Case Report - (2022) Volume 10, Issue 7
Orthodontic Therapy as an Adjunct to Prosthetic Rehabilitation for Restoring Esthetics and Function: An Interdisciplinary Case Report
Akanksha Kumar1*, Apurv Mamidwar2, Narendra Sharma3, Ranjit Kamble3, Sunita Shrivastav3 and Shriya Murarka3
*Correspondence: Akanksha Kumar, Department of Orthodontics and Dentofacial Orthopaedics, Swargiya Dadasaheb Kalmegh Smruti Dental College and Hospital, Nagpur, Maharashtra, India, Email:
Abstract
Introduction: Patients seeking replacement of missing teeth in the esthetic zone alongwith any co-existing malocclusion often present a formidable challenge and call for an interdisciplinary approach for achieving results that are both functionally and esthetically acceptable and stable. For comprehensive oral rehabilitation, pre-prosthetic orthodontics can successfully improve the prognosis of restorative treatment and optimize the outcome. In these cases, thorough communication between the Orthodontist and the Prosthodontist is essential in order to make a prudent decision for the benefit of the patient and establish their treatment objectives.
Case description: This case report describes the management of a 17 years old male patient with three missing maxillary incisors treated with a combined orthodontic-prosthodontic interdisciplinary approach utilizing customized modifications in the treatment mechanics including bracket substitutions, premolar extractions, determination and redistribution of space for adequate prosthetic replacement, incorporation of riding pontic and lateralization of canines to facilitate the final definitive prosthesis in achieving the desired functional and esthetic goals.
Conclusion: The case was finished with definite enhancement in macro, mini and micro-esthetics with optimal functional occlusion.
Clinical significance: This case emphasizes the significance of detailed adjunctive orthodontics in such integrated protocols to bring about considerable improvement and efficiency in treatment results.
Keywords: Pre-prosthetic Orthodontics, Canine lateralization, Interdisciplinary treatment, Adjunctive Orthodontics, Riding pontic, Bracket substitution
Introduction
Dental trauma, especially to the anterior, can cause significant aesthetic and functional problems, which in turn have a major negative impact on the psychosocial wellbeing of patients affecting their self-esteem and confidence [1].
The case becomes even more demanding when it is accompanied by space loss and inter-arch malocclusions, wherein adequate space is not present for the prosthesis to replace all the missing teeth and neither does it permit entire space closure by orthodontics alone. Such patients often present a complex and challenging task of rehabilitation, thus necessitating a comprehensive team approach with more than one speciality to be involved [2]. Also emphasis has to be given towards long-term stability of results while aiming to accomplish favourable esthetics, functional requirements and periodontal tissue health [3]. Hence, diagnosis and treatment planning in these cases always benefit by integrating a symbiotic interdisciplinary approach that offers an all-inclusive method for the achievement of the best possible treatment outcomes [4].
This article aims to emphasize the significance of pre-prosthetic and adjunctive orthodontics in such interdisciplinary protocols in treating a patient with multiple missing anterior teeth.
Case Presentation
A 17 years old male patient reported to the department of prosthodontics with the chief complaint of unpleasant smile esthetics and presence of gap due to missing teeth in the upper front region of the jaw. His medical history was non-contributory. He gave a past dental history of extraction of maxillary anterior teeth 8 years back, following trauma due to a fall from bicycle. The clinical evaluation revealed that a direct prosthetic approach will not result in the achievement of desirable function and esthetics. The patient was thus referred for an Orthodontic consultation.
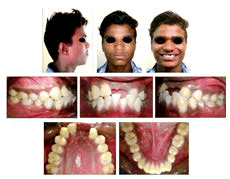
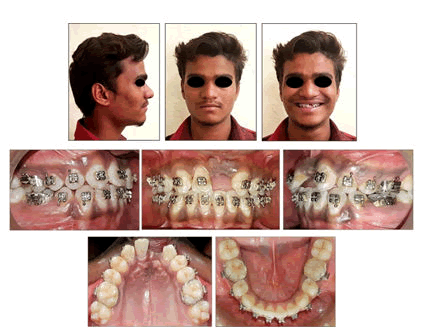
On extraoral examination, the patient had a symmetric mesoprosopic face, convex facial profile with competent lips (Figure 1).
Figure 1: Pre-treatment facial and intraoral photographs of 17 years old male patient with missing 11, 21 and 22.
