Research - (2022) Volume 10, Issue 1
Ondansetron Attenuates Hypotension Due To Subarachnoid Block-A Randomised Double Blind, Placebo-Controlled Study
Hemanatha Kannan M1, Vijayakumar M Heggeri2* and R Muthu Kumaran3
*Correspondence: Vijayakumar M Heggeri, Associate Professor, Department of Cardiac Anaesthesia, Shri Jayadeva Institute of Cardio Vascular Sciences and Research, Bangalore, India, India,
Abstract
Background: A decrease in arterial blood pressure is one of the known complications of subarachnoid block (SAB) and represents a major cause of concern in some patients. Improvements in surgical and anaesthetic techniques have not helped to curb the incidence of hypotension. Therefore search is going on for various modalities to decrease the incidence. Aim: To test the hypothesis that ondansetron attenuates the arterial hypotension and bradycardia produced due to subarachnoid block. Methods: A randomised double blind, placebo-controlled study was performed on 60 patients. They were divided into two groups. Group O patients received 8 mg ondansetron in 10 ml of isotonic NaCl intravenously before SAB. Group P patients had received isotonic NaCl solution 10 ml intravenously without any added medication before SAB. The systolic (SBP), diastolic (DBP) and mean arterial pressure (MAP) and heart rate (HR) were recorded every 5 minutes for first 20 minutes and every 10 Minutes up to 40 minutes. After the subarachnoid block in both groups and subjected to statistical analysis. The Statistical analysis was performed by STATA 11.1 (College Station TX USA). Students paired t-test was used to assess the significance difference between the pre and post comparisons of heart rate and blood pressures. Continuous variables were expressed as mean and standard deviation; Categorical variables were expressed as frequency and percentage. P<0.05 considered as statistically significance. Results: It was noted that the systolic and diastolic and mean arterial blood pressure fall was less in ondasetron group while comparing to the placebo group. The ondansetron group and the placebo group patients did not have significant effect on heart rate induced by SAB. Conclusion: The attenuation of fall in blood pressure during subarachnoid block can be achieved with ondansetron given intravenously before SAB.
Keywords
Ondansetron, Subarachnoid block, Arterial blood pressure drop, Bradycardia, Surgical procedures
Introduction
Subarachnoid block (SAB) is an efficient method of providing intra-operative analgesia and is a safe alternative to general anaesthesia in many surgical interventions. Despite its numerous advantages, SAB is not without adverse effects, which include unwarranted cardiovascular events. In most cases, these include arterial hypotension and bradycardia, the incidence of which is estimated to reach 33% and13%, respectively, in the nonobstetric population [1,2]. Blockade of sympathetic nerves causes reduction in vascular resistance and a decrease in arterial pressure. Bradycardia is related to relative dominance of the parasympathetic system, increased baroreceptor activity, or to the Bezold-Jarisch reflex (BJR) [1]. The latter is triggered by stimulation of intracardiac receptors, and its consequences include Bradycardia, vasodilatation, and hypotension [3]. Receptors triggering the Bezold-Jarisch reflex are mechanoreceptors located in the heart walls, which participate in systemic responses to hyper- and hypovolemia. They also include chemoreceptors sensitive to serotonin (5-HT3 receptors) [4]. 5-HT3 receptors vary from other serotonin receptors, which are mainly coupled to G-protein. They are ligandgated, fast ion (Na+/K+) channels [5], and activation of the receptors by serotonin or other ligands (phenylbiguanide or 2-methyl-5-HT) results in increased efferent vagal nerve activity [6].
