Research - (2021) Volume 9, Issue 7
Osteoconductive Efficacy of Marine Shells Nanoparticles Hydroxyapatite in Bone Regeneration-An Experimental Study in Rabbits
Wafaa K Abid1* and Alyaa I. Naser2
*Correspondence: Wafaa K Abid, Department of Dentistry, Iraq, Email:
Abstract
Introduction: For manipulating new products which used in the treatment of bones diseases, it is essential to understand bone repair and regeneration. Objectives: The purpose was to evaluate the osteogenic response of new synthetic nanohydroxyapatite originated from marine shells in regeneration mandibular bone defects of rabbits. Materials and Methods: 42, domestic male rabbits were divided randomly into 3 classes based on sacrificing days (1week, 2weeks, 4 weeks), every class has fourteen rabbits. Each rabbit was given research material's (Nanoparticles Hydroxyapatite (HAP)). On either sides of the inferior border of the mandible, a three cm parallel incision was rendered after anesthetize the rabbits. To consider as a control group, the first hole on the right side of the mandible was left empty, while the second hole on the left part of the mandible was introduced with 0.25 mg for formulating a nanoparticle's hydroxyapatite. Bone samples were harvested for histological analysis. The data was submitted for statistical analysis with a level of significance of 0.05. Results: The bone regeneration process was a trend toward increased new bone formation in the nanoparticle hydroxyapatites treated group in second and fourth-week intervals (P value were 0.034, 0.011 respectively). Interestingly, no residual of large particles of the nano-HAP material were noticed in the augmented group. Conclusions: It demonstrated that under these experimental conditions, new nano-hydroxyapatite crystals showed osteoconductive potential and are an excellent treatment alternative to autologous bone graft in the field of bone regeneration.
Keywords
Biomaterials, Bone graft, Nano-hydroxyapatite, Regeneration of bone, Tissue engineeringIntroduction
The major challenge facing the world is to improve bone repair and regeneration by introducing an alternative manipulative novel material for the treatment of bone diseases [1, 2]. In order to enhance tissue growth when grafting bone defects with biomaterials, the ingredients that used must have mechanical integrity identical to natural bone. Recently the use of nanotechnology has received increased attention to expanding current styles in tissue and bone regeneration. Indeed, the precise structures of nanoparticles should have solid colloidal particles usually between 10 and 200 nm in dimension with inordinate adaptability in terms of size, surface chemistry, and components. Biomaterial has a distinct structure that allow for structural support, tissues repair, and regenerations. Marine structure is a bioactive material with mechanical and medical characteristics that have many applications in tissues engineering and drugs distribution. In addition, the natural factors in the chemistry of marine's shells show osteoinductive features, resulting in a stronger osteogenic responding in human's tissue [3-5]. Using the marine skeleton is not limiting for tissue restoration in maxillofacial [6] dental [7] Orthopedic, but they can also be used as a carrier system for medicine, gene, or growth factor in small quantities due to the Nano- and mesoporous structures in their constructions [8,9]. Since existing bones healing management options are inadequate, novel strategies have been proposed to generate HAp powders from biogenic constructions that are similar to bones in behavior and structure. By used various synthesis processes which have covered widely in the last 2 decades with metals including eggshell, seashell, animal's bone, and corals. Aside from HAP's biogenic capital, the price increase of bio-ceramics on the market helps natural biogenic material to acquire economic and environmental benefits. It has even been suggested though that these natural nanoparticle HAP products manufactured from marine's shells are physiochemically related to human's bones, they're less likely to be rejected by body tissue [10].
Considering the data explained above, the null hypothesis of this study was that there would be a positive influence of newly synthesized nanoparticle hydroxyapatite from natural marine skeleton biomaterials on enhancing bone regeneration in rabbit’s bone defects.
Materials and Methods
Preparation and characterization of Hydroxyapatite from seashells
Synthesis
Washing the shells from macroscopic impurities in purified water is the first step in synthesize calcium oxide from marine shells, then boiling for ten minutes to killed the microbes, and drying in the air for 48 hours. Using a mortar and pestle, these shells were ground into powder [11]. The powder was then heated for an hour to 900°C in a furnace (Manfredi/Italy) and the shell became pore, fragile and very white at that temperature. This shows that the CaCO3 seashell disintegrates (decarbonisation) and gives CaO and CO2, based on the reaction [12].
