Review - (2023) Volume 11, Issue 1
Review Article on obesity as a contributor to Type-2 Diabetes Mellitus among adolescents
Bhavya Rajeshwari and Guddi Laishram*
*Correspondence: Guddi Laishram, Department of Community Medicine, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences, India, Email:
Abstract
Worldwide, the incidence of obesity causing the incidence of diabetes has been increasing in young adults. This has resulted in an epidemic of diabetes among the young in several countries, which earlier used to be just a disease more common in adults around 30-40 years of age or beyond. Adolescents nowadays are not involved in any outdoor activities or sports, are eating more junk foods rather than healthy and fibrous foods, spending more time on gadgets, sitting in one place, there is no movement at all, and are experiencing more psychological disturbances because of stress, pressure from peers and parents. In obesity, there is an increase in fat deposition in the body which is directly linked with an increase in insulin resistance, which is one of the causative factor of Type II diabetes Mellitus. Another reason which also causes obesity induced Type II Diabetes Mellitus is disturbance in beta-cell function of the pancreas. This issue has become one of the most severe problems worldwide and is also one of the issues which can be easily controlled just by spreading awareness, making people realise the importance of prevention and motivating them to actively act against it. Weight loss is one of the major steps in curbing the initiation of diabetes mellitus in young adults. One of the most important reasons for preventing this is that during adolescence, usually obesity induced diabetes remains asymptomatic, but as they grow in age, there is an increase in the chances of getting severe symptoms as well as an increase in the chance of complications and acquiring severe diseases.
Keywords
Obesity, Type II diabetes mellitus, Adolescents, Fat deposition, Insulin resistance
Introduction
Increase in body weight which occurs due to abnormal growth of fat in the body can be termed as obesity. The abnormal growth either from increased size of the fat cell or number of the fat cell or both [1]. In obesity, there is an increase in weight and Body Mass Index (BMI). When BMI is more than 30 kilogram per meter cube, the person is considered obese [2].
Body mass index is basically Weight-for-Height measurement, which is frequently used to define humans as Underweight, Overweight, or Obese [1].
Increased blood sugar can be characteristic of a condition called Diabetes mellitus. It is mainly of two types:
Type 1 Diabetes Mellitus,
Type 2 Diabetes Mellitus [3].
In Type I Diabetes Mellitus (DM), we can observe a decrease in the amount of insulin along with the loss of beta-pancreatic cells. It is mainly an autoimmune disorder. In Type II Diabetes Mellitus mainly, there is insulin resistance and an insufficient response of betapancreatic cells [3]. Type II Diabetes mellitus was earlier considered to be a predominantly adult disease with the target age group being the elderly and middle age. Diabetes onset after the age of 30 or 40 years has been utilized to differentiate between both the subtypes of diabetes in both clinically as well as research studies. However, recent times have noted an upward slope in the prevalence of Type II DM in adolescents [4]. This has become more and more common in recent decades due to sedentary lifestyle and unhealthy foods.
Obesity has been one of the commonest reasons for increased risk of Type II Diabetes in adolescents but not all of them who are obese will acquire Type II Diabetes Mellitus.
Objective
By writing this review article, we aim to obtain information related to obesity as a contributor to the development of Type II diabetes mellitus, especially in adolescents.
Methodology
NCBI, Public health med search, and the American Diabetes Association were used to examine as well as review previously published literature. This paper was also reviewed using Textbooks of preventive and social medicine as well as that of pathology. Type II diabetes mellitus, adolescents, obesity, and other mesh words were used to search the numerous sources. We were able to mention the further conclusion after consulting the relevant articles and other resources.
Incidence
There have been numerous reports indicating a major increase in incidence of obesity induced Type II diabetes mellitus in adolescents worldwide in past few decades. It has become an epidemic in few countries for example, India and U.S.A.
According to recent estimates from the National Health and Nutrition Examination Survey, over one-third of children in the United States are overweight or obese, with around 17% reaching obesity standards [5].