Smile line was low and non-consonant. Intraoral examination revealed angles class I molar relationship bilaterally and 2 mm class II canine relationship on the left side. Maxillary right and left central incisors and left lateral incisor (11, 21 and 22) were missing and right lateral incisor (12) was proclined. Space of 14 mm was present between maxillary right lateral incisor (12) and left canine (23). In the mandibular arch, crowding was present along with proclined and extruded incisors. Ellis class II fracture was seen with mandibular left central incisor (31) with about half of its coronal structure remaining. Vitality testing showed no evidence of pulpal involvement with 31. Mandibular dental midline was deviated to the left by 2 mm. Over jet was reduced and cross-bite was present with 23. The gingival health was satisfactory and an adequate band of attached gingiva was seen. The path of closure of mandible was normal without any deviation and there were no associated signs or symptoms of temporomandibular disorder.
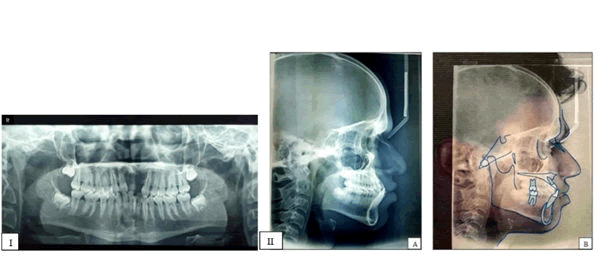
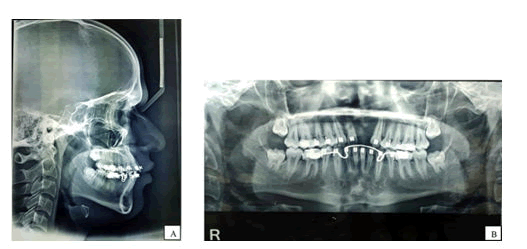
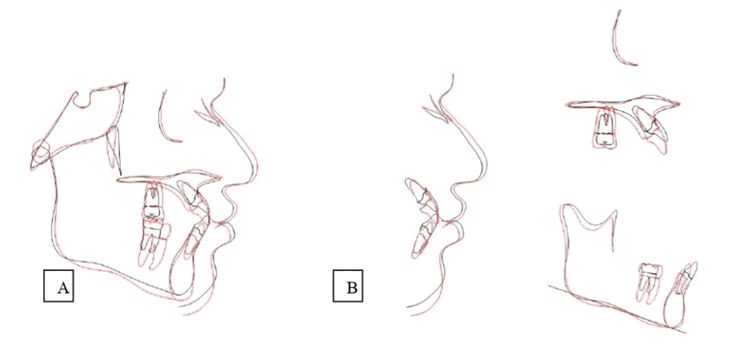
The Orthopantomogram revealed missing 11, 21, 22, mesially inclined 12, 23 and fractured 31. Third molars in all quadrants were in Nollas stage 6 of development. Overall alveolar bone levels were normal. Cephalometric analysis (Figure 2, Table 1) indicated that the patient was in CVMI stage IV (deceleration) and suggested class I skeletal bases with horizontal growth pattern. Upper and lower interiors were proclaimed. The soft tissue analysis demonstrated protrusive upper and lower lips with an acute naso labial angle.
Figure 2: Pre-treatment radiographs, I: Orthopantomogram; II (A-B): Lateral cephalogram.
| Cephalometric parameters | Clinical Norms | Pre-treatment Values | Post treatment values |
|---|---|---|---|
| SNA | 82 ± 2° | 81° | 81° |
| SNB | 80 ± 2° | 80° | 79° |
| ANB | 2 ± 2° | 1° | 2° |
| A-B plane angle | -9 to 0° | 1° | 0° |
| Angle of convexity | -8.5 to 10° | -1° | 1° |
| Wits | 0 to -1 mm | -2 mm | 0 mm |
| Beta angle | 27-35° | 33° | 32° |
| FMPA | 25 ± 2° | 18° | 19° |
| SN-GoGn | 32 ± 2° | 20° | 20° |
| Jarabak ratio | 62-65% | 76.60% | 75.30% |
| Max. I-NA | 22 ± 2° | 40o | 29° |
| Max. I-NA (mm) | 4 mm | 8 mm | 4 mm |
| Man. I-NB | 25 ± 2° | 32o | 22° |
| Man. I-NB (mm) | 4 mm | 9 mm | 4 mm |
| LI-A-Pog | 2.7 ± 1.7 mm | 7 mm | 5 mm |
| IMPA | 90 ± 5° | 107o | 94 o |
| Inter-incisal angle | 135.4o | 108° | 126° |
| Nasolabial angle | 102 ± 8 o | 75° | 95° |
| Ls-E line | -4 mm | -2 mm | -4 mm |
| Li – E plane | -2 mm | 2 mm | -1 mm |
Table 1: Cephalometric summary of pre-treatment and post-treatment values.
