Case Report - (2022) Volume 10, Issue 5
Omphalocele in Newborn: A Case Report
Madhuri Shambharkar*, Kamini Rodge, Achita Sawarkar, Jaya Khandar, Vaishali Tembhare and Sheetal Sakaharka
*Correspondence: Madhuri Shambharkar, Department of Community Health Nursing, Datta Meghe Institute of Medical Sciences, Wardha, Maharasht, India, Email:
Abstract
Introduction: Omphalocele, commonly known as exomphalos or omphalocele, is an uncommon abdominal wall abnormality. Starting in the sixth week of development, fast gut elongation and increasing hepatic volume restrict an area within the abdomen, pushing loops of intestines exiting the abdominal cavity. Around 15% of live children with omphalocele are affected by chromosome abnormalities.
Clinical findings: Swelling over abdomen, protrusion above umbilicus.
Diagnostic evaluation and blood test: HB-19.4%, Total RBCs Count-5.57 million/cubic mm, Total WBCs Count-22900/cubic mm, Total Platelet Count-2.62/microliter, RDW-17.6%, MCV-105.7%
Peripheral smear: RBCs-Normocytic Normochromic, Platelets-Adequate to smear, TLC-22.9 cells/cu mm, ANC-17.175 cells/cu mm, No band forms seen.
Histopathology report: Omphalocele sac with umbilical cord, Content of omphalocele sac. Operation: Omphalocele repair done.
Therapeutic intervention: Inj. Piptaz 260 mg IVx BD, Inj. Amikacin 40 mg IVx OD, Inj. Mertrogyl 20 mg IVx TDS, Glycerin suppository x TDS.
Outcome: After treatment and surgery, the new-born show improvement. No complaint of hypoglycaemia is seen. No sign of respiratory distress.
Conclusion: This patient was hospitalised in Paediatric ward with an omphalocele and a complaint of protrusion above the umbilical cord. His health began to improve when he received proper therapy that is repair of omphalocele done.
Keywords
Om phalocele, Gut elongation, Omphalocele sac, Umbilical cord protrusionIntroduction
An omphalocele is caused by the occurrence of intestine or because umbilical cord contains other abdominal viscera (such as the stomach and liver).
Exomphalos is one in four thousand newborns and is associated with significant death risk (25%) and severe heart defects (50%) and tube defects (40%) as well as bladder exstrophysis and Beckwith-Wiedemann syndrome. Around 15% of live children with omphalocele are affected by chromosome abnormalities. Around 30% of newborns born with an exomphalos also have other hereditary issues [1].
Omphalocele is thought to affect 2-3 out of every 10,000 pregnancies. During 6 to 10 weeks of pregnancy, a baby’s intestines get longer and push out from the belly into theumbilical cord. The intestines then go back into the belly by week 11. If this does not happen, an omphalocele occurs. An omphalocele can be small, with only some of the intestines outside of the belly, or it can be large or "giant", with many organs outside of the belly [2]. Baby’s with omphalocele have developed other problem like heart defects and other chromosomal abnormalities occur in 30% of children [3] (Figure 1).
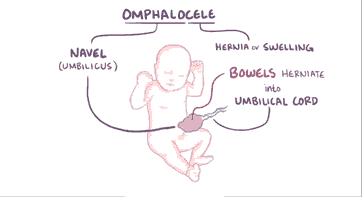
Figure 1: Diagrammatic Representation of Omphalocele.
This condition is occurring due to be a deficiency in the normal physiological umbilical herniation of abdominal content. Targeted prenatal ultrasonography, echocardiography to identify linked deadly heart malformations, and lastly karyotyping, which is frequently connected with chromosomal abnormalities, is the three key diagnostic tests [4]. Complications can arise before, during, or after surgery. Exomphalos can rupture both before and after delivery. For big Omphalocele, there may be liver injuries upon delivery. As a metabolic extract, omphalocele may function, during therapy, to disrupt the nitrogen balance and cause both hypothermia and failures to thrive.
Case Presentation
Patient identification: A male neonates admitted with a complaint of swelling over the umbilicus and fever. A neonate is of 2.6 kg at the time of admission and his length was 48 cm.
Clinical finding: Protrusion above umbilicus seen after birth of baby.
Etiology: During development, Omphalocele is caused by the bowels returning to the abdomen in a twisted state. Omphalocele is thought to be caused by a genetic condition called Edward's syndrome (trisomy 18) or Patau syndrome in some cases (trisomy 13). Omphalocele are another feature of Beckwith- Wiedemann syndrome [4]. Exomphalos is strongly linked to chromosomal abnormalities, which are now being investigated to determine the disease's genetic basis [5].