CaCO3 → CaO+CO2
(64 grams of CaO was given from100grams of marine shell) (Figure 1).
Figure 1: Sea shell after firing.
Hydroxyapatite prepared from seashell
Constantly stirring (30ml) phosphoric acid into (50gm) calcium oxide powder yielded hydroxyapatite (HAP) (set from seashell). Vapor and heat accompanied the chemical reaction. The pH of the process and the density of the reactant must be tightly controlled for obtaining principal hydroxyapatite. The commodity was dried for two hours at 150ºC [11] (Figures 2 and 3).
Figure 2: CaO with phosphoric acid.
Figure 3: HA after drying.
Characterization
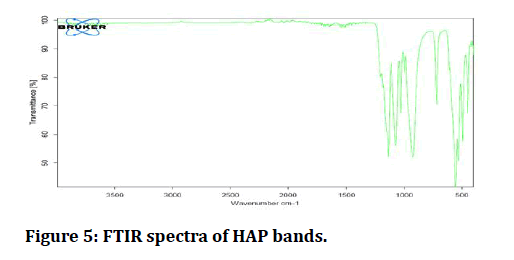
The functional groups present in newly synthesized hydroxyapatite products were ascertained by Infrared Spectroscopy (FTIR) Alfa Bruker instrument, Germany.
Preparation of nanoparticles of hydroxyapatite from seashell
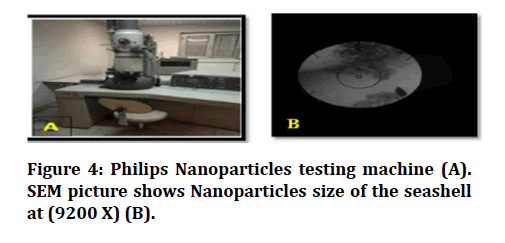
In order to produce pure Nano-Hydrosyapatite of chemical formula; Ca10 (PO4)6(OH)2, nanoparticles were prepared by mechanical attrition [13]. About 100 grams of prepared HAP from the marine shell was conducted. After that, the powder was broken into small pieces then was ground. The structural characterization of nHAp powder synthesized samples was measured using Scanning Electron Microscope (SEM) in Al-Nahrain University laboratory by Philips machine (Model CM10, Holland) as shown in (Figure 4A and 4B). The size of the Nanoparticle was 20-35 nm. The name was provided in the form of powder to be inserted in the bone defect.
Figure 4: Philips Nanoparticles testing machine (A). SEM picture shows Nanoparticles size of the seashell at (9200 X) (B).
Experimental groups and surgical procedure
Forty-two, domestic male rabbits were used in this study. Their age group ranged between6-8 months, each weighing about 2.3±0.5 kg. They all seemed to have good health through continuous monitoring by a veterinarian throughout the study. Once the fur is removed and the operating surface has been washed, the individual animal received a dose of 4mg/kg (Gracure, Pharmaceuticals Ltd, Bhiwadi, India) and 5mg/kg (Interchemi Co, Holland) of ketamine injected into the muscle of the thigh, at an intramuscular dose. Anesthetic integrity of the ear-pinch reflex loss was checked after 10-15 minutes [14]. The animals were divided randomly into three groups according to sacrificing days’ post-intervention, corresponding to follow-up periods (1week, 2 weeks, 4 weeks), with fourteen rabbits per group. Every rabbit in all groups was treated with study material (Nanoparticles Hydroxyapatite). The animals were classified into three classes based on post-intervention sacrificing days, which matches up to follow-up times, with seven rabbits in each group (one week, two weeks, and four weeks). Study material was given to every rabbit in every group (Nanoparticles Hydroxyapatite). Once the rabbit became anesthetized, a 3 cm parallel incision was committed by both sides of the inferior border of the mandible with a no. 15 blade on a scalpel handle. The periosteum was retracted to expose the inferior border of the mandible between the anterior and posterior teeth to avoid damage to the teeth's roots (interdental space). Using a round surgical bur with an external cooler and a 0.2 percent chlorhexidine solution as a cooling irrigant, two 5mm diameter circular subcritical size deficiencies were formed in the buccal-lingual area on either side of the rabbit's mandible (Al-Rahma pharmaceutical CO. JORDAN). First defect served as a control on the right side of the mandible, the second defect is formed on the left side of the mandible and implanted with (0.25 gm) of freshly made modern nanoparticles hydroxyapatite. Finally, the mucoperiosteal flaps were carefully sutured over the defect areas of all the rabbits using 3/0 absorbable suture (VICRYL® coated polyglactin 910, Ethicon) to restore them to their original position.
