Research - (2022) Volume 10, Issue 1
Pit and Fissure Sealants
Yukta N Umalkar*, Nikhil Mankar, Rutuja Rajnekar and Seema Sathe
*Correspondence: Yukta N Umalkar, Department of Conservative Dentistry and Endodontics, Sharad Pawar Dental College and Hospital, Datta Meghe Institute of Medical science (Deemed to be University), Sawangi (Meghe), Wardha, Maharashtra, India, Email:
Abstract
Carious infections of the teeth are considered a major worldwide concern, resulting in significant health, safety, and quality-of-life issues for those patients who suffer from these infections. Routine oral hygiene along with fluoride use helps prevent dental caries. Another prophylactic measure against decay taken with packing the pits and fissures of tooth that tends to get caries. This article's main objective is to present a general overview of packing of grooves, as well as implications and side effects of the materials generally used to seal occlusal surfaces. Furthermore, this article reviews pit and fissure sealants as protective way for caries and also a review in their safe, effective use and cost effectiveness. Based on the findings, our conclusion is that sealing cavities is a productive and appropriate way for stopping and arresting dental caries in mixed and adult teeth. To ensure that there is no advanced tooth decay caused by sealing leakage, a regular dental check-up is necessary.
Keywords
Pits and fissures of tooth, Tooth decay, Carious infections
Introduction
Caries is a multidimensional disease occur when the framework of a microorganisms coating varies, the demineralization and remineralization processes become imbalanced, caries form in both milk and fixed adult teeth [1]. Caries cases increasedmost innineteenth and twentieth centuries because sugar was more easily accessible to the public [2]. Caries is important problem and quality of life threat even in the 21st century [3]. 37 percent of children of 2-8 shows caries in their primary teeth, twenty-one percent of children of 6-11 shows cavities in their fixed teeth, while fifty-eight percent of children of 12-19 shows cavities in their fixed teeth. Compared to earlier survey of 1999–2004, number of cavities among milk teeth has declined, while % of cavities in permanent teeth has decreased slightly [4,5].
The term dental sealant describes procedure of introducing substance on occlusal surface of tooth that is subject in formation of cavities, thereby creating a shielding layer that cuts off sources of nutrients for bacteria that produces caries [6]. It is the molar teeth that experience the number of decay in milk teeth of children and fixed teeth of adolescents [7,8]. When chewing, buccal and lingual areas, molar teeth have numerous grooves (fissures) and pits, making them difficult to properly floss.
This is the most likely place for decay to occur [9].
According to a dental caries risk assessment, primary teeth with fissure anatomy or patient caries risk factors are at risk for caries, and therefore should be sealed with dental sealant [10].
Due to the difficulty of performing this procedure on primary teeth as there are various factors like lack of cooperation, behaviour and age towards dental setup, many studies tells that the amount of time spent etching has a little impact on sealant retention [11].
Further, studies have found that GI sealants are more moisture-resistant than resin-based sealants and when salivary contamination predicted, this may be a useful intermediate choice [12].
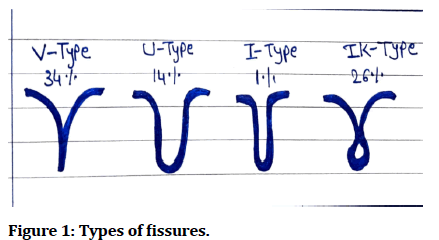
Types of fissures
In the posterior teeth, because of their morphological complexity, the occlusal surfaces of pits and fissures are highly vulnerable to cavities formation than smooth surfaces that makes plaque easier to accumulate.
Fissures with shallow and wide 'V' or 'U' shapes are selfcleaning and have a limited susceptibility to caries, whereas fissures with 'I' or 'K' shapes are very susceptible to caries (Figure 1).
Figure 1: Types of fissures.
Requisites of an efficient sealant
• The viscosity of this paste permits penetration even into fissures as deep as the maxillary teeth.
• A sufficient amount of working time.
• Cure fast
• Adhesion to enamel is good and for longer time.
