Research - (2022) Volume 10, Issue 1
Pre-Diabetes among HIV-Infected Individuals Receiving HAART: Prevalence, Diagnostic Tests, and Associated Factors, a Cross-Sectional Study
Saba Iqbal1*, Naheed Akhter2, Haseeb Mukhtar3, Hina Sadaf4, Sayed Asif Jahanzeb Kazmi5 and Zobiah Hafeez6
*Correspondence: Saba Iqbal, Department of Health Professions Education, CMH & IOD Lahore, Pakistan, Email:
Abstract
Background: In our common practice we use highly active antiretroviral therapy (HAART) which has resulted in a dramatic decrease in mortality and morbidity in HIV-infected patients. Components of HAART, as well as HIV infection itself, can have significant effects on developing new-onset diabetes and this risk will increase if the patient has a positive family history of diabetics. Objective: To determine the frequency of prediabetes among HIV-infected individuals. Methods: A cross-sectional study was conducted through a Non-probability consecutive sampling technique. A retrospective descriptive study was performed on 374 cases in the tertiary care centre in Lahore, Pakistan from September 2020 to April 2021 Results: The association between the prevalence of prediabetes and risk factors was analyzed. Among 374 HIV-infected patients, the mean age was 37.80 years, and 65% were male and 45% were female. Pre-diabetic patients’ means were 1.34 ± 0.477.family history of diabetics 1.34 ± 0.728. Linear correlation was seen between duration of HIV treatment and pre-diabetics, duration of HIV treatment, and marital status of the patient. Family history of diabetic Mellitus is correlated with age, pre-Diabetics with marital status. Conclusion: A high prevalence of prediabetes was observed in this cohort of HIV-infected patients. HAART regimes should be avoided in HIV-infected patients at high risk of developing diabetes, e.g., especially those with a history of positive family history of diabetes, or impaired OGTT. The regime should be avoided, and replaced with less toxic drugs.
Keywords
Diabetes, HAART, HIV infection, Diagnostic test, Prediabetes, Prevalence
Introduction
Human immunodeficiency virus (HIV) is a RNA virus that targets the body’s immune system and destroys the body’s defence mechanism. If HIV is not treated, it can lead to AIDS (acquired immunodeficiency syndrome). In recent years increase the number of cases might be due to increase in the awareness of scanning, early diagnosis, or better modes of treatment. According to the world health organization report 2016-21, HIV infection is prevalent in 27.2-47.8 million worldwide [1].
As the recent studies show, the natural history of the HIV infection is modified now [2]; from acute HIV infection some people have flu-like symptoms including fever, sore throat, body aches, mouth ulcers, etc., these are the body’s natural response to infection. These symptoms may progress after a few days to several weeks into noncommunicable diseases that recognized multiple complications of HIV infection, including dyslipidemia, hepatitis, insulin resistance, etc. [3,4]. As the infection progress further, the amount of human immunodeficiency virus in the blood i.e. called viral load will increase and the CD4 cell count decreases minnow the body defence mechanism is onto the west coast. To start the combined anti-retroviral therapy (HAART) has theatrically changed the natural history of HIV infection, life expectancy, and quality of life of patients. In 2020, about 26.5–27.7 million people world wildly received eg: HAART [5]. These benefits are, however, at the cost of HAART associated with elevated levels of oxidative stress on the body that induce cardiovascular diseases, dyslipidemia, insulin resistance and diabetes mellitus [6]. These appear to be increased by cumulative exposure, with the nucleoside reverse transcriptase inhibitors (NRTIs). In early stages NRTIs are most strongly implicated in the pathogenesis of HIV-related lip dystrophy [7]. Previous research has shown that antiretroviral medication, particularly NRTIs and PIs, can impact glucose metabolism, are linked to metabolic problems, and can add to the complexity of HIV-infected patients' care and management [8].
Pre-diabetics
Patients will be labelled as pre-diabetic when fasting plasma glucose level will be 100 to 125 mg/dl (Impaired fasting glucose) or 2-hour Plasma Glucose on the 75-g Oral Glucose Tolerance Test will be 140–199 mg/dl (Impaired glucose tolerance) [8]. In other words “Prediabetes, a condition in which blood sugars levels are fluctuates but not yet meeting the criteria for Diabetic Mellitus”, represents a high risk for future diabetes development.