Carey's model analysis revealed an arch length discrepancy of 8 mm indicating the need for 1st premolar extraction in the mandibular arch. Bolton’s overall ratio was 95.28% and the anterior ratio was 84.61%. In the maxillary arch, a total of 24 mm was needed to replace the missing 11, 21 and 22, out of which only 14 mm was present, implying insufficient space for replacement of the missing teeth.
Diagnosis
The case was diagnosed as skeletal class I with horizontal growth pattern and convex profile, Angle’s class I Dewey’s modification type 1 and 2 with reduced over jet, missing 11, 21 and 22, cross bite with 23 and acute naso labial angle with protrusive upper and lower lips.
Treatment objectives
- Redistribution of the edentulous space in maxillary arch to facilitate adequate replacement of missing teeth with the prosthesis
- Establishment of normal over jet and overbite supporting functional and esthetic prosthetic rehabilitation and restoration of fractured 31 to normal shape and size
- Correct the convex facial profile
- Proper axial alignment and levelling, correction of maxillary and mandibular pro-clination and cross bite with 23, while maintaining Class I molar relationship
- Achievement of Class I canine relationship on left side
- Correction of midline discrepancy
Treatment plan
In agreement with the orthodontic and prosthodontic goals, it was decided that the case will be treated with fixed orthodontic appliance followed by the prosthetic phase. The case was decided to be treated as a critical (Type A) anchorage case with extraction of mandibular 1st premolars and partial segmental canine retraction followed by incisors intrusion and retraction. In the maxillary arch, space was insufficient to replace all the three missing teeth (11, 21 and 22) and due to accentuated dentoalveolar proclination and soft-tissue convexity, reopening of the space was ruled out [5,6]. It was decided to redistribute edentulous space for prosthetic replacement of only 21 along with 12 substituting for 11, lateralization of canines and 1st premolars substituting for canines by following the rule of golden proportion [7].
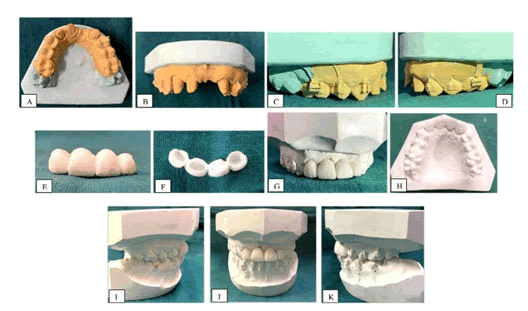
Two prosthetic treatment options were presented to the patient. First one involved replacement of missing 21 by implant-supported prosthesis along with bone graft for the insufficient alveolar bone thickness and thin alveolar crest as determined by CBCT. The second treatment option called for use of Fixed Partial Denture (FPD). The patient didn’t consent to the first plan due to the increased cost and invasiveness of the surgical procedure. Hence, a 4-unit all-ceramic FPD was planned, replacing missing 21 (pontic) with 13, 12 and 23 acting as abutments. A trial diagnostic set-up was prepared in the plaster model to enable both the Orthodontist and the Prosthodontist to visualize the final results confirming that the changes in tooth position were ideal for future restorations that are both esthetically and functionally acceptable [8].
Treatment progress
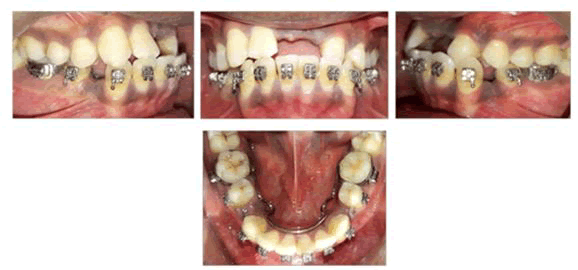
Orthodontic treatment phase: The patient was treated with pre adjusted Edgewise appliance (0.022” x 0.028” MBT prescription). Composite build-up was done with 31 before bracket bonding. Lingual arch was cemented and both mandibular first premolars were extracted. Initially, partial segmental mandibular canine retraction was done on a round 0.018” AJ Wilcock Australian wire (regular plus) to facilitate de-crowding followed by levelling and alignment with continuous 0.016” Nickel-Titanium (NiTi) (Figure 3). Sequentially arch wires were changed up-to 0.019” × 0.025” Stainless Steel (SS). Retraction of lower anterior was initiated using sliding mechanics with active tiebacks to achieve the adequate over jet.