• Solubility and sorption are low.
• Defeats wear and tear.
• Less irritation to tissues.
• Has cariostatic effect [13].
Clinical indications for PFS
Indications
• A permanent tooth's occlusal surface is characterized by well-defined pits and fissures and/or deep fossea. The grooves and pits in primary molars may be sealed if they are significantly deep.
• Patients having high caries incidence, pits and fissures may appear stained or white
• Gingival and operculum grooves that are free of gingival and operculum contact when only the appropriate teeth have erupted.
• Incisors havingpits and fissure lingually.
• Children with deep or stained fissures and pits in primary teeth, or those with caries in the contralateral primary molar, should have a sealant fitted [14].
• Sealing is especially relevant to children and young people with physical, medical andsome disabilities [15].
Contraindications
• Porcelain restorations made from synthetic materials.
• Veneers.
• Restorations containing amalgam.
• Restorations, onlays, inlays, or crowns in gold foil.
• Cavities on occlusal, interproximal areas of teeth.
• Teeth that are not sufficiently isolated.
• Previously restored nonresin areas that need sealing.
• Its retention rate is significantly lower than enamel and it is more sensitive.
• Children of very small age and do not cooperate in treatment.
Polymerization methods
• (Mixing two components) self-activated
• Light activated
• UV-activated sealants are the first generation of sealants.
• Second generation sealants are chemically cured.
• Third generation sealants are visible light cured.
• Fourth generation sealants are fluoride-containing sealants.
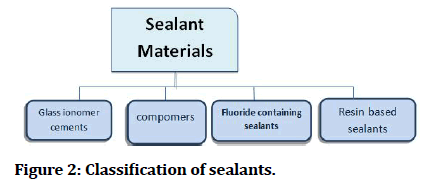
Classification of sealants
Resin-based Sealants (RBSS)
On the basis of polymerization, Resinbased sealants are dividedin to:
• 1st gen: Polymerization is initiated by initiators that are polymerized by UV light. This kind of sealant is not currently being used. One example of a 1st generation resin-based sealant is Nuva-seal, which was first introduced to the market.
• 2nd gen: Also called chemically cured sealants, these resin-based sealants auto-polymerize. However, the 3rd era of RBSs has now supplanted the second era.
• 3rd gen: Using visible light for this type of polymerization involves resin-based sealants. The visible light activates a photo initiator that is present within the sealant. The photo initiator is highly responsive to visible light at around 470nm (purple area) [16].
Resin-based sealants are also classified on the basis of the consistency as (1) Filled (2) Unfilled.
• While filled sealants are highly wearable, they have a difficult time entering fissures and pits. while unfilled sealantsshows low flowability but provide an even perforation, resulting in improved retention.
On the basis of translucency sealant materials are also divided as transparent and opaque.
• A transparent sealant appears as clear, pink, or amber, whereas an opaque sealant is white or toothcoloured. Dental sealants that are white opaque is easier to see while applying and will be easier to identify clinically throughout routine check-ups and follow-ups than those that are clear (Figure 2) [17].
Figure 2: Classification of sealants.
Glass ionomer sealant material
Glass ionomer products are accustomed as dental sealants traditionally. Chemical link between enamel and dentin is formed by a base and acid reaction in the aqueous-based polyacrylic acid solution and fluoroalluminosillicate powder that contain glass. Such type of sealant is further categorized as
• Low type of viscosity.
• High type of viscosity.
As a pit and fissure sealant, you can use resin-modified glass ionomer (RMGIC). The strength of GI cement-based sealants is their continuous fluoride release, as they are formed when resin and glass ionomer cement are mixed together. These materials are moisture controlled and is easily applicable. Glass ionomer sealants are mainly indicated primary molar having deep fissure whose isolation is not easy because of the child’s uncontrollable behaviour [18].