The animals grouping was divided as follow (Table 1).
Table 1: Distribution of animals in groups, based upon whether defects implanted with nanoparticles hydroxyapatite as a bone graft or none (empty defects).
| Groups | No. of animals | nHAP (left side) | Control (right side) |
|---|---|---|---|
| Group 1 (1 week) | 14 | Unilateral filled | None (empty defects) |
| Group 2 (2 weeks) | 14 | Unilateral filled | None (empty defects) |
| Group 3 (4 weeks) | 14 | Unilateral filled | None (empty defects) |
Group 1: 1 week, had defects filled with nanoparticles hydroxyapatite and had defects without bone graft (control).
Group 2: 2 weeks, had defects filled with nanoparticles hydroxyapatite and had defects without bone graft.
Group 3: 4 weeks, had defects filled with nanoparticles hydroxyapatite and had defects without bone graft.
Follow-up and assessment
The animals were given a single dose of oxytetracycline (5 mg/kg) intramuscularly shortly after surgery (Chongqing Fangtong Animal Pharmaceutical, China) [15]. Before they were completely healed from anesthesia, the operated animals were held apart in cages. During the first twenty-four hours following surgery, the operated animals were closely monitored, particularly in terms of feeding and physical activity. Within 3-4 hours of surgery, all animals were back to normal activities and feeding. The animals were euthenized after prescribed healing time had passed, and the mandibles were dissected and fixed in 10% formalin. Every group's mandible was divided into two parts, one of which contained hydroxyapatite nanoparticles and the other of which was left empty. The bone was then decalcified in a solution containing 10% formic acid and 10%hydrochloric acid. The specimens were decalcified, then dehydrated with a graded sequence of ethanol and xylene (70-99 %ethanol and xylene), coated in paraffin wax, partitioned with a microtome (4m thickness), and staining with hematoxylin and eosin.
Histological criteria
In order to evaluate the speed of healing, we have employed Lucaciu et al [16] criteria, with certain modification [17, 18] as described in (Table 2). Histopathological analyses were performed using an Olympus light microscope (X10, X40) and read independently by two expert histopathological evaluators. The score line was computed as the average of the two measurements.
Table 2: Histological scoring criteria.
| Criteria | Description | Points |
|---|---|---|
| Amount of inflammatory cells | Plenty | 1 |
| Moderate | 2 | |
| Few | 3 | |
| Absent | 4 | |
| Neo-blood vessels formation | Absent | 0 |
| Present at peripherally | 1 | |
| Present at centrally | 2 | |
| Present centrally and at the periphery | 3 | |
| Amount of granulation tissue | Profound | 1 |
| Moderate | 2 | |
| Scant | 3 | |
| Absent | 4 | |
| New bone formation | Absent | 0 |
| Present at the periphery | 1 | |
| Present centrally | 2 | |
| Present centrally and at the periphery | 3 | |
| Presence of osteoblast cells | Absent | 0 |
| Present at the periphery | 1 | |
| Present centrally | 2 | |
| Present at the periphery and centrally | 3 | |
| Presence of osteoclast cells | Absent | 0 |
| Present at the periphery | 1 | |
| Present centrally | 2 | |
| Present at the periphery and centrally | 3 |
Evaluation of the measurements
The software package SPSS 19.0 was used to statistically analyze all data. Between the classes, statistical differences were noticed. The Paired Wilcoxon Signed- Rank Test was used to compare mean values. P ≤ 0.05 was thought to be statistically relevant.