Figure 3: After partial canine retraction in mandibular arch.
- The maxillary arch was bonded 6 months after the mandibular strap-up. Posterior bite was raised till correction of cross bite was achieved. Bracket customization was done by using lateral incisor brackets on canines (future lateral incisors) to give +10o palatal root torque and were positioned slightly gingivally to bring about extrusion leading to improvement of the marginal gingival level. To enable seating of flat bracket base, slight enamel plasty was done. Canine cusp tip and palatal enamel were reduced gradually throughout orthodontic treatment whenever pre maturities were detected [9] after the lower incisors had occupied their final position following retraction. Brackets on 14 and 24 (future canines) were positioned slightly distally to hide the palatal cusp and to give the cervical prominence as that of the canine [11] bracket was bonded on 12 (future central incisor) for +17o palatal root torque.
- To ensure restorative space for the crown on 12 for facilitating substitution into 11, space was created between 12 and 13 by the mesial movement of 12, taking care that the future dental midline matches with the facial midline. This space was retained by giving stops in the wire distal to lateral incisor and mesial to canine.
- To preserve the space for 21 as well as for esthetics, riding pontic was given as an interim replacement at the time of the orthodontic treatment itself. Orthodontic pontic was prepared, tried, adjusted and engaged with the rectangular arch wire [10]. The smile and the confidence of the patient showed considerable improvement after engaging the riding pontic which also facilitated in matching the midlines (Figure 4).
Figure 4: Mid-treatment photographs after anterior maxillary edentulous space redistribution and placement of riding pontic with 21.
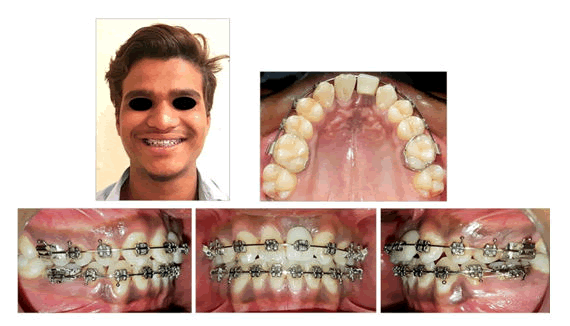
Approximately after 18 months of conventional fixed appliance therapy and achievement of orthodontic goals (Figures 5 and 6), deboning of brackets of 13, 12 and 23 was done and the patient was referred back to the Prosthodontics department. Prosthetic treatment was started immediately to avoid unwanted relapse. The rest of the orthodontic appliance was kept in place along with settling elastics to achieve good posterior interception and to prevent the teeth from drifting during the FPD fabrication.
Figure 5: After complete mandibular alignment and extraction space closure, achievement of sufficient positive over jet and preparation of space in anterior maxilla for pontic with 21.
Figure 6: Radiographs: A) Lateral Cephalogram; B) OPG, after complete mandibular extraction space closure and redistribution of space in anterior maxilla.
Prosthetic treatment phase-periodontal status of the abutments was evaluated. Mock preparation was done on the cast followed by wax-up using white inlay pattern wax (Figure 7).
Figure 7: Mock up; A-D) Crown preparation; E-H) Wax pattern; I-K) Casts in occlusion with wax pattern in place.
After patient’s satisfaction, tooth preparation was initiated with 13, 12 and 23 using a flat-end tapered diamond bur ending up with shoulder margins for the all ceramic prosthesis. For canines, sequential reduction method was followed to avoid pulpal damage. After the application of the gingival retraction cord, impressions were made using the double mix single-stage technique with rubber base impression material. Immediately afterwards, temporization was done using wax-up as the reference with the direct-indirect technique. Following the shade-matching protocol, cementation of FPD was done using glass ionomer cement as a luting agent (Figure 8). The patient was instructed to avoid eating hard food with his anterior teeth for the next 24 hours.
