Review Article - (2022) Volume 10, Issue 11
Outcome of New-born born to Mother with Hypertension in Pregnancy
Apoorv Jain* and Amar Taksande
*Correspondence: Dr. Apoorv Jain, Department of Pediatrics, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences (Deemed to be University), Wardha, Maharashtra, India, Email:
Abstract
Preeclampsia is a multi-organ, heterogeneous pregnancy disorder that is associated with large number of maternal and new-born morbidity and mortality. As the preeclampsia is a progressive disease, delivery may be necessary in some circumstances to prevent the disease from advancing for the benefit of neonate and the mother. Premature birth has long term detrimental effects on critical neonatal outcomes that aren't limited to the most premature new-borns. Late preterm infants account for around two thirds of all preterm deliveries and they have a significant morbidity and mortality rate. In the current literature we will review the definition, physiology and various outcomes of new-born born to pregnancy induced hypertensive mothers.
Keywords
Pregnanacy, Hypertension, Neonate, Outcome, Eclampsia
Introduction
Hypertension in pregnancy is one of the leading causes of maternal mortality and morbidity, accounts for about 10-15% of all fatalities related to mother, particularly in the underdeveloped countries [1,2]. It can lead to multiple complications in 3-10% of all the pregnancies, with varying rates in multiple institutions and countries [3].
The following four categories are recognised by international guidelines:
• Chronic or pre-existing hypertension: Hypertension which has been discovered prior to conceiving and/or before the twentieth pregnancy week.
• Gestational hypertension: Hypertension that occurs after twentieth weeks of pregnancy and goes away once the baby is born.
• Preeclampsia eclampsia: De novo hypertension with at least one of the following signs and symptoms after 20 weeks of pregnancy.
• Proteinuria
• Other signs and symptoms of maternal organ dysfunction, such as acute kidney injury (creatinine 90 mol/L; 1 mg/dL), liver involvement (elevated alanine aminotransferase or aspartate aminotransferase >40 IU/L) with or without right upper quadrant or epigastria abdominal pain, neurological complications (eclampsia, altered mental status, blindness, stroke, clonus).
• Placental and uterine dysfunctions (for example, foetal growth limitation, aberrant umbilical artery Doppler waveform analysis, or still birth).
• Chronic/pre-existing hypertension superimposed eclampsia/preeclampsia.
Eclampsia/preeclampsia signs and symptoms after 20 weeks of pregnancy.
It's important to rule out secondary causes of hypertension while diagnosing and treating it during pregnancy. These factors have the potential to cause morbidity and death in both the mother and the child. Chronic renal disease, hyperaldosteronism, renovascular disease, obstructive sleep apnoea, Cushing's syndrome, pheochromocytoma, thyroid disease, rheumatologic illnesses (such as scleroderma or mixed connective tissue disease) and aortic coarctation are all secondary causes of hypertension.
For the definition of hypertension in pregnancy, the "national high blood pressure education program working group on high blood pressure in pregnancy" [4] recommends a Systolic Blood Pressure (SBP) of 140 mmHg and/or a Diastolic Blood Pressure (DBP) of 90 mmHg. In most cases, two measurements are required to make a diagnosis.
The following is a list of hypertension's severity:
• Non severe hypertension: Any SBP readings between 140 and 159 mmHg and DBP readings between 90 and 109 mmHg. This category is referred to as "light" as a whole or as mild (140–149/90–99 mmHg) and moderate (150–159/100–109 mmHg).
• Severe hypertension (high blood pressure): The blood pressure of 160 mmHg SBP and/or 110 mmHg DBP.
As it is being recognised that pregnant women can get hypertensive encephalopathy at lower blood pressures than non-pregnant individuals, the criteria for severe hypertension in pregnancy are lower.
Literature Review
Physiology of hypertension
Significant amount of changes occur in cardiovascular and renal function throughout normal pregnancy to complete the maternal and foetal metabolic needs. To consider as an example, cardiac output and blood volume of the mother rise by 40% to 50%, whereas there is decrease in total amount of peripheral resistance and arterial Blood Pressure (BP). Furthermore, significant changes occur in the function of the kidney, for example there are thirty to 40% increase in renal plasma flow and glomerular filtration rate. The renin, renin activity, and angiotensin II levels are all elevated; then also the angiotensin II response on vessels appears to be less. Endothelial factor i.e. nitric oxide play a major role and this has been concluded after complete exploration about the process of cardiovascular and renal changes (Figure 1).
