Research - (2019) Volume 7, Issue 6
Marginal Bone Loss around Early Loaded SL Active Implants with Different Retention Means and Antagonist Arches: Clinical Comparative Study
Heba B Mohammed1*, Thair A. Hassan2 and Zainab H. Al-Ghurabi3
*Correspondence: Heba B Mohammed, Department of Oral and Maxillofacial Surgery, College of Dentistry, University of Baghdad, Iraq, Email:
Abstract
Aim: The objective of the present study was to estimate the marginal bone loss (MBL) around early loaded SLActive implants during the first 3 months after loading of the prosthesis with cemented and screw retention means and different antagonist arches using cone beam computed tomography (CBCT).
Materials and Methods: Twelve patients (10 females and 2 males) received 40 SLActive implants inserted with flap and flapless approach and underwent early loading protocol after 8 weeks of healing time, of which 28 DI with screw retention mean. While, 12 DI with cemented retention. Marginal bone loss (MBL) was measured directly by CBCT at the same day of operation and 3 months after loading. Statistical analyses was carried out to study MBL between different retention means and antagonist arches.
Results: No implant was lost during the study follow up appointments with survival rate of 100%. MBL between the cemented and screw retention means showed a statistically no significant difference (pË0.05). On the other hand, MBL significantly decreased (pË0.05) with prosthesis opposing arch.
Conclusion: The findings of this study indicated no differences in MBL between different retention means that may be related to the enhanced osseointegration characteristics of hydrophilic SLActive implant surface and improved bone formation during short period of time.
Keywords
Marginal bone loss, Early loading protocol, Retention mean, SLActive implant
Introduction
The definition of loading protocols has been slightly modified over the years. Early loading of dental implants defined as the occlussal loading of the prosthesis between 1 week and 2 months after implant placement [1]. While, the conventional loading is accomplished with the prosthesis 4 months after implant placement and healing period [2]. Early implant loading protocol have been proposed to reduce the time interval between surgery and the delivery of the prosthetic rehabilitation with the objective of improving patient comfort and satisfaction through the attainment of function and aesthetics during short period of time [3,4] and a favorable implant survival rate by many factors that improves bone healing, facilitates soft tissue shaping and eliminates the need for wearing a removable denture during healing period [3]. In order to determine which loading protocol is most appropriate for a specific patient situation many factors should be considered such as adequate stabilization of the implant, bone quality, implant length, the need for bone agumentation, the time of implant placement and the presence of parafunctional and smoking habits. Primary implant stability is known to be one of the key factors for success associated with placement and loading protocols [5]. Marginal bone level is defined as the distance from the first bone implant contact to the junction of the roughened micro-thread and the smooth beveled implant surface. It was determined at the mesial and distal aspect of the implant [6]. Many studies found that the clinical success of oral implants depends on minimizing the amount of MBL after several years of functional loading [7]. Evaluation of bone stability is essential to ensure optimal long-term results of osseointegrated implants because excessive bone loss can result in periimplantitis which can lead to eventual implant loss. Additionally, the loss of marginal bone height can change the surrounding soft tissue architecture resulting in the loss of interdental papilla which cause esthetic, phonetic changes, food impaction, decreases in inflammatory reactions, load concentrations and bacterial leakage at the implant-abutment interface [8]. The use of CBCT to assess periimplant bone level is more recent as this technology emerged in dentistry only 20 years ago. In comparison with standardized intraoral radiograph, CBCT was found more reliable than periapical and demonstrated more potential in the morphological description of periodontal bone defects. Some of the most influencing parameters are the voxel size and the field of view [6].
Materials and Methods
Twelve patients (10 women and 2 men) with age ranged from 20 to 60 year were enrolled in this study between November 2018 and November 2019 and provided with a written informed consent. This study was approved by the ethical committee of the College of Dentistry, University of Baghdad. The patients were selected without any systemic or local contraindications such as local acute and chronic infections, periodontal disease, parafunctional habits that interfere with surgery or ossiointegeration process. All implantation sites were chosen according to SAC classification (straightforward cases) with sufficient bone height and width and edentulous space in the posterior area of maxilla or mandible, the opposing arch either natural teeth or prosthesis as illustrated in Table 1, to insert 40 SLActive implants (Roxolid, Tapered, Institute Straumann AG, Switzerland), with flapped and flapless approach. The MBL was measured at the time of surgery and 3 months after loading.
Treatment planning
A preoperative orthopantomograph was taken as a standard radiograph for documentation and assessment of the available alveolar bone height taking in consideration the amount of magnification and important anatomical structures and the overall treatment plan was formulated accordingly. The intraoral examination was performed to assesses mouth opening, oral hygiene, periodontal status, evidence of any clinical signs of parafunctional habits, all teeth being inspected for caries and gingival condition. The space analysis of the implant site was done for bone width by using sterile bone caliper.