Physical examination: Baby’s weight was 2.4 kg. Vital signs were normal. There is no other abnormality was found in head to toe examination, instead of abdominal swelling, protrusion above umbilicus. No sign of respiratory distress. The child is lean and thin and having dull look. He was weak.
Diagnostic evaluation: Blood test: HB-19.4%, Total RBCs Count-5.57 million/cubic mm, Total WBCs Count-22900/cubic mm, Total Platelet Count-2.62/ microleter, RDW-17.6%, MCV- 105.7%. Peripheral Smear: RBCs-Normocytic Normochromic, Platelets-Adequate to smear, TLC -22.9 cells/cumm, ANC-17.175 Cells/cumm, No band forms seen. In ultrasonography findings in the sac there was liver attached with herniating content.
Histopathology report
• Omphalocele sac with umbilical cord.
• Content of Omphalocele. Sac measuring 4 cm in length. Received whitish, greyish sac attached to umbilical cord. Single, globular, greyish tissue piece measuring 0.5 cm in length.
Therapeutic intervention: Inj. Piptaz 260 mg IV x BD, Inj. Amikacin 40 mg IV x OD, Inj. Mertrogyl 20 mg IV x TDS, Glycerin suppository x TDS.
Surgical management: The patient underwent surgery after consulting responsible physicians and paediatricians. Repair of Omphalocele was done [6].
Nursing management
Pre-operative
Table 1: Nursing diagnosis: Pain in abdomen related to Omphalocele.
| S. no | Nursing Interventions | Rationale |
|---|---|---|
| 1 | Assess the level of pain then record and report it to doctor. | To know the level of pain and frame further interventions. |
| 2 | Consult and co-ordinate with health care team members of various department included in the case. | To confirm the final diagnosis with staging and prepare nursing diagnosis to provide effective care. |
| 3 | Administer the analgesics as prescribed by the doctors. | To reduce pain. |
Table 2: Nursing diagnosis: Low nutritional pattern less than body requirement related to disease condition.
| S. no | Nursing Intervention | Rationale |
|---|---|---|
| 1 | Monitor the weight of the newborn. | To collect the baseline data. |
| 2 | Insert nasogastric feed to the baby. | To maintain nutrition. |
Post-operative
Table 3: Nursing diagnosis: Acute pain in abdomen related to surgical incision.
| S. no | Nursing Intervention | Rationale |
|---|---|---|
| 1 | Obtain the level of pain on pain-scale | To prepare the post-operative nursing intervention on pain. |
| 2 | Provide comfortable position to the patient. | To induce comfort and rest. |
| 3 | Administer the prescribed medications by the physicians. | To help the patient cure fast and also to reduce pain. |
Table 4: Nursing diagnosis: Risk of infection related to surgical incision and secondary related to low immunity.
| S. no | Nursing Intervention | Rationale |
|---|---|---|
| 1 | Assess the surgical site on every shift further record and report if any pus formation is seen. | To know the wound healing and to check for presence of any infection. |
| 2 | Administer antibiotic as per physician order. | To prevent minimize infection. |
| 3 | Check the physician’s note and apply new dressing on the sutured site. | To prevent infection on the incision site and promote healing. |
Results and Discussion
A male neonate admitted in paediatric ward with chief complaint of swelling over abdomen and protrusion above umbilicus. As soon as he was admitted to hospital investigations were done and appropriate treatment were started. After getting treatment, he shows great improvement. Omphaolcele repaired done. There was no complication before and after the surgical procedure. Patient was discharged from hospital at 12th day and advised the parents for regular follow up.
Deng et al. studied 827 instances of Omphalocele from 1996 to 2006. According to 52.4% of pregnancies ended in late fetal death, with an increased trend in subsequent years, and 37.4% in early new-born death. The frequency of non-isolated Omphalocele (27.9%) was much lower than that of isolated instances (72.1%), indicating a lower occurrence of syndromic features of the defect and corroborating the rarity of our case. Patients with a gestational age of 28-36 weeks had a 2.42 times greater death rate than those with a gestational age of 37-42 weeks, implying that early detection will raise the odds of effective therapy of more cases in less time [6]. Omphalocele can be prevented if the mother will maintain weight and also avoid alocohol and smoking. Omphalocele can be detected in 2nd or 3rd trimester [7]. Abdominal wall defect can be finding out in 10-12 weeks of gestation by doing transvaginal sonography. 3D transvaginal examination helps to detect the condition in early weeks of gestation [8]. Karyotype test is important to find out the birth defect like Omphalocele in the mother of elderly prime or having history of genetic disorder [9].