Compomers
In dentistry compomers are also known as polyacidmodified resin composite which are used as a filling material. There are compomers whichare modified dental materials with the advantages of composites and glass ionomers. This material is made up of 2 elements: the dimethacrylate monomer along with the 2 carboxylic groups in its composition with filler which is akin to glass found in glass ionomer cement. The ratio is 1:8 of the carboxylic groups which has foundation carbon atoms in it. Water is absent in the composition of such materials and to ensure some bonding between the matrix and the ion-leachable glass, the glass is incompletely covered. These materials don’t interact with cells of firm teeth tissues since it is set by free radical polymerization, [19] and has low levels of fluoride release than GICs [20,21]. Investigation on compomers is still going on widely in both in vivo and in vitro. Compared with GIC, distilled water emits substantially less F than does GIC [22]. The aesthetics of composites are obviously superior to those of dental amalgams. Since compomers are tooth coloured, their aesthetics stand out immediately. As compared to resin modified glass ionomer cements compomers acts better aesthetically. They are also present in various non-natural colors for deciduous teeth from a wide range of dental companies. As compared to standard type of GI, the resin modified glass ionomers along with thecompomers has good aesthetic quality. In cases where a patient's likelihood of suffering from tooth decay in the future is higher, compomers and glass ionomer cements can release fluoride.
Flouride-containing Sealants
It was tested to see how well the fluoride-containing sealant (FluroShield) penetrated fissures, resisted microleakage, and released fluoride. This sealant was compared to one without fluoride. FS containing F now appears to be as conducted over long periods of time to determine whether the presence of incorporated F affects the durability of FS. It remains to be seen what clinical significance the F ion has in terms of caries prevention in F containing FS [23].
Flouride application methods of fissure sealantsare
There are 2 routes of fluoride application in dental sealants:
• Sealant degrades and releases fluoride ions after its administration on tooth and in 1st step the fluoride is mixed to the unpolymerized resin and fluoride salt is dissolved in water.
• A second method involves chemically binding natural fluoride mixture with resin, followed by an exchange with another ion [24].
Clinical technique
STEP 1: To prevent salivary contamination isolation of tooth surface.
STEP 2: Preparation of tooth.
STEP 3: Etching.
STEP 4: Rinse and etch dry.
STEP 5: Application of the sealant substance.
STEP 6: Examining the surface of a sealed tooth.
STEP 7: Examine the sealed surface's occlusion.
STEP 8: When needed, reassessment and reapplication of sealant material.
Recent advances in pit and fissure sealants
On employing the fluoride-releasing flowable resin, for a fissure sealant in younger children's enamel caries of permanent molars that increase sealant retention value that successfully inpet enamel caries progression when compared to traditional fissure sealants. On of 12 and 24 months, clinical impact of fluoride-releasing flowable resin utilised in the curing of early enamel caries in the young child was contrasted to that of traditional sealant the fluoride releasing flowable resin group saw a greater reduction in caries progression than the manage classand there was a qualitative dissimilarity in two categories [25].
Nanocomposites as pit and fissure sealants
Although it displays modest microleakage, nanocomposite has been shown to be an effective dental material for penetration in deep pits and cracks. As a result, it can be suggested for use as a pit and fissure sealant in juvenile dental patients [26].
Colour changing sealants
Very 1st coloured sealant the 3M's Concise White Sealant, got released to the square in March 1977. A white sealant is trouble free to look during its use, and a white sealant is fast and easier for examine at later time intervals than a clear sealer [27].
Hydrophobic and hydrophilic pit and fissure sealants
Hydrophilic sealants can be handle as effectual pit and fissure sealants in the young age patients who are at big chance of caries, who are highly salivating, who are handicapped, then very young, have uncooperative children, have half of erupted molars, that are enrolled in community protection programmes [28].
Cost-effectiveness of dental sealants
There is no doubt that dental sealants are a cost-effective procedure. By preventing the need for more intrusive and expensive restorative treatments, sealing permanent molars lowers the overall cost. When used on high-risk children and on surfaces susceptible to decay, sealants are considered more cost-effective. So it is advised that sealants can be used on the basis of child’s fissures anatomy and caries risk [29,30].