Figure 8: After cementation of 4-unit all-ceramic fixed prosthesis and posterior settling of occlusion.
Results
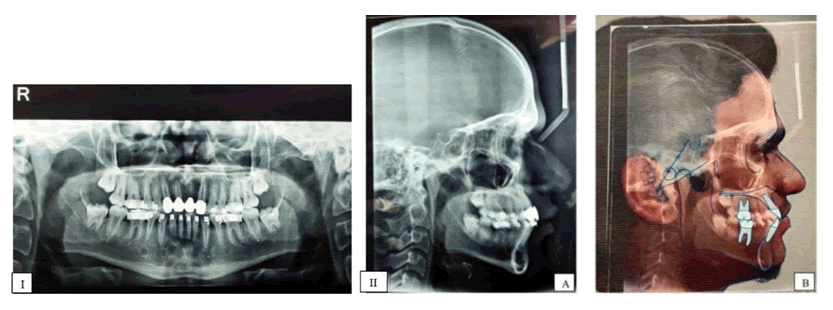
The post-treatment lateral cephalogram (Figure 9 and Table 1) showed significant skeletal, dental and soft tissue changes. Adequate root parallelism was evident on Orthopantomogram with no signs of root resorption. Superimposition of pre-and post-treatment lateral cephalograms demonstrated up righting of mandibular and maxillary incisors, improvement of naso labial angle and lip prominence in relation to the E-line (Figure 10).
Figure 9: Post-treatment radiographs after fixed prosthesis and before posterior debonding; I) Orthopantomogram; II (A-B): Lateral Cephalogram.
Figure 10: Superimposition of pre-and post-treatment Lateral Cephalograms: A-Total, B-Regional.
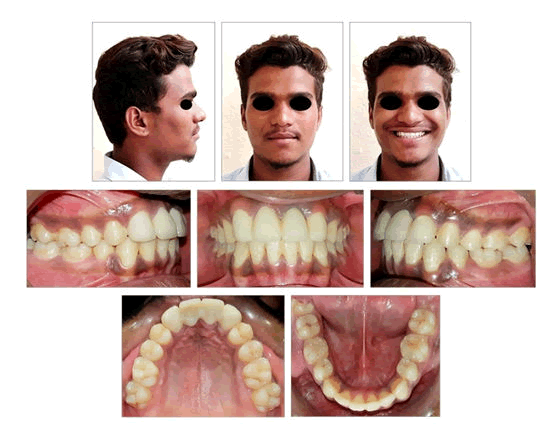
After complete orthodontic and prosthetic correction, the patient exhibited a remarkable improvement of facial profile, esthetics and soft-tissue balance along with a consonant and well-balanced smiles (Figure 11) [11]. Bonded lingual retainer was given in the mandibular arch. Patient was placed on a regular follow-up in which oral hygiene maintenance was found to be satisfactory without any reporting of the periodontal problem.
Figure 11: Post-treatment facial and intraoral photographs.
Discussion
The benefits of pre-prosthetic orthodontics have been well documented [12,13]. The partially edentulous case discussed in this article had three missing maxillary incisors along with reduced over jet and crowded mandibular anterior. The sagittal and vertical clearance and the mesiodistal space weren't favourable for adequate replacement with an esthetically and functionally acceptable prosthesis. Thus, pre-prosthetic orthodontic treatment was deemed necessary for the creation of sufficient over jet and ideal pontic space.
Adjunctive orthodontic procedures to prosthetic rehabilitation of missing anterior teeth are governed by a multitude of factors such as the extent of the edentulous span, teeth alignment, occlusion, over jet, overbite, midlines, skeletal relation and growth pattern [6,14,15]. In this patient, as the space was insufficient to replace all the missing teeth, modification of mechanics by bracket substitutions was devised. Lateralization of canines and premolars replacing canines have been routinely advocated by various authors which can produce excellent long-lasting treatment results by executing optimal torque control, differential extrusion of canines with cusp-tip trimming, mesial rotation and if needed, intrusion of the first premolars [3,16,17]. Use of canines as abutments for FPD in this case further enabled changes in form, contour, and colour by using all ceramic crowns. Here, maxillary lateral incisor brackets were bonded on canines for +10o of palatal root torque. In cases requiring increased palatal root torque, other possible variations can be utilized such as maxillary central incisor bracket or inverted mandibular second premolar bracket delivering +17° root torque [18].