Results
Infrared spectroscopy estimation of hydroxyapatite bands
The results showed that the prepared nHAP is a biocompatible α-orthophosphate type. On drying with 100 ± oC, the powder structure was analyzed with FT-IR spectroscopy. Fourier Infrared Transform Spectroscopy (FTIR) is an analytical technology widely used to routinely characterize biomaterials. In the spectrum of synthetic commercial hydroxyapatite, hydroxyl stretch of 3569 cm-1 is observed.
The IR spectrum of raw HAP powder
O-H group stretch vibration may clarify the strong peak ranging from 3300-3600 cm-1. CO32- stretching is allocated to the band at 1450 cm-1. At 1048 cm-1, a strong PO4-3 peak appeared. A sharp peak of OH stretch vibration band appeared at 3570 cm-1, and a less intense CO3- peak appeared at 1450 cm-1. Additional phosphate group bands can be found in the 963, 875, 633, and 472 cm-1 regions.
At 1048 cm-1, a strong PO4-3 peak appeared. Phosphate peaks can be found in the 1110, 975, 600, and 470 cm-1 regions.
At 1254, 1200 cm-1, there is a C-O-C peak, and at 1040 cm-1, there is an extreme phosphate peak. At 810 cm-1 and 757 cm-1, there are additional phosphate group bands. There is no peak at 2270 cm-1 in this spectrum. The structure of hydroxyapatite is confirmed by these bands (Figure 5).
Figure 5: FTIR spectra of HAP bands.
Histological assessment of mandible defect repair
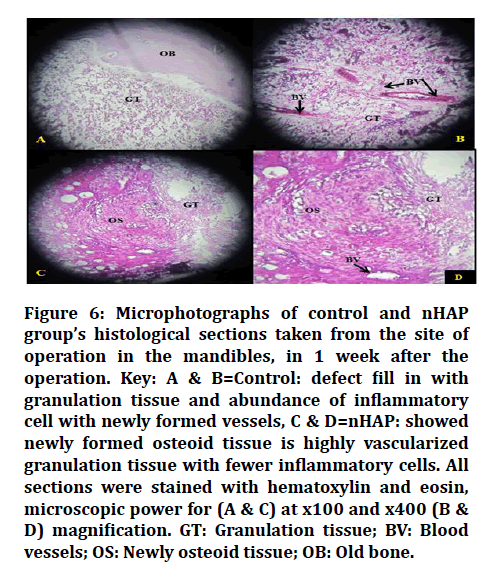
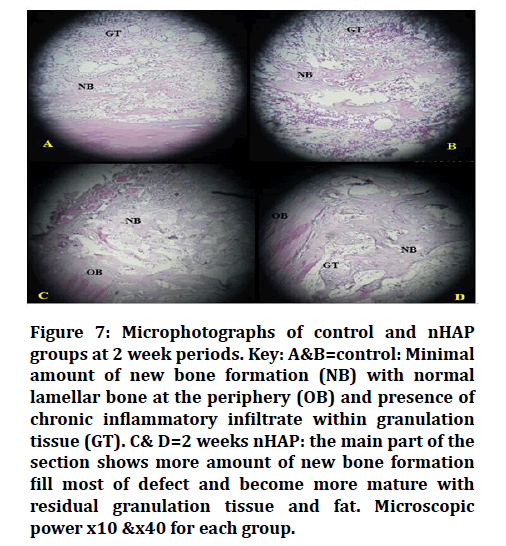
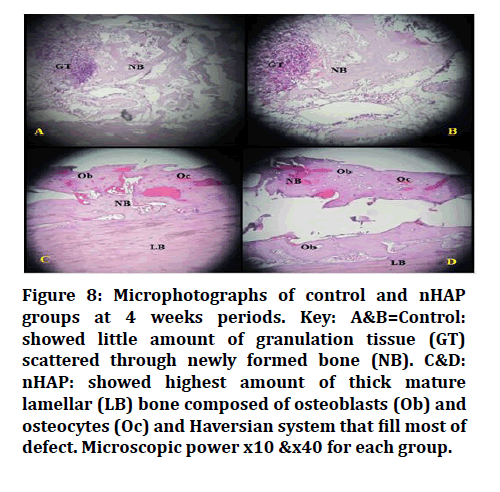
The results of the statistical analysis of the differences between seashell (nanoparticle) hydroxyapatite and control regarding granulation tissue formation, inflammation, blood vessel formation, new bone formation, osteoblast, and osteoclast formation, at given periods of healing are showed in (Table 3). Regarding material using in this study, there were very low levels of inflammatory cells seen microscopically and no evidence of foreign body response which revealed biocompatibility of biomaterial. Furthermore, there were no residues of bone substitute material (nHAP) detected in the augmented defects (Figure 6). For all stages of healing, the Paired Wilcoxon signed-rank test showed discrepancies between variables. A p-value≤ 0.05 was used to determine statistical significance. The overall histological scores concerning the one-week duration of healing period sof bone granulation tissue formation, inflammatory reaction, and new blood vessels formation appeared more significant than others in which P-values for them were (0.014, 0.025, and 0.059) respectively while in two weeks’ period all histopathological score appeared significant except in inflammatory reaction in which P-value was (0.180). The best results of new bone apposition were observed around the experimental defects (Figure 7). However, in the fourth week of rehabilitation, treating subjects bridged more bones than control subjects, with a big variation at P≤ 0.05 (Figure 8).