It seems that both types of receptors are involved in the induction of hypotension andbradycardia after subarachnoid blockade. Although mechanoreceptors located in all cardiac chambers are normally sensitive to distension, diminished venous return of blood, as observed after subarachnoid block, induces deformation of the cardiac wall, resulting in irritation of mechanoreceptors and activation of the Bezold- Jarisch reflex. Chemoreceptors are activated by serotonin released from activated thrombocytes [7,8]. Animal studies suggest that serotonin may be an important factor inducing BJR in cases of decreased blood volume [7,9,10], and the mechanism of triggering the reflex depends on activation of peripheral 5-HT3 receptors located in intracardiac vagal nerve endings by serotonin [11]. Yamano et al. demonstrated that 5-HT3 receptor blockade antagonizes BJR induced by serotonin administration in rats [12]. The aim of the present study was to verify the hypothesis that blockade of type 3 serotonin. Receptors by intravenous ondansetron administration would reduce hypotension and bradycardia induced by subarachnoid block.
Materials and Methods
This study was conducted in ASA class I and II patients of both sex aged between 20-70 years undergoing various surgical procedures under SAB. During the period of Aug 2018-Dec 2020. The exclusion criteria included : patient’s refusal, hypersensitivity to ondansetron, history of allergy to local anaesthetic agents, patients with arterial hypertension, coronary heart disease, cardiovascular insufficiency, on anti-hypertensive agents, selective serotonin reuptake inhibitors or serotoninrelated migraine medication, patients on coagulation abnormalities were excluded from the study.Heart rates, non-invasive blood pressure, mean arterial pressure, pulse oximetry, respiratory rate, electro cardiogram were the parameters observed in this study. After Ethical committee approval, fulfilment of inclusion and exclusion criteria and taking informed written consent from patient, the study was conducted as follows. Patients were randomly allocated to either in the ondansetron group (O) and in the placebo (P) group (30 in each group) using sealed envelope technique. A routine preoperative assessment was made on the previous day. Patients were fasted for 10 hrs before anaesthesia and no pre-loading was done before the procedure. Patients were pre medicated 60 mins before anaesthesia with oral midazolam 7.5mg. In the operation theatre the above said monitors were connected, base line values recorded for heart rate, non-invasive blood pressure (Systolic BP, Diastolic BP, Mean arterial pressure). 18 G Intravenous cannula was inserted for I.V. fluid and drug administration. I.V. slow (0.9%) NaCl was started during study period so as not to exceed 200 ml during the entire study period.
I.V. 8 mg ondansetron in 10 ml of isotonic NaCl was given (for ondansetron group) intravenously 5 minutes prior to the performance of the Subarachnoid block. A 3 ml of 0.5% hyperbaric bupivacaine solution was given intrathecally in L3- L4/L4-L5 space by 25/26/27 G QB spinal needle.
I.V. Isotonic NaCl solution 10 ml was given for the placebo group intravenously 5 minutes prior to the performance of the subarachnoid block. A 3 ml of 0.5% hyperbaric bupivacine solution was given intrathecally in L3- L4/L4- L5 space by 25/26/27 G QB spinal needle.
From this moment onwards the level of anaesthesia was evaluated every five minutes till the study period. The person administering the solution was unaware of the content in the syringe.
Heart rate and non-invasive blood pressure values were recorded for every 5 minutes for the 20 minutes and every 10 minutes up to 40 minutes after the SAB and both the groups we compared with the base line values and after Subarachnoid block values.
Surgical procedure including, patient positioning, tourniquet placement and urinary catheterization were not done during study period.
Lumbar puncture was performed with the patient in a sitting position, and the subarachnoid space was punctured at the L3-L4 or L4-L5 level. quicke babcok spinal needle 25-, 26-, or 27-gauge needles were used. After identification of the subarachnoid space (cerebrospinal fluid outflow), 3 mL of 0.5% hyperbaric bupivacaine solution (Spinal 0.5% Heavy; AstraZeneca) was administered. Immediately after completing the subarachnoid injection, patients were positioned supine on the operating table. From this moment on, the level of anesthesia was evaluated 4 times (every 5 minutes) with cold sensation (using alcohol swab). At the same time points, the level of motor blockade was assessed (according to the Bromage scale: 0, no paralysis; 1, inability to lift the thigh [only able to move kneeand feet]; 2, inability to flex the knee [only able to move feet]; 3, inability to move any joint in the legs), and heart rate and arterial pressure were measured. Atropine (0.5 mg intravenously) was administered in cases of bradycardia, and ephedrine (10 mg intravenously) in cases of hypotension, respectively. Medication was individually decided upon by the anesthesiologist participating in the operation.
