Karunachandra NN, Perera I, Fernando G. Reply to comment on: Oral health status during pregnancy: Rural urban comparisons of oral disease burden among antenatal women in Sri Lanka. 2012. [Googlescholar][Indexed]
- Al-Najjar SN. Selected salivary antioxidants and lipid peroxidation biomarker in relation to periodontal health condition among a group of pregnant women. Maser Thesis College of Dentistry, University of Baghdad. 2018.
- Mirza KB, Al-Saidy AH, Mohammad CA. The prevalence and severity of periodontal disease in different stages of pregnancy and in women taking oral (contraceptive pills) in Sulaimani City, Kurdistan Region, Iraq. Diyala J Med 2013; 4:61-73. [Googlescholar]
- Salameh R. The periodontal status during pregnancy and intake of contraceptives. A thesis presented to the University of Baghdad for the degree of Master of Science in Periodontics, 2000.
- Suliaman A. Oral health status and cariogenic micro flora during pregnancy. A master thesis, College of Dentistry, University of Baghdad, 1995.
- Gursoy M, Pajukanta R, Sorsa T, et al. Clinical changes in periodontium during pregnancy and post‐partum. J Clin Periodontol 2008; 35:576-583. [Crossref][Googlescholar][Indexed]
Author Info
Maimonah Tariq Abed* and Nada Jafer MH Radhi
Department of Pedodontics and Preventive Dentistry, College of Dentistry, University of Baghdad, Baghdad, IraqReceived: 24-Oct-2022, Manuscript No. JRMDS-22-50875; , Pre QC No. JRMDS-22-50875; Editor assigned: 26-Oct-2022, Pre QC No. JRMDS-22-50875; Reviewed: 09-Nov-2022, QC No. JRMDS-22-50875; Revised: 26-Dec-2022, Manuscript No. JRMDS-22-50875; Published: 03-Jan-2023