Table 3: Paired Wilcoxon signed-rank test for histopathological readings between variables within same periods of bone healing.
| Criteria | Description | Points |
|---|---|---|
| Amount of inflammatory cells | Plenty | 1 |
| Moderate | 2 | |
| Few | 3 | |
| Absent | 4 | |
| Neo-blood vessels formation | Absent | 0 |
| Present at peripherally | 1 | |
| Present at centrally | 2 | |
| Present centrally and at the periphery | 3 | |
| Amount of granulation tissue | Profound | 1 |
| Moderate | 2 | |
| Scant | 3 | |
| Absent | 4 | |
| New bone formation | Absent | 0 |
| Present at the periphery | 1 | |
| Present centrally | 2 | |
| Present centrally and at the periphery | 3 | |
| Presence of osteoblast cells | Absent | 0 |
| Present at the periphery | 1 | |
| Present centrally | 2 | |
| Present at the periphery and centrally | 3 | |
| Presence of osteoclast cells | Absent | 0 |
| Present at the periphery | 1 | |
| Present centrally | 2 | |
| Present at the periphery and centrally | 3 |
*Significance at P ≤ 0.05, nHAP= nanoparticles hydroxyapatite, con= control (without the addition of bone graft).
Figure 6: Microphotographs of control and nHAP group’s histological sections taken from the site of operation in the mandibles, in 1 week after the operation. Key: A & B=Control: defect fill in with granulation tissue and abundance of inflammatory cell with newly formed vessels, C & D=nHAP: showed newly formed osteoid tissue is highly vascularized granulation tissue with fewer inflammatory cells. All sections were stained with hematoxylin and eosin, microscopic power for (A & C) at x100 and x400 (B & D) magnification. GT: Granulation tissue; BV: Blood vessels; OS: Newly osteoid tissue; OB: Old bone.
Figure 7: Microphotographs of control and nHAP groups at 2 week periods. Key: A&B=control: Minimal amount of new bone formation (NB) with normal lamellar bone at the periphery (OB) and presence of chronic inflammatory infiltrate within granulation tissue (GT). C& D=2 weeks nHAP: the main part of the section shows more amount of new bone formation fill most of defect and become more mature with residual granulation tissue and fat. Microscopic power x10 &x40 for each group.
Figure 8: Microphotographs of control and nHAP groups at 4 weeks periods. Key: A&B=Control: showed little amount of granulation tissue (GT) scattered through newly formed bone (NB). C&D: nHAP: showed highest amount of thick mature lamellar (LB) bone composed of osteoblasts (Ob) and osteocytes (Oc) and Haversian system that fill most of defect. Microscopic power x10 &x40 for each group.