If the body mass index is found to be present in the range of the 85th and 95th percentiles, this implies that the individual may become overweight in future. However, if the BMI exceeds the 95th percentile, it will be classified as overweight (Figure 1) [6].
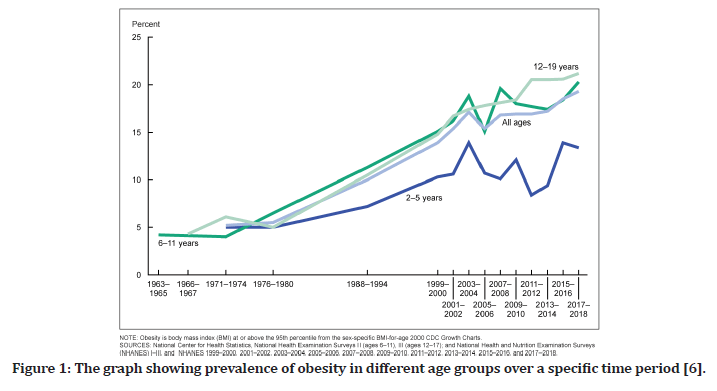
Figure 1. The graph showing prevalence of obesity in different age groups over a specific time period [6].
In USA, the overweight rates in adolescents between age 12-19 year olds are approximately 15.5% [6].
In the United States, roughly 12.7 million children and teenagers are obese [7].
Few cases are also being noted in United Kingdom. As noted by eminent Dr Abbas Ali, an overwhelming number of cases of diabetes have been noted in children and young adults since the beginning of 1990s, as the rate of obesity has increased fast [8]. He also stated that obesity increases the rate of diabetes in these young adults by 4 times [8].
According to the International Diabetes Federation [IDF], diabetes affects 1.1 million children and adolescents aged 14 to 19. In India, the proportion of pre-diabetes and diabetes was 12.3% and 8.4%, among young adults accordingly [7]. BMI and sub-scapular skin-fold thickness are two crucial indicators of diabetes mellitus as well as prediabetes in teenagers. It is more common in young obese girl than young boy [7].
Etiology [9]
The etiology included in causation of diabetes includes 2 factors and they are:
Modifiable factors: These are the variables that can be changed. They are mainly environmental in nature and include aspects of nutrition and lifestyle.
Non-modifiable factors: These are inherently irreversible and are primarily present from birth.
Non-modifiable factors
This contains three significant factors that are the primary causes of Type 2 Diabetes Mellitus. Intrauterine exposure, family history, and ethnicity are those three aspects.
Intrauterine exposure is the most prominent of these three attributes.
Modifiable factors
These factors are usually the ones which can easily be controlled by humans. An individual's lifestyle is a selfsufficient component that can be changed by the persons themselves.
Out of all the most important is Obesity and overweight.
Obesity is linked as it causes rise in the resistance to insulin which inadvertently causes increased concentration of free fatty. The increase in free fatty acids acts as a promoter of lipolytic activity, which is also an important factor in contributing to diabetes mellitus.
PCOS (polycystic ovarian syndrome) also acts as a contributor to type II DM in adolescent girls.
Obesity is commonly related with PCOS. It's an endocrine condition linked to poor reproductive health. It's also linked to insulin resistance, regardless of fat [10].
Pathophysiology
The most common factor causing type II diabetes in adolescents is obesity.
The clear pathogenesis of this is not very known.
The pathology involved in occurrence of type II diabetes is intricate and consists of range of risk factors like genetic and environmental. These are vital in causing malfunctioning of beta cells along with increased hepatic and muscular insulin resistance [11].
Early onset of type II diabetes appears to contribute to a heightened risk of illness and death rates during life's peak years [11,12].
In ideal conditions, there is a state of equilibrium between the amount of insulin secreted by pancreatic cells and the sensitivity of various body organs and tissues to insulin [13].
A decrease in sensitivity to insulin must be counteracted by equal increase in secretion for maintaining ideal glucose tolerance. In majority of the teenagers, obesity results in reduction in insulin sensitivity due to which insulin is secreted in higher amounts for compensation [13].