Narrow, deep I-shaped fissures are somewhat more susceptible to caries in comparison to V-shaped fissures which are shallow and wide [31]. Permanent first molars that have just emerged should likewise be considered decay-prone. These teeth should be protected from caries and sealed at the earliest opportunity. Buccal pits and lingual grooves are also vulnerable to caries whose sealing is difficult [32].
In high risk caries patients application of sealant should be a part of caries management protocol [33]. Fluoridated toothpaste, fluoride supplements, and expert topical fluoride treatment are all recommended and diet counselling, evaluating to what extent other preventive approaches are used is important [23]. several indicators are used to assess caries risk, including low socioeconomic status, past caries experience, sugar intake between meals, and active white spot lesions.
Conclusion
Carious lesions most commonly occuron the occlusal surfaces. It is impossible to foresee which teeth will become carious but if the surface is sealed with a pit and fissure sealer, no caries will form as long as the sealant is kept in place. Sealant can additionally prevent caries progression on teeth with early non-cavitated carious lesions. The method of application of sealant is a technique sensitive method that needs an environment which is moisture controlled. The material used is determined by the patient's behaviour, the child's age, and the timing of tooth eruption. Teeth with early noncavitated carious lesions can also benefit from sealant treatment to prevent caries development. Application of sealant needs moisture controlled environment as it is a sensitive procedure. To increase the efficiency and adequacy of the treatment maintenance is essential. Pit and fissure sealants must be used to prevent pit and fissure caries on primary and permanent teeth.It is therefore important for dentists to apply sealants to pits and fissures in patients at high risk for dental caries should be treated with additional preventative methods, as well.
References
- Young DA, Nový BB, Zeller GG, et al. The American dental Association caries classification system for clinical practice: A report of the American dental association council on scientific affairs. J Am Dent Assoc. 2015; 146:79-86.
- Naaman R, El-Housseiny AA, Alamoudi N. The use of pit and fissure sealants: A literature review. Dent J 2017; 5:34.
- Cvikl B, Moritz A, Bekes K. Pit and fissure sealants: A comprehensive review. Dent J 2018; 6:18.
- Dye BA, Tan S, Smith V, et al. Trends in oral health status; United States, 1988-1994 and 1999-2004.
- Dye BA, Thornton-Evans G, Li X, et al. Dental caries and sealant prevalence in children and adolescents in the United States, 2011-2012. NCHS Data Brief. 2015;(191):1-8.
- Simonsen RJ. Pit and fissure sealant: Review of the literature. Paediatr Dent 2002; 24:393-414.
- Elfrink ME, Veerkamp JS, Kalsbeek H. Caries pattern in primary molars in Dutch 5-year-old children. Eur Arch Paediatr Dent 2006; 7:236-240.
- Batchelor PA, Sheiham A. Grouping of tooth surfaces by susceptibility to caries: a study in 5–16 year-old children. BMC Oral Health 2004; 4:1-6.
- Slade GD, Spencer AJ, Davies MJ, et al. Intra‐oral distribution and impact of caries experience among South Australian school children. Aust Dent J 1996; 41:343-350.
- Feigal RJ. The use of pit and fissure sealants. Pediatr Dent 2002; 24:415-22.
- Chandak MS, Chandak M, Nikhade PP, et al. Role of liners in restorative dentistry. J Evol Med Dent Sci 2020; 9:1881-1887.
- Antonson SA, Antonson DE, Brener S, et al. Twenty-four month clinical evaluation of fissure sealants on partially erupted permanent first molars: glass ionomer versus resin-based sealant. J Am Dent Assoc 2012; 143:115-122.
- Brauer GM. Properties of sealants containing Bis-GMA and various diluents. J Dent Res 1978; 57:597-607.
- https://www.elsevier.com/books/pediatric-dentistry/nowak/978-0-323-60826-8
- Welbury R, Raadal M, Lygidakis NA. EAPD guidelines for the use of pit and fissure sealants. Eur J Paediatr Dent 2004; 5:179-184.