Surgical procedure
Anaesthesia of the planned surgical field with Lidocaine 2% (Septodent) commencing one tooth before and after the site of implant in maxilla or mandible using infiltration technique. The implant site was exposed either by three sided flap for flapped group or soft tissue punch for flapless one. The preparation of the implant bed was carried out with spiral drills of increasing diameter with copious normal saline irrigation and sequential drilling technique according to implant system recommendations using dental engine hand piece set at 800 (rpm) and torque equal to 35 N/cm. The implants were inserted by a surgical micro motor hand piece with a torque of 35 N/cm and speed 35 rpm as shown in Figure 1. Seating of DI is completed manually into its final position with the aid of a ratchet. Finally, the closer cup is placed according to implant diameter. Wound closer is accomplished utilizing interrupted 3/0 braided black silk sutures.
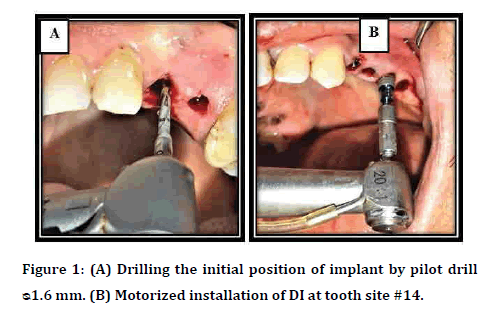
Figure 1: (A) Drilling the initial position of implant by pilot drill ᴓ1.6 mm. (B) Motorized installation of DI at tooth site #14.
For both groups (flapped and flapless surgery) the patients were subjected to CBCT examination with (KAVO OP 3D; Germany) in the same operation day immediately after surgery to determine the marginal bone level as a baseline data be measuring the distance between the apical part of the implant and the margin of the crest in two views (coronal and sagittal) as demonstrated in Figure 2. The patients were allocated to the early loading protocol depending on the measurement of stability values after 8 weeks of implant placement, in which ISQ 57-80 is considered suitable for successful implants [9].
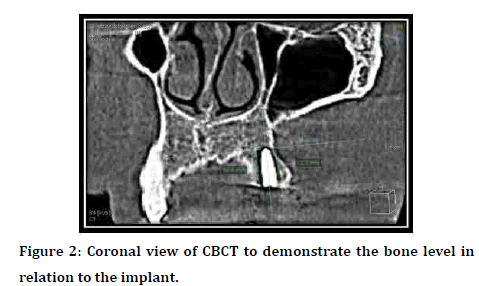
Figure 2: Coronal view of CBCT to demonstrate the bone level in relation to the implant.
Prosthetic procedure
For the impression making closed-tray technique is applied with custom-made trays using the respective impression components of strumman AG, Basel, Switzerland (impression posts) which are selected according to the diameters of the implants. Elastomeric impression material (addation silicons and polyethers) for facilitating impression making with details. The abutments and Zirconium restoration with screw retention were gently tightened to the implant bodies using a manual screwdriver. While cemented one fixed temporarily by temporary cement to facilitate its opening during follow-up appointment after blocking the abutment screw access holes with wax as illustrated in Figure 3.
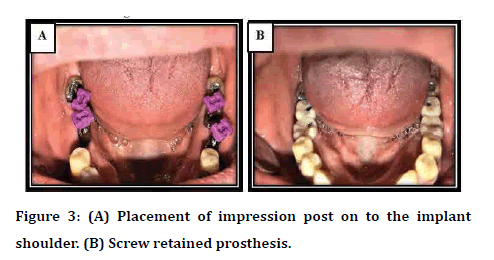
Figure 3: (A) Placement of impression post on to the implant shoulder. (B) Screw retained prosthesis.
Follow up and data collection
Three months after loading of the prosthesis, a standardized CBCT was taken to the patient to evaluate the marginal bone level change. Following that the screw-retained restoration was tightened permanently by wrench ratchet and cemented retained restoration fixed with permanent cement (Resin Modified Glass Ionomer Cement).
Statistical analysis
The data analyzed using Statistical Package for Social Sciences (SPSS) version 25. The data presented as mean, standard deviation and ranges. A level of P˂0.05 was considered significant.