ART The major contributor to hyperglycaemia in HIV/ AIDS treat patients. The effect of ART treatments in HIV can contributes in two main directions; at one side consequence of increased weight and improvement in well-being after initiating therapy; and on other side the specific effects of drugs on aspects of glucose metabolism [4]. It is well established through medical practice that we can delayed or prevent the patient from diabetics by using preventive measures and adopting healthy life style like, regular exercise, balanced diet and using medications like metformin [3]. Preventing the progression of prediabetes to diabetes and minimizing the possible consequences of prediabetes were the main goals of care for patients with prediabetes. As a result, detecting prediabetes in HIV-positive patients is critical for identifying those who require treatment to lower their diabetes risk in the future [7]. Recent studies of data shows between 2004–2011 periods, they found that HIV-infected patients had lower Diabetic mellitus incidence than HIV-uninfected patients [9]. Prediabetes, like diabetes, increases the chance of developing macrovascular problems such cardiovascular disease and stroke. Certain risk factors, such as being overweight or obese, being physically inactive, having a family history of diabetes, being of a certain ethnicity, and having gestational diabetes, all raise the chance of prediabetes [8]. Studies have been conducted on the prevalence of diabetes in HIV- infected patients in different regions of the world, but no recent studies have looked at the prevalence rate of prediabetes in this patient population in the Pakistan.
Objectives
The objectives of this study are to determine the frequency of prediabetes among HIV-infected individuals. Results of this study may help us for early management of prediabetes and decrease the morbidity rate related to it.
Materials and Methods
A cross-sectional study was conducted through Nonprobability consecutive sampling technique. A retrospective descriptive study was performed on 374 cases in tertiary care center in Lahore from September 2020 to April 2021. Sample size was calculated with 95% Confidence Interval. All the ethical guidelines were followed. Participation in this study was voluntary. The purpose of the study was explained to every patient and an informed consent was taken.
For each patient the following information will be collected using a standardized protocol: age, duration of HIV infection. Blood sample of each patient will be drawn and sent to the pathology laboratory of the hospital for analysis of fasting blood glucose levels, HBA1C, plasma glucose levels; oral glucose tolerance test and findings will be noted in term of pre-diabetes (Yes/No) as peroperational definition. Demographic profile of the patients will also be recorded in pre designed Performa.
Inclusion criteria
All HIV diagnosed male and female patient and age between 20 to 70 years. Diagnosed HIV patient, without any secondary illness except diabetic mellitus.
Exclusion criteria
Patient with any chronic illness like Tuberculosis or any heart diseases etc., pregnant women and Patients taking lipid lowering drugs etc.
Statistical analysis
All the data were recorded in pre-designed Performa. Data enter and analyzed in statistic program SPSS version 21.0.
Results
Patients Characteristics
Baseline characteristics a total of 374 HIV-infected patients under ART were evaluated. The mean age of patients included was 37.80 ± 12.78 years, and 65% of them were male and 35%were female. All the variables of the study i.e. age and duration of HIV infection, gender, and pre-diabetics condition, family history of diabetics and status of the patient were presented as Mean ± SD in (Table 1). The gender quantitative data were presented as frequency and percentages Pie chart. Results were analyzed after including all 374. Mean age was 37.80 ± 12.787 years, duration of HIV infection treatment mean is 5.31±2.859 (Table 2) (Figure 1).
| Mean | Std. Deviation | |
|---|---|---|
| Age | 37.8 | 12.787 |
| Duration of HIV treatment | 5.31 | 2.859 |
| Gender | 1.35 | 0.477 |
| Pre-Diabetics | 1.34 | 0.473 |
| status | 1.24 | 0.806 |
| Family history of diabetics | 1.34 | 0.728 |
Table 1: Mean and Std.Deviation of different qualitative and quantitative variables.
| Age | Duration of HIV treatment in years | Gender | Pre-diabetics | status | Family history of DM | |
|---|---|---|---|---|---|---|
| Age | 1 | 0.013 | -0.037 | -0.011 | 0.055 | -0.01 |
| 0.807 | 0.473 | 0.828 | 0.288 | 0.854 | ||
| Duration of HIV treatment in years | 1 | 0.043 | -0.006 | 0.018 | -0.047 | |
| 0.411 | 0.906 | 0.735 | 0.366 | |||
| Gender | 1 | -.401** | -0.03 | 0.007 | ||
| 0 | 0.565 | 0.899 | ||||
| Pre-diabetics | 1 | 0.075 | -0.006 | |||
| 0.147 | 0.906 | |||||
| status | 1 | 0.011 | ||||
| 0.83 | ||||||
| Family history of DM | 1 | |||||
| **. Correlation is significant at the 0.01 level (2-tailed) | ||||||
Table 2: Correlation Matrix of factors which influence the Diabetic mellitus in HIV infected patients.