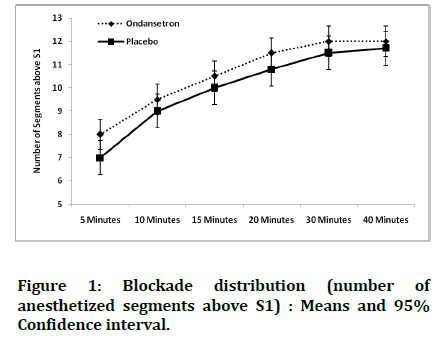
Blockade distribution (number of anesthetized segments above S1) is presented in Figure 1. Numbers of anesthetized segments at respective time points did not differ between the groups. Blockade level increased until the 15-minute time point; statistically significant differences were observed between the levels of analgesia after 5 minutes and at the following evaluation time points, but there were no such differences after 5, 10, 15, 20, 30 and 40 minutes of blockade. Bromage scores of motor block showed no significant differences between the groups at the respective time points. Motor blockade only at level 2 or 3 was noted after 5, 10, 15, 20, 30 and 40 minutes in both groups.
Figure 1:Blockade distribution (number of anesthetized segments above S1) : Means and 95% Confidence interval.
Statistical methods
The Statistical analysis was performed by STATA 11.1 (College Station TX USA). Student-test were performed to assess the significance difference between the age, height, weight, BMI, level of spinal blockade, blood pressure and heart rate with the groups. Students paired t-test was used to assess the significance difference between the pre and post comparisons of heart rate and blood pressures. Continuous variables were expressed as mean and standard deviation; Categorical variables were expressed as frequency and percentage. P<0.05 considered as statistically significance.
Results and Observations
Demographic parameters did not differ significantly. (p> 0.05) for all comparisons. Patient demographic and anthropometric details of the patients are shown in table 1.
| Ondansetron Group | Placebo Group | P-Value | |
|---|---|---|---|
| (n=30) | (n=30) | ||
| Mean ± SD | Mean ± SD | ||
| Age | 32.8 ± 9.9 | 34.8 ± 11.8 | 0.481 |
| Weight | 65.8 ± 9.35 | 63.53 ± 8.1 | 0.326 |
| Height | 158.17 ± 6.6 | 155.6 ± 9.18 | 0.214 |
| BMI | 26.3 ± 3.5 | 26.19 ± 2.38 | 0.932 |
| Body Mass Index | |||
| Normal | 11 (37%) | 11 (37%) | |
| Overweight | 14 (17%) | 18 (3%) | 0.085 |
| Obese | 5 (47%) | 1 (60%) | |
| Gender | |||
| Male | 29 (97%) | 25 (83%) | 0.085 |
| Female | 1 (3%) | 5 (17%) | |
| Type of Surgery Performed | |||
| Hernia Surgery | 9 (30%) | 14 (47%) | |
| Excision of Sac | 7 (23%) | 7 (23%) | 0.064* |
| PerinealSurgeries | 3 (10% | 6 (20%) | |
| ORIF | 5 (17%) | 3 (10%) | |
| Others | 6 (20%) | -- | |
Table 1: Demographic Data (Mean+/_SD).
*Fisher Exact test,ORIF-Open Reduction and internal Fixation All numbers are mean
P value < 0.05 significant
Most of the patients in the study were males. 29 of 30 cases and 25 of 30 control patients were males. Only 1 case was female and 5 controls were females as shown in table.