Results
Twelve patients were contributed to this study in which the age ranged from 20-60 years with an average of 46.71 year and standard deviation (SD) of ± 11.36 year. The highest percentage (83.33%) was reported in females. Forty prosthesis were constructed for the survived DI after 8 weeks of the healing period. In this study the prominent figure with each variable was single prosthesis design form (65%). While it has been reported that the screw retention means occupied (70%) of DI. In contrast, concerning the type of opposing arch, natural teeth represented (50%) of them, as illustrated in the Table 1. The results of MBL was not significantly changed (P˃0.05) regarding to age and gender after 3 months of loading. There was a significant decrease (P˂0.05) of the marginal bone level after 3 months in patients with prosthetic opposing arch compared to the baseline data. On the other hand, the results concerning the retention means and prosthetic design illustrated no significant change as demonstrated in Table 2.
| Variable | No. of DI | % |
|---|---|---|
| Type of opposing arch | ||
| Natural | 20 | 50 |
| Prosthesis | 20 | 50 |
| Retention means | ||
| Screw retention | 28 | 70 |
| Cemented retention | 12 | 30 |
| Prosthetic design | ||
| Single | 26 | 65 |
| Splinted | 14 | 35 |
Table 1. Distribution of DI according to prosthetic variables.
Discussion
In the present research, patient’s age ranged between 20-60 years with a mean of (46.71) years and SD of (± 11.36 years). The highest percentage (83.33%) was reported in females. Altinci, et al. [10] and Sener-Yamaner, et al. [7] supported these finding when utilized SLA and SLActive DI in their studies in which the patients aged 26-62 years with an average of 47.2 years, the highest percentage of patients enrolled in this study was in the age group 50-56 years formed 42.85% and 20-65 with a mean age 50 years respectively. There was no significant change of MBL after 3 months in all age group and gender which can be considered as normal remodeling process during ossiointegeration and new bone formation independent on the recipient site or DI dimension. Also, may be related to SLActive implant surface modification to decrease the amount of bone loss. This opinion is supported by Sener-Yamaner et al. [7] who illustrated that the patient’s sex did not have any statistical effect on the mean of MBL. While, this is in disagreement with other studies who demonstrated that postmenopausal women undergo rapid and significant decline in bone mass may be belonged to that after menopause the natural level of estrogen was greatly reduced which is one of the most important factors for osteoblast differentiation from bone marrow osteoprogenitor cells which lead to significant decrease of the bone mass in older female [11,12]. The results of MBL readings related to the retention means and prosthetic design illustrated no significant change in marginal bone loss after this period of time Table 2. This powered by other studies [13,14] who demonstrated no significant differences between cemented and screwed retention prosthesis. In contrast, Nissan et al. [15] observed lower bone loss values for cemented prostheses.8 On the other hand, Hameed, et al. [16] clarified that the screw-retained prosthesis shown greater MBL than cemented retained type. They retained this to the fact that the position of the access opening in the prosthetic restoration transfers occlusal loads in a nonaxial manner which results in increased MBL. There was a significant decrease in MBL in patients with prosthetic opposing arch compared to the baseline data as showed in Table 2. The most important factor for success and failure of implant is the occlusion which differs from the natural teeth and is affected by many factors that may lead to occlussal overload such as location of the implants, the length of cantilever extension, premature contacts, morphology of the prosthesis and design of occlusal scheme which request further studies. This opinion is supported by Alothman, et al. [17] who mentioned in their systematic review that multiple factors can cause occlussal overload on dental implants occlussion. While, this in disagreement with Cid et al. [18] who reported no significant difference in peri-implant bone resorption among different types of antagonists (opposing arch).
| Variables | Baseline Mean ± SD | 3 Months Mean ± SD | p-value |
| Type of opposing arch | |||
| Natural | 10.72 ± 1.3 | 10.75 ±1.1 | 0.8 |
| Prosthesis | 9.95 ± 1.3 | 9.66 ± 1.4 | 0.012 S |
| Retention mean | |||
| Screw retention | 9.94 ± 1.3 | 9.83 ± 1.4 | 0.357 |
| Cemented retention | 11.4 ± 0.75 | 11.2 ± 0.8 | 0.216 |
| Prosthetic design | |||
| Single | 10.1 ± 1.4 | 10.0 ± 1.4 | 0.252 |
| Splinted | 10.7 ± 1.25 | 10.65± 1.2 | 0.455 |
Table 2: Mean of marginal bone loss with prosthetic variables 3 months after loading.
Conclusion
The discoveries of this examination showed no distinctions in MBL between various maintenance implies that might be identified with the upgraded osseointegration attributes of hydrophilic SLActive embed surface and improved bone development during brief timeframe.
References
- Gallucci GO, Benic GI, Eckert SE, et al. Consensus statements and clinical recommendations for implant loading protocols. Int J Oral Maxillofac Implants 2014; 29:287-290.