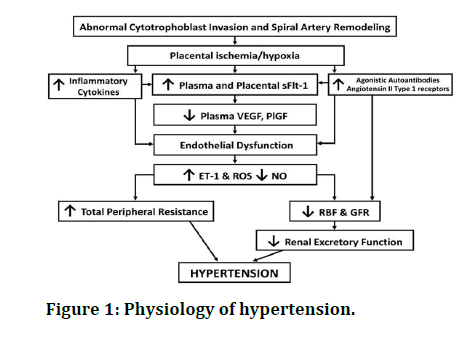
Figure 1: Physiology of hypertension.
Various Outcomes neonates to PIH mother
Intrauterine Growth Restriction (IUGR): IUGR, also called as the foetal growth restriction, is a condition in which a foetus grows slowly while in the womb of the mother during pregnancy; regardless the neonates’ percentile of the birth weight, IUGR is being defined [5] by the evidence of stunted growth and the clinical indications of malnutrition.
Types: True IUGR and pseudo IUGR are the two main types of IUGR.
The birth weight of a baby with pseudo IUGR is below the tenth percentile for gestational age, yet the ponderable index, subcutaneous fat accumulation, and body proportion are all normal.
These new-borns can be called as baby’s small for gestational age.
IUGR i.e. true is caused by pathologic abnormalities that can be foetal or maternal in nature. They have body disproportion, abnormal ponderable index and less subcutaneous fat deposition in addition to their less weight of the body.
Asymmetrical and symmetrical are the two categories [6].
IUGR can be due to number of reasons, including maternal, foetal, and genetic and the placental factors (Table 1).
Risk factors for IUGR
| Maternal | Uteroplacental | Fetal | Genetic |
|---|---|---|---|
| Malnutrition | Preeclampsia | Chromosomal abnormalities | Placental genes |
| Anaemia | Multiple gestation | Infections that are vertically transmitted i.e. congenital HIV infection, syphilis, malaria and TORCH infections. | Genes of the mother: Leptin under expression, endothelin-1 over expression. |
| Substance abuse: Drugs including marijuana or cocaine, alcohol and smoking. | Uterine malformations | Erythroblastosis fetalis | Fetal genes |
| Medication: Warfarin, steroids, anticonvulsants | Placental insufficiency | Congenital abnormalities | |
| Gestational diabetes | |||
| Disease of the pulmonary system | |||
| Disease of cardiovascular system |
Table 1: Risk factors for IUGR.
Low Birth Weight (LBW): LBW is defined as the birth weight of neonate less than 2.5 kg, in spite of gestational age by the World Health Organization.
The following categories apply to birth weight.
• Macrosomia=more than 4.2 kg
• Average birth weight=2.5–4.2 kg
• LBW ≤ 2.5 kg
• <1.5 kg=very LBW
• <1 kg=extremely LBW
Causes: Preterm birth (a baby with low for gestational age at birth, usually less than thirty seven weeks) or small for gestational age neonate (a slow prenatal growth rate), or a combination of the two, causes LBW.
Young age group, multiparous women, early history of low birth weight infants, poor nutritional status, any disease of the heart or hypertension (raised blood pressure), non-treated celiac disease, substance abuse disorder, heavy consumption of alcohol, incorrect antenatal care are all risk factors for the mother's low birth weight. It could also be caused by a ruptured membrane before to labour. Risk factors related to environment [7] which includes exposure to smoke, exposure to lead, and other forms of pollutants of air.
Stillbirth: Stillbirth is being defined as the death of the foetus at or after 20th weeks or 28th weeks of gestational age. Stillbirth is defined as the baby who is born without any indications/signs of life [9].
According to the World Health Organization, every new born who is born without any indicator of life at ≤ 28 weeks gestation have to be classified as a stillbirth using ICD-10 guidelines. Stillbirth is defined by the WHO [ ] as per the ICD-10 "late foetal deaths” definition. The cause of still birth is not frequently known. Complications related to the pregnancy like preeclampsia (increased Blood pressure) and complications related to birth, abnormality with the placenta or umbilical cord. Other possible causes include birth abnormalities, diseases, for example syphilis, malaria, and poor mother health. Risk factors include women above the age group of 35 years, smoking and misuse of drug, assisted reproductive technology use and first pregnancy [8].
Diagnosis: Though it is usual for a foetus who is healthy to show close to the end of a pregnancy such type of changes as there is substantially less volume of space in the uterus for the baby to move around than earlier in pregnancy, it is not uncommon for a sick foetus to show such changes. A decrease in or complete stoppage of foetal activity could indicate pain or death in the foetus. If there is any transformation in the power or number of cycles of foetal movement, importantly a complete cessation, a medical examination, including a non-stress test, is essential; to help identify any changes, most midwives and obstetricians advise using a kick chart. To confirm or rule out foetal suffering or death, fetoscopy/ doptone, ultrasound, and/or electronic foetal monitoring can all be employed [10].