Most of the patients were overweight (53.3%) followed by normal (36.7 %) and obese patients (10%) as shown in table 3 of distribution of BMI among patients. Larger percentage of patients were from hernia surgeries (38.3%) as this is the most common group of surgery performed under spinal anaesthesia. Rest was followed by excision of sac forming single most common surgery done. Perineal surgery and ORIF were other surgeries done. Distribution of patients according to type of surgery is shown in Table 2.
| Ondansetron | Placebo | P-Value | |
|---|---|---|---|
| 5 Minutes | |||
| Bromage 3 | 5 | 10 | 0.136 |
| Bromage <3 | 25 | 20 | |
| 10 Minutes | |||
| Bromage 3 | 18 | 12 | 0.196 |
| Bromage <3 | 12 | 18 | |
| 15 Minutes | |||
| Bromage 3 | 20 | 22 | 0.779 |
| Bromage <3 | 10 | 8 | |
| 20 Minutes | |||
| Bromage 3 | 25 | 24 | 1.000 |
| Bromage <3 | 5 | 6 | |
| 30 Minutes | |||
| Bromage 3 | 26 | 25 | 1.000 |
| Bromage <3 | 4 | 5 | |
| 40 Minutes | |||
| Bromage 3 | 26 | 25 | 1.000 |
| Bromage <3 | 4 | 5 |
Table 2: Characteristics of the Motor Blockade.
As shown in table 2, The progress of intensity of motor block after 5 minuites of SAB,10 min, 15,20,30and 40 min after SAB was similar in both study groups- group-O and group P.It was found to bestatically not significant. (P>0.05
As shown in figure 1 the height of motor block achieved after SAB was similar in both study groups at 5,10,15,20,30 and 40 min.it was fond to be statistically not significant(P>0.05).
HR, SBP, DBP, MAP at 5 minutes and baseline for both placebo and ondansetron group are compared in table 3.
| Ondansetron Group (n=30) | Placebo Group (n=30) | P-Value | |||
|---|---|---|---|---|---|
| Mean ± SD | P-Value | Mean ± SD | P-Value | P-Value* | |
| Heart Rate (bpm) | |||||
| Baseline | 78.1 ± 16.8 | 79.97 ± 13.47 | 0.636 | ||
| 5 Minutes | 77.67 ± 15.8 | 0.604 | 78.53 ± 13.64 | 0.256 | 0.821 |
| 10 Minutes | 75.97 ± 14.3 | 0.801 | 75.17 ± 15.36 | 0.015 | 0.835 |
| 15 Minutes | 76.8 ± 15.7 | 0.245 | 77.6 ± 15.29 | 0.169 | 0.849 |
| 20 Minutes | 77.07 ± 17.8 | 0.475 | 77.01 ± 15.82 | 0.144 | 1 |
| 30 Minutes | 77.50 ± 15.8 | 0.55 | 79.42 ± 16.2 | 0.898 | 0.459 |
| 40 Minutes | 77.8 ± 15.2 | 703 | 78.5 ± 16.3 | 0.689 | 0.259 |
| Systolic Blood Pressure (mmHg) | |||||
| Baseline | 115.3 ± 8.8 | 116.3 ± 8.8 | 0.662 | ||
| 5 Minutes | 112.2 ± 9.57 | <0.001 | 112.03 ± 10.98 | <0.001 | 0.001 |
| 10 Minutes | 112.9 ± 13.8 | 0.204 | 109.3 ± 9.75 | <0.001 | 0.248 |
| 15 Minutes | 110.37 ± 9.29 | <0.001 | 102.37 ± 8.29 | <0.001 | 0.001 |
| 20 Minutes | 110.17 ± 10.72 | <0.001 | 94.17 ± 11.39 | <0.001 | <0.001 |
| 30 Minutes | 111.4 ± 8.9 | <0.001 | 92.4 ± 8.8 | <0.001 | <0.001 |
| 40 Minutes | 110.5 ± 9.5 | <0.001 | 90.5 ± 8.5 | <0.001 | <0.001 |
| Diastolic Blood Pressure (mmHg) | |||||
| Baseline | 75.3 ± 8.21 | 76.20 ± 9.6 | 0.698 | ||
| 5 Minutes | 70.6 ± 8.6 | <0.001 | 76.6 ± 8.02 | 0.001 | 0.002 |
| 10 Minutes | 69.73 ± 8.89 | <0.001 | 66.1 ± 9.5 | <0.001 | 0.131 |
| 15 Minutes | 67.97 ± 8.39 | <0.001 | 62.6 ± 8.13 | <0.001 | 0.019 |
| 20 Minutes | 68.2 ± 7.84 | <0.001 | 58.47 ± 8.9 | <0.001 | <0.001 |
| 30 Minutes | 68.7 ± 6.28 | <0.001 | 57.89 ± 9.34 | <0.001 | <0.001 |