Most probably karyotype test can be done in first trimester and another in second trimester [10]. In pregnancy and after delivery care is very important also after surgery of omphalocele is very important. Because some fetal characteristics are significantly associated with the perinatal risk of death from omphalocele [11]. After omphalocele repair complications can occur difficulty in breathing, signs of bowel obstruction and fever [12]. Long term problems can occur like damage to abdominal organs, difficulty in digestion and infection also [13].
Conclusion
Omphalocele is an uncommon congenital malformation of the anterior abdominal wall that has a negative impact on infant mortality and quality of life. A timely diagnosis of such a problem is required. The best approach would be with advanced techniques first to terminate the pregnancy or determine the viability of the foetus, followed by the execution of the best treatment programme. But the fact is that there is a lack of trained expert in health profession also lack of awareness in peoples about health. Also lack of diagnostic tools such as advanced ultrasonography examination and genetic screening.
References
- Hartmann Hagen, Wirth Klaus, Klusemann Markus, et al. Analysis of the load on the knee joint and vertebral column with changes in squatting depth and weight load. Sports medi. 2013; 43:993-1008.
- Page Carolyn J, Hinman Rana S, Bennell Kim L, et al. Physiotherapy management of knee osteoarthritis. Int J Rheum Dise 2011; 14:145-151.
- Ayanniyi Olusola, Egwu Roseline F, Adeniyi Ade F, et al. Physiotherapy management of knee osteoarthritis in Nigeria-A survey of selfreported treatment preferences." H k Physioth J 2017; 36:1-9.
- Gupta U, Tiwari P, Kumari R, et al. A report on omphalocele and associated congenital deformity with intrauterine death: Need for early diagnosis. Int J Stud Res 2015; 5:34.
[Crossref][Google Scholar][Indexed]
- Poaty H, Pelluard F, Diallo MS, et al. Omphalocele: A review of common genetic etiologies. Egypt J Med Hum Genet 2019; 20:37.
- Bhatia Dinesh, Bejarano Tatiana, Novo Mario, et al. Current interventions in the management of knee osteoarthritis. J Pharm Bio Sci 2013; 5:30.
- Naryana Cristina Mascarin, Luiz Vancini Rodrigo, Andrade Mara lia dos Santos, et al. Effects of kinesiotherapy, ultrasound and electrotherapy in management of bilateral knee osteoarthritis: prospective clinical trial. BMC Musculoskelet Disord. 2012;13:1-9.
- Hovorakova Maria, Lesot Herve, Peterka Miroslav, et al. Early development of the human dentition revisited. J anat 2018; 233:135-145.
- Andrew Jheon H, Seidel Kerstin, Biehs Brian, et al. From molecules to mastication: The development and evolution of teeth. Wiley Interdiscipl Rev Dev Bio 2013; 2:165-182.
- Sharma D, Murki S, Pratap T, et al. A newborn with omphalocele and umbilical cord cyst: An interesting entity. Iran J Pediatr 2014; 24:449-450.
- Deng K, Qiu J, Dai L, et al. Perinatal mortality in pregnancies with omphalocele: Data from the Chinese national birth defects monitoring network 1996-2006. BMC Pediatr 2014; 14:160.
- Ana Angelova Volponi, Pang Yvonne, Sharpe Paul T, et al. Stem cell-based biological tooth repair and regeneration. Trends cell bio 2010; 20:715-722.
- Anamaria Balic. Biology explaining tooth repair and regeneration: A mini-review. Gerontology 2018; 64:382-388.
Author Info
Madhuri Shambharkar*, Kamini Rodge, Achita Sawarkar, Jaya Khandar, Vaishali Tembhare and Sheetal Sakaharka
Department of Community Health Nursing, Datta Meghe Institute of Medical Sciences, Wardha, Maharasht, IndiaCitation: Madhuri Shambharkar, Kamini Rodge, Achita Sawarkar, Jaya Khandar, Vaishali Tembhare, Sheetal Sakaharka, Omphalocele in Newborn: A Case Report. J Res Med Dent Sci, 2022, 10(5): 47-50.
Received: 23-Feb-2022, Manuscript No. 43823; , Pre QC No. 43823; Editor assigned: 25-Feb-2022, Pre QC No. 43823; Reviewed: 11-Mar-2022, QC No. 43823; Revised: 25-Apr-2022, Manuscript No. 43823; Published: 03-May-2022