In comparison to non-obese young adults, obese adolescents have approximately 40% lesser amount of insulin-stimulated glucose metabolism and as a result they are usually hyper insulin emic (Figure 2) [14].
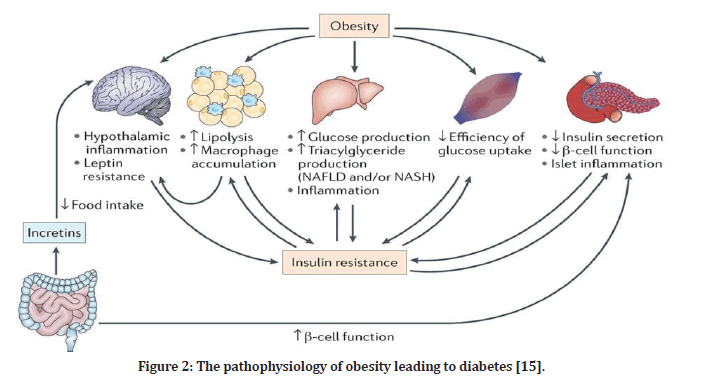
Figure 2. The pathophysiology of obesity leading to diabetes [15].
The Mechanisms involved in these are:
Inflammation
This is one of the crucial components of the obesitydiabetes connection. Obesity-related chronic lowgrade inflammation promotes and anticipates diabetes, according to many studies [16].
The most frequent and significant inflammatory marker seen in obese children which induces diabetes is C-reactive proteins (CRP) [16].
Another inflammatory marker which also shows a connection is Adiponectin. This is mainly related to insulin resistance and inflammation [16].
In a study conducted in North India focusing on participants in the age group of 14 to 25 years, CRP levels were found to be elevated in about 21.8% of subjects who were overweight and 24.5% of the subjects who had a high percentage of body fat [17].
Insulin resistance
This is closely linked to obesity and is also thought to be a vital precursor of DMII [18].
Fasting hyperinsulinemia, a predictive sign of insulin resistance, was seen in 64 percent of obese teenagers in India aged 14–19 years [19].
Early detection of insulin resistance can help prevent type II diabetes association with obesity.
Some points to be noted about insulin resistance in obese individuals:
It should be taken into consideration that adipose tissue that proliferates in the obese state, synthesises and secretes certain metabolites as well as signalling proteins. Some of these include Tumour Necrosis Factor (TNF-α), Leptin, and Visfatin. These metabolites change insulin secretion and also lead to insulin resistance [14].
Insulin resistance is linked to a high BMI and pubertal hormones, as well as improper fat fragmentation, high Free Fatty Acids, Mitochondrial dysfunction, and Inflammation [20].
When the pancreas can't keep up with the increased insulin demands caused by insulin resistance, hyperglycaemia and Type II Diabetes Mellitus develop [20].
Metabolic syndrome
This is viewed as a collection of symptoms that include intolerance to glucose, hypertension, abnormally elevated lipid level, and central obesity along with insulin resistance [21].
Obese children have an increased risk of acquiring metabolic syndrome [22].
Though it is very commonly seen in obese adolescents, its role as a contributor to Type II Diabetes has not yet been established [18].
Body fat distribution plays an important role in pathogenesis of diabetes and the reasons for the same have been explained as follows:
Insulin resistance has been linked to a change in fat distribution between the subcutaneous and visceral locations [23].
In obese adults, if fat is present in greater amount in visceral locations, then there is a greater correlation with insulin sensitivity than it is with subcutaneous fat distribution [24].
Insulin resistance in obese individuals is caused by ectopic fat deposition in the muscles and liver, as fat accumulation in these areas inhibits insulin signaling. Therefore, there is reduced uptake of glucose in the muscle and consequently decline in the insulin mediated inhibition of glucose synthesis in liver [23].
Even in the absence of obesity fat accumulation in the liver is associated with insulin resistance [25,26].