- Grandi T, Guazzi P, Samarani R, et al. Immediate, early (3 weeks) and conventional loading (4 months) of single implants: Preliminary data at 1 year after loading from a pragmatic multicenter randomised controlled trial. Eur J Oral Implantol 2015; 8:115-126.
- Ganeles J, Zöllner A, Jackowski J, et al. Immediate and early loading of Straumann implants with a chemically modified surface (SLActive) in the posterior mandible and maxilla: 1-year results from a prospective multicenter study. Clin Oral Implants Res 2008; 19:1119-1128.
- Sanz-Sánchez I, Sanz-MartÃÂn I, Figuero E, et al. Clinical efficacy of immediate implant loading protocols compared to conventional loading depending on the type of the restoration: A systematic review. Clin Oral Implants Res. 2015; 26:964-982.
- Schrott A, Riggi-Heiniger M, Maruo K, et al. Implant loading protocols for partially edentulous patients with extended edentulous sites: A systematic review and meta-analysis. Int J Oral Maxillofac Implants 2014; 29:239–255.
- Raes F, Renckens L, Aps J, et al. Reliability of circumferential bone level assessment around single implants in healed ridges and extraction sockets using cone beam CT. Clin Implant Dent Relat Res 2011; 15:661-672.
- Sener-Yamaner ID, Yamaner G, Sertgöz A, et al. Marginal bone loss around early-loaded SLA and SLActive implants: Radiological follow-up evaluation up to 6.5 Years. Implant Dent 2017; 26:392-399.
- De Medeiros RA, Pellizzer EP, Vechiato Filho AJ, et al. Evaluation of marginal bone loss of dental implants with internal or external connections and its association with other variables: A systematic review. J Prosthet Dent 2016; 116:501-506.
- Sachdeva A, Dhawan P, Sindwani S. Assessment of implant stability: Methods and recent advances. Br J Med Med Res 2016; 12:1-10.
- Altinci P, Can G, Gunes O, et al. Stability and marginal bone level changes of SLActive Titanium-Zirconium implants placed with flapless surgery: A Prospective pilot study. Clin Implant Dent Relat Res 2016; 18:1193-1199.
- Negri M, Galli C, Smerieri A, et al. The effect of age, gender, and insertion site on marginal bone loss around endosseous implants: Results from a 3-year trial with premium implant system. Bio Med Research Int 2014; 2014: 369051.
- Chrcanovic BR, Albrektsson T, Wennerberg A. Dental implants inserted in male versus female patients: A systematic review and meta-analysis. J Oral Rehabil 2015; 42:709–722.
- Vigolo P, Mutinelli S, Givani A, et al. Cemented versus screw-retained implant-supported single-tooth crowns: a 10-year randomised controlled trial. Eur J Oral Implanto 2012; 5:355-64
- Crespi R, Cappare P, Gastaldi G, et al. Immediate occlusal loading of full-arch rehabilitations: Screw-retained versus cement-retained prosthesis. An 8-year clinical evaluation. Int J Oral Maxillofac Implants 2014; 29:1406-1411.
- Nissan J, Narobai D, Gross O, et al. Long-term outcome of cemented versus screw-retained implant-supported partial restorations. Int J Oral Maxillofac Implants 2011; 26:1102-1107.
- Hameed MH, Khan FR, Ghafoor R, et al. Marginal bone loss around cement and screw-retained fixed implant prosthesis. Clin Exp Dent 2018; 10:949-54.
- Alothman Y, Ailubli H. Occlusal Considerations in Dental Implantology. EC Dental Science 2019; 18:1872-1883.
- Cid RMO, Stanley K, Cordero EB, et al. Influence of cantilever length and type of arch antagonist on bone loss in total implant supported prosthesis. Acta Odontol Latinoam 2014; 27: 131-136.
Author Info
Heba B Mohammed1*, Thair A. Hassan2 and Zainab H. Al-Ghurabi3
1Department of Oral and Maxillofacial Surgery, College of Dentistry, University of Baghdad, Iraq2Iraqi Scientific Council of Maxillofacial Surgery, Iraqi Board for Medical Specializtion, Iraq
3Department of Oral Diagnosis, College of Dentistry, University of Baghdad, Iraq
Citation: Heba B Mohammed, Thair A Hassan, Zainab H Al-Ghurabi, Marginal Bone Loss around Early Loaded SL Active Implants with Different Retention Means and Antagonist Arches: Clinical Comparative Study, J Res Med Dent Sci, 2019, 7(6):59-.63
Received: 04-Nov-2019 Accepted: 19-Nov-2019