For conversion of 12 into 11, bracket of 11 with +17° palatal root torque was used along with the creation of space distal to lateral incisor by musicalizing it. This space was preserved for achieving the required mesiodistal width of 11 in the prosthesis. Also, it has been observed that the lateral incisor root is capable of supporting the crown of a central incisor size and is considered as a valid treatment modality [19].
The brackets on 1st premolars were positioned slightly distally to bring about mesial rotation which helped to mask the palatal cusp and flat mesial surface, improve the “cuspid” look, and achieve a better contact point [16]. It also ensured that most of its contact with the mandibular cuspid lies on the mesial ridge of the buccal cusp, thereby eliminating the need for grinding the palatal cusps. Generally in cases where 1st premolars are made to replace canines, intrusion is carried out to achieve optimal levelling of the marginal gingiva similar to centrals [3,16]. However, such intruded premolars often require additional restorative build-up to obtain a larger ‘canine’ and also can cause vertical bony defects, leading to an increased risk for alveolar bone loss without systematic periodontal therapy [3,20]. Hence 1st premolar intrusion was avoided in this patient and although some adjunctive gingivoplasty and crown lengthening was needed on ‘now’ canines to improve esthetics, the patient denied it as he was satisfied with the achieved results. Also, the low smile line of the patient successfully helped in masking and making it non-evident [5].
Group function occlusion in lateral excursions was achieved at the end of rehabilitation, which is considered adequate as seen mostly in cases with relocated canines and premolars and do not pose any risk for Temporomandibular disorders [3,21,22].
Prosthetic treatment options in restoring anteriors are removable partial dentures, resin retained, fixed tooth-supported or implant-supported prosthesis and autotransplantation, depending upon the availability of primary abutments, underlying osseous topography, age, post-treatment maintenance and most importantly patient’s preference [9,14,23,24]. In this case, implant-supported prosthesis was ruled out because of the increased cost factor and additional surgical intervention which were unacceptable to the patient. Also considering the young age of the patient, some waiting period was anticipated till the growth completion [25]. Thus all-ceramic fixed prosthesis was finalized in this case which also provided the additional benefit of preventing post-orthodontic relapse along with superior esthetics and durability [15].
Conclusion
Excellence in cases requiring an interdisciplinary approach can only be achieved when attention to detail based upon sound diagnosis is exercised by the teamwork wherein, orthodontics and prosthetic procedures are planned in agreement with the periodontium. The present clinical report underlines the importance of following an integrated approach of prudent case selection and adherence to sound orthodontic principles, which can lead to the permanence and biological compatibility of the finished result and overcome the challenges in achieving satisfactory treatment results from the professional and the patient perspective.
Acknowledgement
We would like to thank the patient for his consent to publish his treatment records.
References
- Steele JG, Sanders AE, Slade GD, et al. How do age and tooth loss affect oral health impacts and quality of life? A study comparing two national samples. Community dent oral epidemiol 2004; 32:107-114.
- Biagi R, Cardarelli F, Storti E, et al. Multiple traumatic injury to maxillary incisors in an adolescent female: treatment outcome with two years follow-up. Ann Stomatol (Roma) 2013; 4:212-217.
- Rosa M, Lucchi P, Ferrari S, et al. Congenitally missing maxillary lateral incisors: long-term periodontal and functional evaluation after orthodontic space closure with first premolar intrusion and canine extrusion. Am J Orthod Dent fac Orthop 2016; 149:339-348.
- Sarver DM. Orthodontics and Esthetic Dentistry: Mission Possible! A Broader Approach to Interdisciplinary Esthetic Treatment. J Cosmet Dent 2016; 31:14-26.
- McNeill RW, Joondeph DR. Congenitally absent maxillary lateral incisors: treatment planning considerations. Angle Orthod 1973; 43:24-29.
- Paduano S, Cioffi I, Rongo R, et al. Orthodontic management of congenitally missing maxillary lateral incisors: A case report. Case rep dent 2014; 1-7.
- Levin EI. Dental esthetics and the golden proportion. J Prosthet Dent. 1978; 40:244-252.
- Alfallaj H. Pre-prosthetic orthodontics. Saudi dent j 2020; 32:7-14.
- Sabri R. Management of missing maxillary lateral incisors. J Am Dent Assoc 1999; 130:80-84.
- Mathew BN, Senthil Kumar KP, Tamizharasi S. "Riding pontics": A tool behind a confident smile: A case report. J Indian Acad Dent Spec Res 2015; 2:90-93.