It has recently been proposed that fat deposits around arteries can trigger an endocrine action which in turn will increase the development of resistance to insulin [27].
Clinical features
The gold standard for diabetes assessment in youngsters is:
Presence of the hallmark symptoms of diabetes mellitus like increase in urination (polyuria), increased thirst (polydipsia) and weight loss which could not be explained. Additionally concentration of glucose over 200 or equivalent to 200mg/dl in venous or capillary blood sample is considered [28].
Upon performing fasting glucose test, glucose concentration of greater or equal to 126mg/dl is categorized as DM [28].
When considering the oral glucose tolerance test (GTT), any value greater than or equal to 200mg/dl is classified as DM [28].
These requirements should be confirmed on a subsequent day by repeating the tests if there is no obvious hyperglycaemia with acute metabolic decompensation [28].
The symptoms of diabetes in adolescents can be classified on the basis of whether it is acute or chronic. When the diabetes is acute in young adults, it presents with glycosuria with no ketone bodies in the urine, either polyuria is not present or is less in amount and there is very little or no weight loss. When the diabetes is in chronic form, It presents with immoderate weight loss, glucose in urine along with ketone bodies and excessive urination [28].
Usually the child will not show presence of any symptoms, so the diagnosis is done by screening or routine checkups in which blood test and urine examination is done to check glucose.
During adolescence, as it is mainly asymptomatic the severity of the disease is less, as the child gets older the severity and incidence of the disease increases.
Complications
The complications that can be seen in obesity induced Type II Diabetes in adolescents are:
Cardiac problems are among the most widely known consequences associated with Diabetes Mellitus Type II. Important cardiac modifications include Cardiomyocyte metabolism changes, changes in insulin signalling in the heart, overall calcium management, and the initiation of fibrosis in cardiac muscle were all interpreted within the context as important cardiac modifications [29].
Other well-known cardiac pathology consequences include hyperlipidaemia, coronary artery disease, hypertension, and diabetic cardiomyopathy as a result of these difficulties [30,31].
Certain sequalae, like Chronic Kidney Disease (CKD), can affect the renal function [32]. In this, there is inadequate blood flow which occurs primarily as a result of excessive solute [glucose] in the blood which is also known Hyperglycaemia. This leads to mesangial cell impairment and prevents the kidney from functioning properly [33].
As there is an obstruction in the functioning, albumin is present in the urine [34].
Some other complications that can be noted is Peripheral neuropathy [33].
Treatment [35]
There are three types of treatment interventions:
Weight control through changes in nutrition and lifestyle
Treatment of Diabetes mellitus include an integration of the various therapies including the presence of various health care providers like a general physician, nurse specialised in diabetic care, nutritionist, fitness instructor along with the help of psychologists and social worker as and when necessary [36].
Family participation is necessary for initiating and maintaining the necessary lifestyle modifications for handling this condition [37].
Exercise induces two mechanisms, the first one is enhancement of glucose uptake while the second is an increase in glycogen synthesis. It also addresses livers insulin resistance [35].
Hypoglycaemic agents
These promote insulin production, increase the effectiveness of metabolic action of insulin, reduce the amount of glucose which is being produced by the liver, decrease food absorption or sensitise tissue to insulin, can all be employed to lower the glucose level in blood [38].
Agents which are given orally includes biguanides like metformin, sulfonylureas, AGIs etc [38].
Biguanides like metformin improve peripheral insulin sensitivity while lowering hepatic glucose production. They also help you lose weight and enhance your lipid profile [38].
Sulfonylureas boost insulin secretion by increasing the reactivity of pancreatic cells to glycaemic stimuli [35,39].
AGIs known as alpha-glucosidase inhibitor like acarbose are. Complex oligosaccharide that slow the breakdown of carbohydrates. The main impact of these supplements are to decrease post meal glucose reflex [35,40].
Insulin therapy
This is given when there is no improvement on medication. It is given in the form of injections.