| 40 Minutes | 68.32 ± 4.30 <0.001 56.57 ±8.80 <0.001 | <0.001 | 56.57 ±8.80 | <0.001 | <0.001 |
| Mean Arterial Blood Pressure (mmHg) | |||||
| Baseline | 87.47 ± 7.73 | 88.23 ± 11.56 | 0.766 | ||
| 5 Minutes | 83.7 ± 8.73 | 87.47 ± 9.05 | 0.69 | 0.005 | |
| 10 Minutes | 83 ± 9.24 | 0.001 | 78.60 ± 8.35 | <0.001 | 0.058 |
| 15 Minutes | 80.77 ± 8.77 | <0.001 | 74.30 ± 8.23 | <0.001 | 0.005 |
| 20 Minutes | 83.63 ± 10.85 | <0.001 | 69.83 ± 9.03 | <0.001 | <0.001 |
| 30 Minutes | 83.24 ± 9.20 | <0.001 | 67.35 ± 8.60 | <0.001 | <0.001 |
| 40 Minutes | 83.13 ± 8.50 | <0.001 | 65.88 ± 7.50 | <0.001 | <0.001 |
| *Between the group Comparisons. P-Value – Intra Group Comparisons | |||||
Table 3: Hemodynamic Changes (expressed as Mean ± SD).
All values are mean
P value < 0.05 significant
The fall in heart rate was not significant between the two groups with p >0.05 as there was no clinically discernable difference in attenuation of heart rate in case group as compared to control group. The fall in systolic and diastolic BP was significantly attenuated in case group when compared to control group with their base line values in the first 5 minutes. The systolic BP reduction was significantly attenuated in case group with p= 0.001. The reduction in diastolic BP was attenuated in case group with p= 0.002. Mean arterial pressure fall was significantly attenuated with p= 0.005 in the case group.
The heart rate, systolic BP, diastolic BP and mean arterial pressure at 10, 15 and 20 minute intervals were compared with their baseline values for both placebo and ondansetron group and shown in table.
All values are mean P value < 0.05 significant
The attenuation in fall of Heart rate was not significant with p=0.84
The attenuation in fall of systolic BP was not significant in study group at 10 minute interval with p=0.24, but significant at 15 and 20 minutes with p <0.05.
Comparison of the heart rate at baseline, 5, 10, 15 and 20 minute showed no significant changes in case and control group when compared to their baseline values as depicted. Changes in the heart rate 5th, 10th, 15th and 20th minute. No significant changes seen between case and control group. The attenuation in fall of heart rate was not significant with p=0.84.Attenuation of fall in systolic blood pressure was significant in case group when compared to control group with the respective base line values, except at 10 min interval P (0.001 to <0.001).
Changes in the SBP at 5th, 10th, 15th and 20th minute.
P value < 0.005 (except at 10 minutes).The attenuation in fall of SBP was not significant in study group at 10 minute interval with p=0.24, but significant at 15 and 20 minutes with p <0.05.Fall in the diastolic blood pressure at 5th, 10th, 15th and 20th minute. Comparison of DBP between case and control group as compared to their baseline studies. Fall in the DBP at 5th, 10th, 15th and 20th minute P value < 0.05 (except at 10 minutes]
Comparison of diastolic blood pressure between case and control group as compared to their baseline studies showed significant attenuation of BP fall (p< 0.05) except at 10 min (p=0.13).