Necrotising enterocolitis: NEC is a life threatening intestinal illness that affects new-borns who are born preterm or with a low birth weight [11].
Signs and symptoms: Premature babies are more likely to develop the condition, and the gestational age of the new-born is usually inversely proportional [12] to the onset of the disease (i.e., if the baby is born early then signs of NEC will be seen later).
Increased residuals of stomach, distension of abdomen, and stools containing blood are the early indications, followed by feeding intolerance and failure to thrive. Abdominal discoloration, intestinal perforation, peritonitis, and systemic hypotension are all symptoms that require prompt medical intervention.
Diagnosis: To confirm the diagnosis, diagnostic imaging, most commonly used is x-ray radiography, which shows the intestinal and can visualise the areas with dead tissue or an area of bowel perforation, is sometimes necessary.
Prevention: Breast milk and probiotics are two methods of prevention [13]. The paediatrics American academy advised feeding with human milk to the premature babies in 2012, citing "strong long and short term benefits, "including a reduction in the NEC rate by half to three quarters. While the infant is mostly fed intravenously, tiny volumes of human milk oral feeds are introduced as soon as possible to help the immature gut grow and prepare for more absorption by mouth.
Treatment: If any of the new-born is being diagnosed with NEC, treatment should be given as early as possible. Supportive management includes the cessation of enteral feedings, decompression of the stomach with suctioning intermittently, rectifying electrolyte imbalances with replacement with fluids and losses related to third spaces, blood pressure support, parenteral nutrition, and early antimicrobial medication [14]. Although repeated left lateral decubitus and supine abdominal x-rays to be performed every six hourly whereas usually the monitoring is clinical.
After the recovery stage from NEC feeds are gradually started. Decreased (low) volume feeding initially, sometimes known as "trophic feeds" is usually initiated first.
Respiratory Distress Syndrome (RDS): RDS, also known as Hyaline Membrane Disease (HMD) [15], is the most common clinical condition in premature babies. It is caused by structurally immature and surfactant deficient lungs.
Treatable and preventable factors aggravate the condition, including hypoxia, acidosis, secondary surfactant inadequacies meconium aspiration syndrome, diabetic mother's infant, pneumonia, cold stress.
The diagnosis is based on a combination of clinical characteristics, which include: tachypnoea, cyanosis, higher oxygen need, nasal flaring, grunting respirations, and intercostal retraction.
Investigation
Chest x-ray
• Widespread ground glass lungs.
• Usually bilateral and symmetrical.
• Air bronchograms may be visible.
• Hyperinflation (in a non-ventilated patient) rules out the diagnosis.
Management: Non-respiratory management of RDS temperature control, enteral feeding should generally be avoided; Minimal handling is imp ortant, antibiotics. Respiratory management of RDS airway, oxygen.
Neonatal sepsis: Neonatal sepsis is a type of neonatal sickness that occurs when a new-born baby has a fever and has a bacterial Blood Stream Infection (BSI) (such as meningitis, pneumonia, pyelonephritis, or gastroenteritis). The two varieties of neonatal sepsis are sepsis with Early on Set (EOS) and sepsis with Late on Set (LOS). Sepsis that appears within the first 72 hours is known as EOS, whereas sepsis that appears after 72 hours is known as LOS.
In both hospitals and the community, new-born sepsis is the primary cause of infant death in developing countries.
Symptoms and signs: The following are non-specific indicators [16] of sepsis: Changes in body temperature, breathing difficulties, diarrhoea, hypoglycaemia (low blood sugar), reduced motions, reduced sucking, seizures, yellow skin and whites of the eyes, bradycardia, swollen belly area, vomiting, rash with haemorrhage.
Diagnosis
New-born septic screening
• DLC (Differential Leukocyte Count) indicating large number of neutrophils in new born sepsis screening.
• DLC: Band cells greater than 20%.
• Higher haptoglobin levels.
• Erythrocyte Sedimentation Rate (ESR) titter >15 mm.
• Gastric aspirate with more than five polymorphs per high power field.
• Screening of neonatal CSF (cerebrospinal fluid) reveals an increase in cells and proteins.
• PROM (premature rupture of membranes), chorioamnionitis, and other possible causes.