Discussion
The outcomes of this study were to confirm the set of rabbit models to investigate the healing of a mandibular critical-size defect submits with nanoparticles hydroxyapatite. As the rabbits get a higher metabolism and bone turnover than humans, and healing is nearly finished at four weeks, the four-week time frame was specified. The major challenge that faced the surgeon in the reconstruction of critical-size bony defects is the lack of suitable grafting material and techniques to restore the volume and shape of alveolar defects. A critical size defect, as defined by Schmitz et al. [19], is one that is sufficient to produce a non-viable blankness, preventing indirect bone healing from bridging the gap. The bone defect in this experiment was 5mm to enable the bone for healing via restitutio and integrum, also for defining a meaning of supercritical scale defect rely on research that proposed the defect must not be bigger to 8.8mm in diameter [20]. Marine’s shells, which have been majorly carbonated, are biogenic materials that's used through a two decades in the treatments of multiple defects. Those who were tailored the naturally dense configurations to bones and supplied them both structural strength and other biochemical processes feasible for reparation and regeneration of human tissue [21].The null hypothesis was accepted, as there was more bone regeneration and improvement in bony structural defect augmented with nHAP rather than control one. The results of this study coincided with the results of Macha et al. where structural performance was maintained and bone repair improved. It is due to nanoand microstructures, which constitute an important element in the conversion of marine shells and show a promise that bone reparation and regenerative medicine can be maintained structural capacity [2]. Several efforts were made to generate nHAp from seashells in order for improving tissue and organ regenerations. Nanoparticles have a lot of promise in the fields of bone regenerations. The use of nanoparticles offers interesting features to advance the field of bone tissue engineering. Our results indicated the benefit of our ground-breaking new method for synthesizing and processing nHAp powders from marine shells as a biogenic source for bone regeneration. The findings were equivalent in a study conducted in Jahangirnezhads where nHAP consisted mainly of osteoconductive properties which can produce adequate bone quantities as substitutes products for the bone [22]. Histologically, the treatment of nHAp for bone defects has increased the total number of newly formed blood vessels and reduced infiltration of inflammatory cells. The in vivo observation that nHAP was more powerful to initiate fibroblast and collagen fibre, increased osteoblast proliferation was supported by histologic analysis which showed more concentrated forming and newly formed bone formation in study group wounds. Those finding that support bone regeneration process in vivo may be explained by osteoconductive properties of nHAP by it is role through chemo-attraction of cells first at the wound site that accumulate and debride the injured tissue. In biological bone healing strategies (hemostasis, inflammation, proliferation and remodeling), the attracting mesenchymal cells play crucial roles, which start with well-vascularized connective tissue that fills the wound bone, which is presented as a granulation tissue, increases chemotactic activity that results in a higher inflammatory response and activation by angiogenesis. Subsequently, these blood vessels will form an intergranular web that could transfer precursor osteoblast cells into the grain [23] and lead to a newly immature bone, which has been subsequently transformed into mature bone. Pilloni et al. have shown that nHAP can increase osteoblast proliferation and differentiation [24]. This finding showed great similarity to our results that demonstrated statistical significance of osteoblasts proliferation in experimental group at second and fourth weeks.
Following studies done by Kubasiewicz et al, on calvaria defect treated with application of nano-HAP, the authors achieved very promising properties of using nHAP on bone regeneration when used alone or combined with other biomaterials [25]. The results have been combined with previous studies that have shown statistically significantly higher levels of bone formation in the study group compared to the control group. Some behavior was attributed to the clarification of techniques via which nHAP promotes bone constriction. Chemotaxis, proliferation, and successive differentiation of mesenchymal cells were used by HA to speed up bone formation. HA promotes cell mineralization by increasing alkaline phosphatase levels. By providing a scaffold to which osteoprogenitor cells could bind and promote osteoblastic differentiation, HA allowed for the early deposition of osteoid tissue. This may be true for HA's osteoconductive and osteoinductive properties, which promote early osteogenesis and subsequent bone remodeling [26]. Additionally, the pore sizes of nanoparticles and interconnectivities of the pores may offer new opportunities to promote angiogenesis, migration of cells, and repair of bone defects even without the use of growth factors [27]. Furthermore, the main advantage in nanophase is to gain smaller material grain size which greatly plays an important factor in increasing the surface area in relation to it is volume which have great potential for bone tissue regeneration [28]. In other hands, when exogenous HA is applied to the surgical site, its anti-inflammatory properties can reduce postoperative inflammation and bacterial contamination, improving surgical outcomes [29]. Via achieving clinical findings analogously to most studies, nHAP's primary benefits being biocompatibility, slow insitu biodegradability and good osteoconductive properties [30] have resulted in its being a suitable biogenic material for the treatment of bone defects possess a good stimulant cell responsiveness to promote faster bone regeneration.