Mean arterial pressure among case and control group, shows significant attenuation of BP fall in case group (p <0.05) showing the effect of ondansetron in attenuation of BP fall by spinal anaesthesia to be significant when compared to placebo. Changes in the Mean Arterial Pressure at 5th, 10th, 15th and 20th minute.
P value < 0.05
Discussion
The major finding in the present study is the observation of decreased fall in the systolic, diastolic and mean blood pressures in patients who were given 8 mg intravenous ondansetron before SAB, as compared to those patients who received placebo. Fall in arterial pressure accompanying subarachnoid blockade is a common side effect. Hemodynamic changes due to SAB are generally benign; however, occasionally, they may lead to serious complications, including cardiac arrest. Moreover, hypotension is not desirable in patients with ischemic heart disease or those with cerebrovascular insufficiency. It is worth noting that the mechanisms of hypotension in SAB may be different than those producing severe Bradycardia and cardiac arrest. Hypotension is due to a decrease in systemic vascular resistance and filling pressure, due to sympathetic blockade and redistribution of blood in the intravascular compartments. Bradycardia is due to the consequence of Bezold- Jarisch reflex and activation of baroreceptor reflex. It is al so likely that parasympathetic predominance may produce hypotension and bradycardia [13-15]. To combat the cardiovascular side effects of SAB, the following methods are recommended preloading with intravenous fluid infusion, use of vasoconstrictors,head-downposition and administration of anti-cholinergic drug such as atropine [16-18]. There are reports which suggest the cardiovascular side effect of SAB result from stimulation of 5-HT3 receptors in vagal nerve endings [19-26]. This study was aimed to look at the influence of pre-treatment with ondansetron on the incidence of hypotension caused by SAB. Martinek described a case of cardiac arrest in asystole during SAB, which was successfully treated with intravenous ondansetron and atropine [7]. Tsikouris et al. found that granisetron, a 5-HT3 receptor blocker, diminishes heart rate fluctuations occurring during the course of the head-up tilt table test, which might be related to the BJR. In the present study, ondansetron was effective in attenuating hypotension due to SAB; this effect was evident on SAP, DAP and MAP and did not result in significant changes in HR.. Serotonin is known to influence systolic activity of the heart, but through the binding to 5-HT4 receptors [27]. Blauw et al. showed in healthy volunteers, that infusion of serotonin in to the radial artery was associated with vasodilatation and this effect was inhibited by 5-HT3 antagonists, (tropisetron) [28-30]. Current indication for use of serotonin receptor blockers include prevention and in the treatment of post-operative nausea and vomiting [31], and for prevention of shivering in patients undergoing SAB [32]. In this report, how have concluded that pre-treatment with ondansetron decreases the extent of hypotension (SBP, DBP and MAP) Owczuk, et al demonstrated that the use of ondansetron did not have any impact on DAP, but our study demonstrated the maintenance of all the three SBP, DBP and MAP after subarachnoid blockade [33,34].
Conclusion
We recommend that ondansetron 8mg IV can be administered before spinal anaesthesia to attenuate hypotension. More studies regarding role of 5 HT3 receptors in maintaining of blood pressure should be conducted. Mechanism of Bezold Jarisch reflex has to be studied further. Ondansetron can be used for its antiemetic effect during anaesthesia to prevent aspiration. Ondansetron can be made as a part of protocol during spinal anaesthesia in patients precluding fluid overload.
References
- Liu SS, McDonald SB. Current issues in spinal anesthesia. Anesthesiol 2001; 94:888-906.
- Carpenter RL, Caplan RA, Brown DL, et al. Incidence and risk factors for side effects of spinal anaesthesia. Anaesthesiol 1992; 76:906-916.