Microbial culture is the gold standard method for the diagnosis of neonatal sepsis obtained from the blood, urine and CSF sample
Treatment: It's worth mentioning that sepsis in newborns is often difficult to identify. Because the new-born may be asymptomatic until there is imminent hemodynamic and respiratory collapse, these neonates with suspected sepsis are mostly treated with empirical antibiotics until the cultures come to be negative. Beta lactam group of antibiotics i.e. usually ampicillin and aminoglycoside i.e. usually gentamycin or cephalosporin usually third generation i.e. cefotaxime that is commonly used (generally ceftriaxone is not used in neonates as it can lead to kernicterus) is a common antibiotic regimen which is commonly used in new-borns with suspected sepsis. Pathogens such as group B Streptococcus, Listeria monocytogenes and Escherichia coli, that thrive in the genitourinary tract of the females and are particularly hazardous to baby.
Meconium Aspiration Syndrome (MAS): The first faeces, or stool, of a baby is called meconium. Around the moment of delivery, a new-born breathes a mixture of meconium and amniotic fluid into the lungs, causing meconium aspiration syndrome [17].
Symptoms include: Bluish skin tone in the new-born, breathing difficulties, dark, greenish staining or streaking of the amniotic fluid; or the presence of meconium in the amniotic fluid; and limpness in the infant during delivery.
Diagnosis
• Meconium can be found in the amniotic fluid during birth, and the foetal monitor may reveal a sluggish heart rate before birth. Looking for meconium staining on the vocal cords with a laryngoscope is the most accurate test for suspected meconium aspiration.
• A stethoscope is used to detect abnormal breath sounds, particularly coarse, crackly noises.
• A blood gas study reveals low blood acidity, low oxygen, and high carbon dioxide levels.
• Patchy or streaky patches on the lungs may be seen on a chest x-ray.
Treatment: As soon as the head is seen during delivery, suction the new-born’s mouth. If there is thick meconium staining and foetal discomfort, more treatment is required. The baby may be admitted to the new-born intensive care unit or the special care nursery.
Other treatments may include:
• Antibiotics for infection.
• A breathing machine to keep the lungs inflated.
• A warmer to keep the body warm.
• Tapping on the chest to loosen secretions.
Birth asphyxia: . Birth asphyxia occurs when a baby does not receive enough oxygen before, during, or soon after birth.
Babies may recover completely in mild or moderate cases. Birth asphyxia, on the other hand, can cause lasting brain and organ damage or even death in severe situations.
The following are risk factors for birth asphyxia: Numerous births, such as delivering twins or triplets, not attending prenatal care, low birth weight, improper position of the foetus during delivery, preeclampsia or eclampsia, previous birth asphyxia, antepartum and intra partum anaemia.
Symptoms and signs: Symptoms of birth asphyxia can arise before, during, or soon after birth. A new-born’s heart rate or blood pH levels may be abnormal before birth, indicating an excess of acid.
A shortage of oxygen or blood flow in the new-born might be detected at birth and other manifestations that can be detected, some of them among are: Low heart rate (bradycardia) and poor muscle tone (hypertonia), sluggish reflexes, inability to breathe or difficulty breathing, meconium tainted amniotic fluid, skin discoloration, seizures, low blood pressure, inability to urinate, irregular blood clotting, poor circulation, limp or lethargic baby. A low Apgar score is another indicator.
Treatment: The degree and aetiology of the birth asphyxia will determine the method of treatment.
The following are immediate treatments:
• Extra oxygen for the expectant mother if she suffers from birth asphyxia before giving birth.
• Caesarean or emergency delivery
• If meconium aspiration syndrome occurs, suction fluid from the airways.
• Placing the baby on a breathing machine.
Severe cases of birth asphyxia are treated by:
• Putting the new-born in a hyperbaric oxygen tank, which gives him 100% oxygen.
• Blood pressure medicine; dialysis to strengthen the kidneys and eliminate waste; seizure medication.
• A tube for inhaling nitric oxide.
• A heart and lung pump to keep you alive.
Discussion
The aim of this study is to assess the effect of pregnancy induced hypertension on adverse perinatal outcomes. Based on this we will try to find that women with PIH shows a higher risk of adverse perinatal outcomes such as low birth weight, birth asphyxia, small for gestational age, preterm delivery, stillbirth, admission to NICU and perinatal death compared to normotensive pregnant women.
The burden of PIH is common in India. Many mothers and new-borns are affected by the adverse outcomes of PIH. There are many causes for this problem such as poor access to health service and quality of maternal and newborn care in India. Therefore, the rationale for this study is to help policymakers and programmers to have a clear picture about the effect of PIH on adverse perinatal outcomes to make evidence based decision and mobilize resources for the management of PIH and its associated perinatal complications in the region. It will also guide health care providers working in clinical areas to make evidence based decisions for the prevention and management of adverse perinatal outcomes of PIH.