- Sabri R. The eight components of a balanced smile. J Clin Orthod 2005; 39:155-167.
- Kokich VG, Spear FM. Guidelines for managing the orthodontic-restorative patient. Semin Orthod 1997; 3:3-20.
- Chaushu S, Becker A, Zalkind M. Prosthetic considerations in the restoration of orthodontically treated maxillary lateral incisors to replace missing central incisors: a clinical report. J Prosthet Dent 2001; 85:335-341.
- Devadoss P, Kumar VR, Dua P, et al. Adjunct orthodontics in contemporary prosthodontic rehabilitation of hypodontia: An interdisciplinary case report. IP Ann Prosthodont Restor Dent 2020; 6:34-37.
- Meyur S, Barui AK, Das R, et al. Comprehensive orthodontic and prosthodontic rehabilitation of hypodontia: a case report of interdisciplinary approach. Int J Contemp Med Res 2019; 6:1-4.
- Rosa MA, Zachrisson BU. Integrating esthetic dentistry and space closure in patients with missing maxillary lateral incisors. J Clin Orthod 2001; 35:221-234.
- Rosa M, Zachrisson BU. Integrating esthetic dentistry and space closure in patients with missing maxillary lateral incisors: Further improvements. J Clin Orthod 2007; 41:563-573.
- Gupta SP, Rauniyar S. Orthodontic space closure of a missing maxillary lateral incisor followed by canine lateralization. Case Rep Dent 2020; 14:1-7.
- Czochrowska EM, Skaare AB, Stenvik A, et al. Outcome of orthodontic space closure with a missing maxillary central incisor. Am J Orthod Dent fac Orthoped 2003; 123:597-603.
- Papapanou PN, Wennstrom JL. The angular bony defect as indicator of further alveolar bone loss. J Clin Periodontol 1991; 18:317-322.
- Robertsson S, Mohlin B. The congenitally missing upper lateral incisor. A retrospective study of orthodontic space closure versus restorative treatment. Eur J Orthod 2000; 22:697-710.
- Nordquist GG, McNeill RW. Orthodontic vs. restorative treatment of the congenitally absent lateral incisor: Longterm periodontal and occlusal evaluation. J Periodontol 1975; 46:139-143.
- Mcintyre, Frederick. Restoring esthetics and anterior guidance in worn anterior teeth: A conservative multidisciplinary approach. J Am Dent Assoc 2000; 131:1279-1283.
- Lahoti E, Nakib A, Choudhury P, et al. Esthetic Rehabilitation of Bilaterally Missing Maxillary Permanent Canines–An interdisciplinary Approach. Global J ResAnalysis 2016; 5:164-167.
[Crossref]
- Oesterle LJ, Cronin RJ Jr. Adult growth, aging, and the single-tooth implant. Int J Oral Maxillofac Implants 2000; 15.
Author Info
Akanksha Kumar1*, Apurv Mamidwar2, Narendra Sharma3, Ranjit Kamble3, Sunita Shrivastav3 and Shriya Murarka3
1Department of Orthodontics and Dentofacial Orthopaedics, Swargiya Dadasaheb Kalmegh Smruti Dental College and Hospital, Nagpur, Maharashtra, India2Department of Prosthodontics, Sharad Pawar Dental Collegeand Hospital, Datta Meghe Institute of Medical Sciences (Deemed to be University), Sawangi, Wardha, Maharashtra, India
3Department of Orthodontics and Dentofacial Orthopedics, Sharad Pawar Dental College and Hospital, Datta Meghe Institute of Medical Sciences (Deemed to be University), Sawangi, Wardha, Maharashtra, India
Citation: Akanksha Kumar, Apurv Mamidwar, Narendra Sharma, Ranjit Kamble, Sunita Shrivastav, Shriya Murarka, Orthodontic Therapy as an Adjunct to Prosthetic Rehabilitation for Restoring Esthetics and Function: An Interdisciplinary Case Report, J Res Med Dent Sci, 2022, 10 (7): 000-000.
Received: 02-May-2022, Manuscript No. JRMDS-22-46825; , Pre QC No. JRMDS-22-46825; Editor assigned: 04-May-2022, Pre QC No. JRMDS-22-46825; Reviewed: 18-May-2022, QC No. JRMDS-22-46825; Revised: 04-Jul-2022, Manuscript No. JRMDS-22-46825; Published: 14-Jul-2022