- Campagna JA, Carter C. Clinical relevance of the Bezold-Jarisch reflex. Anaesthesiol 2003;98:1250-1260.
- Aviado DM, Guevara Aviado D. The bezold-jarisch reflex. A historical perspective of cardiopulmonary reflexes. Ann NY Acad Sci 2001; 940:48-58.
- Gyermek L. Pharmacology of serotonin as related to anaesthesia. J Clin Anesth 1996; 8:402-425.
- Villalón CM, Centurión D. Cardiovascular responses produced by 5-hydroxytriptamine: A pharmacological update on the receptors/mechanisms involved and therapeutic implications. Naunyn schmiedebergs. Arch Pharmacol 2007; 376:45-63.
- Martinek RM. Witnessed asystole during spinal anaesthesia treated with atropine and ondansetron: A case report. Can JAnaesth 2004; 51:226-230.
- Mao HZ, Li Z, Chapleau MW. Platelet activation in carotid sinuses triggers reflex sympathoinhibition and Hypotension. Hypertension 1996; 27:584-590.
- Veelken RO, Sawin LL, DiBona GF. Epicardial serotonin receptors in circulatory control in conscious Sprague-Dawley rats. Am J Physiol Heart Circ Physiol 1990; 258:466-72.
- Veelken R, Hilgers KF, Leonard M, et al. A highly selective cardiorenal serotonergic 5-HT3-mediated reflex in rats. Am J Physiol 1993; 264:1871-1877.
- Yamano M, Ito H, Kamato T, et al. Characteristics of inhibitory effects of serotonin (5-HT) 3-receptor antagonists, YM060 and YM 114 (KAE-393), on the von bezold-jarisch reflex induced by 2-methyl-5-HT, veratridine and electrical stimulation of vagus nerves in anesthetized rats. Jap J Pharmacol 1995; 69:351-6.
- Yamano M, Kamato T, Nishida A, et al. Serotonin (5-HT)3 receptor antagonism of 4,5,6,7-tetrahydrobenzimidazole derivatives against 5-HT-induced bradycardia in anesthetized rats. J Pharmacol 1994; 65:241-248.
- Pollard JB. Cardiac arrest during spinal anaesthesia: common mechanisms and strategies of prevention. Anesth Analg 2001; 92:252-256.
- Kopp SL, Horlocker TT, Warner ME, et al. Cardiac arrest during neuraxial anaesthesia: frequency and predisposing factors associated with survival. Anesth Analg 2005; 100:855-865.
- HanssR, BeinB, WeselohH, et al. Heart rate variability predicts severe hypotension after spinal anaesthesia. Anaesthesiol 2006; 104:537-545.
- Kinsella SM, Tuckey JP. Perioperative bradycardia and asystole: Relationship to vasovagal syncope and the Bezold–jarisch reflex. Br J Anaesth 2001; 86:859-68.
- Lim HH, Ho KM, Choi WY, et al. The use of intravenous atropine after a saline infusion in the prevention of spinal anesthesia-induced hypotension in elderly patients. Anesth Analges 2000; 91:1203-6.
- Tsikouris JP, Kluger J, Chow MS, et al. Usefulness of intravenous granisetron for prevention of neurally mediated hypotension upon head upright tilt testing. Am J Card 2000; 85:1262-4.
- Matzen S, Secher NH, Knigge U, et al. Effect of serotonin receptor blockade on endocrine and cardiovascular responses to head‐up tilt in humans. Acta Physiol Scand 1993;149:163-76.
- White CM, Chow MS, Fan C, et al. Efficacy of intravenous granisetron in suppressing the bradycardia and hypotension associated with a rabbit model of the bezold‐jarisch reflex. J Clin Pharmacol 1998; 38:172-7.
- Bagchi S, Deshpande SB. Indian red scorpion (Buthus tamulus) venom-induced augmentation of cardiac reflexes is mediated through the involvement of peripheral 5-HT3 and central 5-HT1A receptor subtypes. Toxicon 1999; 37:1697-709.