Conclusion
• Pregnancy Induced Hypertension (PIH) is a maternal condition that involves placental alterations and is linked to perinatal problems. Preeclampsia causes significant foetal morbidity and mortality, which can be attributed to poor care. Because babies delivered to hypertensive moms are more likely to have difficulties, they should be closely monitored in order to reduce morbidity and promote growth and survival. Prematurity and low birth weights are the leading causes of perinatal mortality in this group of babies.
• As a result, all pregnant women should receive comprehensive antenatal care to avoid and screen for preeclampsia. Improved public health awareness, primary health care provider education, and socioeconomic conditions can all help to enhance new-born prognosis.
References
- Gracia VDP, Rueda MC, Ruiz J. Expectant management of severe preclampsia and preeclampsia superimposed on chronic hypertension between 24 and 34 weeks gestation. Eur J Obstet Gynecol Reprod Biol 2003; 107:24-27.
- Barron WM, Murphy MB, Lindheimer MD. Management of hypertension during pregnancy. Laragh JH, Brenner BM. hypertension: Pathophysiology, diagnosis and management. 1990; 2:2427-2450.
- Chobanian AV, Barkris GL, Black HR, et al. Seventh report of the joint national committee on prevention, detection, evaluation and treatment of high blood pressure. Hypertension 2003; 42:1206â??1252.
- Expectant management of severe preclampsia and preeclampsia superimposed on chronic hypertension between 24 and 34 weeks gestation
- Kesavan K, Devaskar SU. Intrauterine growth restriction: Postnatal monitoring and outcomes. Pediatr Clin North Am 2019; 66:403-423.
- Hunter SK, Kennedy CM, Peleg D. Intrauterine growth restriction: Identification and management. Am Fam Physician 1998; 58:453-467.
- Rizzo N, Simonazzi G, Curti A. Obstetrical risk factors of ELBW. Ital J Pediatr 2015; 41:1.
- Lawn JE, Blencowe H, Waiswa P, et al. Stillbirths: rates, risk factors, and acceleration towards 2030. Lancet 2016; 387:587â??603.
- Bamber AR. "Macerated Stillbirth". In Khong TY, Malcomson RD (eds.). Keeling's fetal and neonatal pathology. Cham: Springer international Publishing. 2022; 345â??368.
[Crossref]
- Gravett C, Eckert LO, Gravett MG, et al. "Non-reassuring foetal status: Case definition and guidelines for data collection, analysis, and presentation of immunization safety data". Vaccine 2016; 34:6084â??6092.
- Gephart SM, Quinn M. A call to action to fight for equity and end necrotizing enterocolitis disparities. Adv Neonatal Care 2021; 21:333-335.
- Yee WH, Soraisham AS, Shah VS, et al. Incidence and timing of presentation of necrotizing enterocolitis in preterm infants. Pediatrics 2012; 129:e298-e304.
- Palleri E, Aghamn I, Bexelius TS, et al. The effect of gestational age on clinical and radiological presentation of necrotizing enterocolitis. J Pediatr Surg 2018; 53:1660-1664.
- Heird WC, Gomez MR. Total parenteral nutrition in necrotizing enterocolitis. Clin Perinatol 1994; 21:389â??409.
- Thompson BT, Chambers RC, Liu KD. Acute respiratory distress syndrome. N Engl J Med 2017; 377:562-572.
- Ohlin A, Bjorkqvist M, Montgomery SM, et al. Clinical signs and CRP values associated with blood culture results in neonates evaluated for suspected sepsis: Clinical signs in neonatal sepsis. Acta Paediatr 2010; 99:1635â??1640.
- Van Ierland Y, De Beaufort AJ. Why does meconium cause meconium aspiration syndrome? Current concepts of MAS pathophysiology. Early Hum Dev 2009; 85:617â??620.
Author Info
Apoorv Jain* and Amar Taksande
Department of Pediatrics, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences (Deemed to be University), Wardha, Maharashtra, IndiaCitation: Apoorv Jain, Amar Taksande, Outcome of New-born born to Mother with Hypertension in Pregnancy, J Res Med Dent Sci, 2022, 10 (12): 001-006.
Received: 29-Sep-2022, Manuscript No. JRMDS-22-64962 ; , Pre QC No. JRMDS-22-64962(PQ) ; Editor assigned: 01-Oct-2022, Pre QC No. JRMDS-22-64962(PQ) ; Reviewed: 15-Oct-2022, QC No. JRMDS-22-64962 ; Revised: 29-Nov-2022, Manuscript No. JRMDS-22-64962(R) ; Published: 08-Dec-2022