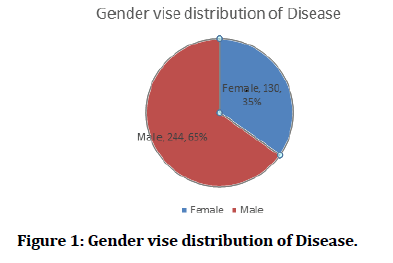
Figure 1: Gender vise distribution of Disease.
As the Table 2 shows, Perfect linear correlation seen between duration of HIV treatment and pre-diabetics, duration of HIV treatment and marital status of the patient. Family history of diabetic mellitus is strongly correlate with age, pre-Diabetics with marital status (Tables 3 and 4).
| Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â *FPG | Total | |||
|---|---|---|---|---|
| Â <100 100-125Â = 126 | ||||
| **HbA1c | ||||
| <5.7 | 256 | 36 | 0 | 292 |
| 5.7-6.4 | 13 | 12 | 1 | 26 |
| =6.5 | 6 | 2 | 48 | 56 |
| Total | 275 | 50 | 49 | 374 |
| FPG fasting plasma glucose, HBA1c haemoglobin A1c (p<0.001) | ||||
Table 3: Analysis of the agreement between hemoglobin A1c and fasting plasma glucose.
| Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â 2 hours plasma glucose | Total | |||
|---|---|---|---|---|
| Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â <140 140-199=200 | ||||
| *FBG | ||||
| <100 | 218 | 39 | 5 | 262 |
| 100-125 | 42 | 21 | 0 | 63 |
| =125 | 2 | 0 | 47 | 49 |
| Total | 262 | 60 | 52 | 374 |
| *FBG fasting blood glucose (p<0.001) | ||||
Table 4: Analysis of the agreement between fasting plasma glucose and 2-hours plasma glucose after performing 75gm oral glucose tolerance test (OGTT).
Measure of agreement
Analysis of all HBA1C and FPG measurements (n = 374) as shown in table no 3, cases of more than 100 FBG shows 356 patients HbA1C <5.7, 13 were range the 5.7-6. And 6 patients were ≥ 6.5. Fasting blood glucose levels were observed between the range of 100-125mg are, HbA1C <5.7 were 36 patients, range the 5.7-6 are 12 patients. And 2 patients were ≥ 6.5 HbA1C levels. Similarly FBG levels were observed between the range of ≥126mg are, HbA1C <5.7 were no patients observed, range the 5.7-6 is only 1 patient. And 48 patients were ≥ 6.5 HbA1C levels.
Tables 4 analyzed the 2-h BG and FBG measurements (n = 374). 2-h Blood Glucose after performing Oral Glucose Tolerance Test (OGTT) values more than 140mg whose fasting Blood Glucose were less than 100 are 218 patients, FBG levels between 100-125mg were observed in 42 patients and more than 125mg FBG found in only 2 patients. 2-h BG after performing OGTT values are range 140-199mg whose fasting Blood Glucose were less than 100 are 39 patients, FBG levels between 100-125mg were observed in 21 patients. 2-h Blood Glucose after performing Oral Glucose Tolerance Test (OGTT) values more than 140mg whose fasting Blood Glucose were less than 100 are 5 patients, and more than 125mg FBG found in 47 patients.
Discussion
The current study examined the prevalence, agreement among diagnostic methods, and correlation of associated factors of prediabetes among the diagnosed, HIV-infected individuals who are receiving ART for more than 1 year in teaching hospital Lahore, Pakistan. We observed a higher than expected prevalence of having prediabetes or diagnosed diabetes in patients who have positive family history of diabetics and in ambulatory HIV-infected individuals 25 years and older. In the study conducted in USA shows mean age of the HIV-infected was 16 or more [10,11], which is much lower than this study.
The socio-demographic characteristics of the study cohort were similar with us to the underlying HIVinfected population in the West and Central Africa, which is disproportionately represented by ethnic minorities and male gender [5,12].
Some correlation between the development of DM and the use of HAART was found. In this study, was found, the main cause of development of diabetes in patients with HIV/AIDS due to the use of HAART. Despite the benefits of using anti-retroviral, they can lead to metabolic changes such as insulin resistance, hypoproteinemia, diabetes mellitus, and dyslipidemia. Some studies shows diabetes can be four times more common in men with HIV receiving HAART than in men without HIV [13,8].
For the prediabetes diagnostic methods with or without the family history, we observed the interpretation varied throughout the three methods. Our results showed that FPG revealed the large numbers, whereas HbA1C revealed the small numbers of prediabetes diagnosis. This was consistent with previous findings done by Phuphuakrat et al [3].