Conclusion
This study assesses the new preparation of nHAP in the treatment of bone defect from a marine skeleton. Histologically, a positive osteogenic potential was shown to show nHAP to be an appropriate alternative to autogenous bone graft in bone tissue regeneration. The use of this kind of biological materials has recently been improved, presumably due to its biocompatibility, osteoconductivity, lack of toxicity, etc. More clinical studies are required on different biomaterial applications combined with other bioactive materials or growth factors that may induce a synergistic effect in terms of new bone formation.
Ethical Approval
All animal’s procedure involving in this study was conducted in compliance with guidelines of National Institutional Health Principles of Laboratory Animal Care (NIH publication no. 85-23, revised 1985). The authors declared that they have obtained Institutional ethical approval for this study (protocol number UOM.Dent/A.L. 15/21).
Conflict of Interest
The authors declare no competing of interest.
Funding
None.
References
- Zhu P, Huang G, Zhang B, et al. Assessment of fracture healing properties of lovastatin loaded nanoparticles: Preclinical study in rat model. Acta Biochimica Polonica 2019; 66:71-76.
- Macha IJ, Ben-Nissan B. Marine skeletons: towards hard tissue repair and regeneration. Mar Drugs 2018; 16:225.
- Macha IJ, Cazalbou S, Ben-Nissan B, et al. Marine structure derived calcium phosphate-polymer biocomposites for local antibiotic delivery. Mar Drugs 2015; 13:666-680.
- Alakpa EV, Burgess KE, Chung P, et al. Nacre topography produces higher crystallinity in bone than chemically induced osteogenesis. ACS Nano 2017; 11:6717-6727.
- Rink JS PM, Tripathy S, Thaxton CS. Update on current and potential nanoparticle cancer therapies. Curr Opin Oncol 2013; 25:646-651.
- Chen PY, Lin AY, McKittrick J, et al. Structure and mechanical properties of crab exoskeletons. Acta biomaterialia 2008; 4:587-596.
- Lahaye M, Robic A. Structure and functional properties of ulvan, a polysaccharide from green seaweeds. Biomacromol 2007; 8:1765-1774.
- Karacan I, Macha IJ, Choi G, et al. Antibiotic containing poly lactic acid/hydroxyapatite biocomposite coatings for dental implant applications. Key Eng Mater 2017; 758:120-125.
- Macha IJ, Cazalbou S, Shimmon R, et al. Development and dissolution studies of bisphosphonate (clodronate)-containing hydroxyapatite–polylactic acid biocomposites for slow drug delivery. J Tissue Eng Regen Med 2017; 11:1723-1731.
- Webster TJ, Ahn ES. Nanostructured biomaterials for tissue engineering bone. Tissue Eng II 2006; 275-308.
- Alkhalidi EF, Alsalman TH, Taqa AA. Mechanical properties of new calcium based cement prepared from egg Shell. Int J of Enhanced Res Sci Technol Eng 2014; 3:70-76.
- Alkhalidi EF, Alsalman TH, Taqa AA. Antibacterial properties of new calcium based cement prepared from egg shell. Edorium J Dent 2015; 21-28.
- DeCastro CL, Mitchell BS. Nanoparticles from mechanical attrition. Synthesis, functionalization, and surface treatment of nanoparticles. 2002; 5.