- Rathi SD, Nikhade P, Chandak M, et al. Microleakage in composite resin restoration-A review article. J Evolution Med Dent Sci 2020; 9:1006-1011.
- https://www.sciencedirect.com/book/9780323287456/mcdonald-and-averys-dentistry-for-the-child-and-adolescent
- Marwah N. Textbook of pediatric dentistry. JP Medical Ltd 2018.
- Martin R, Paul SJ, Lüthy H, et al. Dentin bond strength of Dyract Cem. Am J Dent 1997; 10:27-31.
- Forsten L. Flouride release of glass ionomers. J Esthet Restorative Dent 1994; 6:216-222.
- Jaiswal AS, Nikhade PP, Chandak M, et al. Colour stability of composite-A review. J Evol Med Dent Sci 2020; 9:1928-1935.
- Meyer JM, Cattani-Lorente MA, Dupuis V. Compomers: Between glass-ionomer cements and composites. Biomater 1998; 19:529-539.
- Jensen OE, Billings RJ, Featherstone JD. Clinical evaluation of Fluroshield pit and fissure sealant. Clin Prev Dent 1990; 12:24-27.
- Yan WJ, Zheng JJ, Chen XX. Application of fluoride releasing flowable resin in pit and fissure sealant of children with early enamel caries. Beijing Da Xue Xue Bao 2018; 50:911-914.
- Singh S, Pandey RK. An evaluation of nanocomposites as pit and fissure sealants in child patients. J Indian Soc Pedod Prev Dent. 2011;29(4):294.
- Garg N, Mayall SS, Pathivada L, et al. Combined effect of enamel deproteinization and intermediate bonding in the retention of pit and fissure sealants in children: A randomized clinical trial. J Clin Pediatr Dent 2018; 42:427-433.
- Puppin-Rontani RM, Baglioni-Gouvea ME, deGoes MF, et al. Compomer as a pit and fissure sealant: Effectiveness and retention after 24 months. J Dent Child 2006; 73:31-36.
- Wright JT, Crall JJ, Fontana M, et al. Evidence-based clinical practice guideline for the use of pit-and-fissure sealants: A report of the American dental association and the american academy of pediatric dentistry. J Am Dent Assoc 2016; 147:672-82.
- Rajnekar R, Mankar N, Nikhade P, et al. Dental burs in restorative dentistry and endodontics–past and present: A review. J Res Med Dent Sci 2021; 9:163-170.
- https://dental-library.com/pediatric-dentistry-infancy-through-adolescence-4th-edition/
- Feigal RJ. Sealants and preventive restorations: Review of effectiveness and clinical changes for improvement. Pediatr Dent 1998; 20:85-92.
- American Academy of Pediatric Dentistry. Guideline on caries-risk assessment and management for infants, children, and adolescents. Pediatr Dent 2013; 35:e157-64.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar Cross Ref
Indexed at, Google Scholar Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar Cross Ref
Indexed at, Google Scholar Cross Ref
Indexed at, Google Scholar Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Yukta N Umalkar*, Nikhil Mankar, Rutuja Rajnekar and Seema Sathe
Department of Conservative Dentistry and Endodontics, Sharad Pawar Dental College and Hospital, Datta Meghe Institute of Medical science (Deemed to be University), Sawangi (Meghe), Wardha, Maharashtra, IndiaCitation: Yukta N Umalkar, Nikhil Mankar, Rutuja Rajnekar, Seema Sathe,Pit and Fissure Sealants, J Res Med Dent Sci, 2022, 10(1):181-185
Received: 13-Dec-2021, Manuscript No. JRMDS-21-47329; , Pre QC No. JRMDS-21-47329 (PQ); Editor assigned: 15-Dec-2021, Pre QC No. JRMDS-21-47329 (PQ); Reviewed: 29-Dec-2021, QC No. JRMDS-21-47329; Revised: 03-Jan-2022, Manuscript No. JRMDS-21-47329 (R); Published: 10-Jan-2022
Copyright:
This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.