In our study, we were doing the detailed analysis of blood glucose estimation by using different methodologies. Although this was the cross-sectional study, but we repeat the tests in the absence of unequivocal hyperglycaemia according to the criteria for the diagnosis of diabetes recommended by the American Diabetes Association [12]. However, the guidelines propose that for prediabetes testing, FPG, 2 h-PG, OGTT and A1C are equally appropriate. We recruited only HIV- infected patients who received HAART with an undetectable plasma viral load. Thus, the results from this present study might not be applicable only to the HAART-na�ve HIV- infected population not to the HIV-infected patients without successful ART. So the prevalence of prediabetes varies between different ethnic groups, culture and epidemics, the results may not be implied for non-Asian HIV infected populations.
Conclusion
Co-infections frequently observed in people living with HIV also significantly influence the age and positive family history of diabetics. In HIV patients major implications for treatment are the avoidance of PI- based regimens at high risk of developing diabetes, and the careful choice, observation and close monitoring of antidiabetic medications in HIV-infected people in relation with potential comorbidities and drug interactions.
Recommendation
PI-based regimes should be avoided in HIV infected patients at high risk of developing diabetes, e.g., especially those with a history of gestational diabetes, a positive family history of diabetes, or impaired glucose tolerance on screening. Regime should be avoided, and replaced with less toxic drugs.
Acknowledgement
The authors would like to acknowledge all patients who participated in the research.
CONFLICT OF INTEREST
Authors declare no conflict of interest.
References
- World Health Organization. Global health sector strategy on HIV 2016-2021. Towards ending AIDS. World Health Organization; 2016.
- Phuphuakrat A, Nimitphong H, Reutrakul S, et al. Prediabetes among HIV-infected individuals receiving antiretroviral therapy: Prevalence, diagnostic tests, and associated factors. AIDS Res Ther 2020; 17:1-8.
- Noubissi EC, Katte JC, Sobngwi E. Diabetes and HIV. Current Diabetes Rep 2018; 18:1-8.
- UNAIDS. Fact Sheet 2021 global hiv statistics. End AIDS epidemic. 2021; 1–3.
- Rasool M, Malik A, Khan KM, et al. Time dependent changes in circulating biomarkers during diabetic pregnancies: A Perspective case study. Life Sci J 2014; 11.
- McMahon CN, Petoumenos K, Hesse K, et al. High rates of incident diabetes and prediabetes are evident in men with treated HIV followed for 11 years. Aids 2018; 32:451-9.
- Arafath S, Campbell T, Yusuff J, et al. Prevalence of and risk factors for prediabetes in patients infected with HIV. Diabetes Spectrum 2018; 31:139-43.
- Tripathi A, Liese AD, Jerrell JM, et al. Incidence of diabetes mellitus in a population‐based cohort of HIV‐infected and non‐HIV‐infected persons: the impact of clinical and therapeutic factors over time. Diabetic Med 2014; 31:1185-93.
- Stephane De Wit MD, Worm MD, Reiss P, et al. Incidence and risk factors for new-onset diabetes in HIV-infected patients. Diabetes Care 2008; 31:1224-9.
- Liu J, Wang G, Jia Y, et al. Physical exercise as therapy for type II diabetes. Diab. Metab Res Rev 2014; 32:13-23.
- Care M. Pharmacologic approaches to glycemic treatment: Standards of medical care in diabetesd―2020. Diabetes Care 2020; 43:98–110.
- Yokoyama BY, Chehter EZ. Diabetes and HIV: What do we know? 2021; 22:77–82.
- Freedman RB. Membrane-bound enzymes. In New Comprehensive Biochemistry 1981; 1:161-214.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Saba Iqbal1*, Naheed Akhter2, Haseeb Mukhtar3, Hina Sadaf4, Sayed Asif Jahanzeb Kazmi5 and Zobiah Hafeez6
1Department of Health Professions Education, CMH & IOD Lahore, Pakistan2Department of Medicine, CMH institute of Medical Sciences, Bahawalpur, Pakistan
3CMH and IOD Lahore, Pakistan
4Department of Physiology, Azra Naheed Medical College, Pakistan
5Department of Pharmacology, CMH institute of Medical Sciences, Bahawalpur, Pakistan
6Department of Physiology, UCMD, UOL, Pakistan
Received: 14-Dec-2022, Manuscript No. Jrmds-21-47803; , Pre QC No. Jrmds-21-47803 (PQ); Editor assigned: 16-Dec-2021, Pre QC No. Jrmds-21-47803 (PQ); Reviewed: 30-Dec-2021, QC No. Jrmds-21-47803; Revised: 04-Jan-2022, Manuscript No. Jrmds-21-47803 (R); Published: 11-Jan-2022