- Henke J, Astner S, Brill T, et al. Comparative study of three intramuscular anaesthetic combinations (medetomidine/ketamine, medetomidine/fentanyl/midazolam and xylazine/ketamine) in rabbits. Vet Anaesth Analg 2005; 32:261-270.
- Zheng LW WM, Rabie ABM, Cheung LK. Evaluation of recombinant human bone morphogenetic protein-2 in mandibular distraction osteogenesis in rabbits: Effect of dosage and number of doses on formation of bone. Br J Oral Maxillofac Surg 2006; 44:487-494.
- Lucaciu O GD, Soritau O, Baciut M, et al. Comparative assessment of bone regeneration by histometry and a histological scoring system. Rev Romana Med Lab 2015; 23:31-45.
- Naser AI. The effect of the new hemostatic agent Ostene® on bone healing: An experimental study in rabbits. J oral Res 2018; 7:286-291.
- Abid WK, Mukhtar YH. Repair of surgical bone defects grafted with hydroxylapatite+ β-TCP combined with hyaluronic acid and collagen membrane in rabbits: A histological study. J Taibah Univ Med Sci 2019; 14:14-24.
- Schmitz JP, Hollinger JO. The critical size defect as an experimental model for craniomandibulofacial nonunions. Clin Orthop Relat Res 1986; 205:299-308.
- Honma T, Itagaki, T, Nakamura M, et al. Bone formation in rat calvaria ceases within a limited period regardless of completion of defect repair. Oral Dis 2008; 14:457-464.
- Macha IJ, Cazalbou S, Ben-Nissan B, et al. Marine structure derived calcium phosphate–polymer biocomposites for local antibiotic delivery. Mar Drugs 2015; 13:666-680.
- Jahangirnezhad M, Kazeminezhad I, Saki G, et al. The effects of Nanohydroxyapatite on bone regeneration in rat calvarial defects. Am J Res Commun 2013; 1:302-316.
- Gotz W, Gerber T, Michel, B, et al. Immunohistochemical characterization of nanocrystalline hydroxyapatite silica gel (NanoBone(r)) osteogenesis: A study on biopsies from human jaws. Clin Oral Implants Res 2008; 19:1016-1026.
- Pilloni A, Pompa G, Saccucci M, et al. Analysis of human alveolar osteoblast behavior on a nano-hydroxyapatite substrate: An in vitro study. BMC oral health 2014; 14:1-7.
- Kubasiewicz-Ross P, Hadzik J, Seeliger J, et al. New nano-hydroxyapatite in bone defect regeneration: A histological study in rats. ANN Anat 2017; 213:83-90.
- Gotz W, Lenz S, Reichert C. A preliminary study in osteoinduction by a nano-crystalline hydroxyapatite in the mini pig. Folia Histochem Cytobiol 2010; 48:589-596.
- Furuya H, Tabata Y, Kaneko K. Bone regeneration for murine femur fracture by gelatin hydrogels incorporating basic fibroblast growth factor with different release profiles. Tissue Eng Pt A 2014; 20:1531-1541.
- Lim KT, Patel DK, Dutta SD, et al. Human teeth-derived bioceramics for improved bone regeneration. Nanomater 2020; 10:2396.
- Gontiya G GS. Effect of hyaluronan on periodontitis: A clinical and histological study. J Indian Soc Periodontol 2012; 16:184-192.
- Huber FX, McArthur N, Hillmeier J, et al. Void filling of tibia compression fracture zones using a novel resorbable nanocrystalline hydroxyapatite paste in combination with a hydroxyapatite ceramic core: first clinical results. Arch Orthop Trauma Surg 2006; 126:533-540.
Author Info
Wafaa K Abid1* and Alyaa I. Naser2
1Department of Dentistry, Basrah, Iraq2Department of OMFS, College of Dentistry, University of Mosul, Iraq
Citation: Wafaa K Abid, Alyaa I Naser, Osteoconductive Efficacy of Marine Shells Nanoparticles Hydroxyapatite in Bone Regeneration-An Experimental Study in Rabbits , J Res Med Dent Sci, 2021, 9(7): 77-84
Received: 05-Jun-2021 Accepted: 07-Jul-2021