- Heyman JS, Young ML, Bagshaw RI, et al. Cardiovascular stability with rapid intravenous infusion of ondansetron. Can J Anaesthe 1993; 40:448-52.
- Faerber L, Haus U, Späth M, et al. Physiology and pathophysiology of the 5‐HT3 receptor. Scand J Rheumatol 2004; 33:2-8.
- Charbit B, Albaladejo P, Funck-Brentano C, et al. Prolongation of QTc interval after postoperative nausea and vomiting treatment by droperidol or ondansetron. J Am Soc Anesthesiolo 2005; 102:1094-100.
- Kasinath NS, Malak O, Tetzlaff J. Atrial fibrillation after ondansetron for the prevention and treatment of postoperative nausea and vomiting: a case report. Can J Anaes 2003; 50:229-31.
- Bosek V, Hu P, Robinson LA. Acute myocardial ischemia after administration of ondansetron hydrochloride. J Am Soc Anesthesiol 2000; 92:885.
- Kaumann AJ, Levy FO. 5-hydroxytryptamine receptors in the human cardiovascular system. Pharmacol Therapeu 2006; 111:674-706.
- Blauw GJ, van Brummelen P, Chang PC, et al. 5HT3 receptor-mediated vasodilation in the human forearm. J Hypertens 1988; 6:33-35.
- Grubb BP, Karas BJ. The potential role of serotonin in the pathogenesis of neurocardiogenic syncope and related autonomic disturbances. J Interven Cardi Electrophysiol 1998; 2:325-32.
- Simpson KH, Murphy P, Colthup PV, et al. Concentration of ondansetron in cerebrospinal fluid following oral dosing in volunteers. Psychopharmacol 1992; 109:497-8.
- Ho KY, Gan TJ. Pharmacology, pharmacogenetics, and clinical efficacy of 5-hydroxytryptamine type 3 receptor antagonists for postoperative nausea and vomiting. Curr Opin Anesthesiol 2006; 19:606-11.
- Kelsaka E, Baris S, Karakaya D, et al. Comparison of ondansetron and meperidine for prevention of shivering in patients undergoing spinal anesthesia. Reg Anesth Pain Med 2006; 31:40-5.
- Hartmann B, Junger A, Klasen J, et al. The incidence and risk factors for hypotension after spinal anesthesia induction: An analysis with automated data collection. Anesth Analg 2002; 94:1521-9.
- Owczuk R, Wenski W, Polak-Krzeminska A, et al. Ondansetron given intravenously attenuates arterial blood pressure drop due to spinal anesthesia: a double-blind, placebo-controlled study. Regional Anes Pain Med 2008; 33:332-9.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Hemanatha Kannan M1, Vijayakumar M Heggeri2* and R Muthu Kumaran3
1Consultant Cardiac Anaesthiologist and Intensivist, Dr. Kumaran Multispeciality, Pondicherry, India, India2Associate Professor, Department of Cardiac Anaesthesia, Shri Jayadeva Institute of Cardio Vascular Sciences and Research, Bangalore, India, India
3Director, Dr. Kumaran Multispeciality Hospital, Puducherry, India, India
Citation: Hemanatha Kannan, Vijayakumar M Heggeri,Ondansetron Attenuates Hypotension Due To Subarachnoid Block-A Randomised Double Blind, Placebo-Controlled Study, J Res Med Dent Sci, 2022, 10(1): 364-370
Received: 10-Dec-2021, Manuscript No. Jrmds-21-44366; , Pre QC No. Jrmds-21-44366 (PQ); Editor assigned: 13-Dec-2021, Pre QC No. Jrmds-21-44366 (PQ); Reviewed: 27-Dec-2021, QC No. Jrmds-21-44366; Revised: 04-Jan-2022, Manuscript No. Jrmds-21-44366 (R); Published: 06-Jan-2022