Consequences
There can be a lot of reasons due to which obesity in adolescents can act as a etiological factor of Type II Diabetes Mellitus. Some of the more common reasons include, but are not limited to, sedentary lifestyle, unhealthy food, decreased outdoor activities, and increased screen time due to the recent development of technologies [41-43].
There are also psychological disturbances which can lead to an increase in obesity in adolescents. For example, when there is an overweight child and he/she goes to school, they are teased or bullied about their weight. This leads to lowered self-esteem, lack of selfworth, stress, fearfulness, and lack of confidence. This will subsequently cause them to eat more and more unhealthy foods like cakes, chocolates, etc., leading to an increase in weight. These children also don’t go to work out or play sports or involve themselves in any outdoor activities due to the fear of being judged by their peers. Lack of friends is another problem faced by such children [44-46].
Psychological factors can lead to emotional disturbances and eating disorders. This can also occur due to academic pressure, pressure from parents, and pressure from peers and friends. In teenagers nowadays, there is also a lack of self-esteem because of constant body shaming and also, teenagers are not satisfied with the way they look.
Conclusion
From the studies conducted on obese adolescents it can be concluded that obesity is a primary contributing factor to the incidence of Type II diabetes. In this type of situation, we should try to spread more awareness among the community. Some of the measures which can be adopted include telling parents about the importance of sports and physical exercise. Children should be encouraged to partake in physical activities and positive reinforcements or incentives can be provided for the accomplishment of set goals. Healthy food eating habits can be inculcated Rather than pressurising children, parents and friends should be supportive. We can also promote the introduction of health education with the aim of teaching children about the importance of sports, good eating habits, and the importance of not ragging or shaming anyone.
The most important thing is to spread awareness because both of these conditions are also accompanied simultaneously by lots of serious complications. As obesity induced Type II diabetes is becoming an epidemic in some countries, preventing it is of prime importance to take effective measures to do the same.
References
- Park K. Parks Textbook of preventive in social medicine. 25th ed. Jabalpur: Banarsidas Bhanot Publishers 1994.
- Badhwar R, Kaur G, Popli H, et al. Pathophysiology of obesity-related non-communicable chronic diseases and advancements in preventive strategies. 2020; 25:317-340.
- Kumar A, Abbas AK, Jon C. Aster: Robbins and cotran pathologic basis of disease. Professional Edition 2015.
- Shaw J. Epidemiology of childhood type 2 diabetes and obesity. Pediatr Diabetes 2007; 8:15.
- Ogden CL, Carroll MD, Curtin LR, et al. Prevalence of high body mass index in US children and adolescents, 2007-2008. JAMA 2010; 303:242-249.
- Fryar CD, Carroll MD, Afful J. Prevalence of overweight, obesity, and severe obesity among adults aged 20 and over: United States, 1960–1962 through 2017–2018. NCHS 2020; 10.
- https://www.endocrine.org/news-and-advocacy/news-room/2017/childhood-obesity-quadruples-risk-of-developing-type-2-diabetes
- Xue Y, Gao M, Gao Y. Childhood type 2 diabetes: Risks and complications. Exp Ther Med 2016; 12:2367-2370.
- Calcaterra V, Verduci E, Cena H, et al. Polycystic ovary syndrome in insulin-resistant adolescents with obesity: The role of nutrition therapy and food supplements as a strategy to protect fertility. Nutr 2021; 13:1848.
- DeFronzo RA. From the triumvirate to the ominous octet: a new paradigm for the treatment of type 2 diabetes mellitus. Diabetes 2009; 58:773-795.
- D’adamo E, Caprio S. Type 2 diabetes in youth: Epidemiology and pathophysiology. Diabetes Care 2011; 34:S161-S165.
- Pinhas-Hamiel O, Zeitler P. Acute and chronic complications of type 2 diabetes mellitus in children and adolescents. Lancet 2007; 369:1823-1831.
- Kumar P, Srivastava S, Mishra PS, et al. Prevalence of pre-diabetes/type 2 diabetes among adolescents (10–19 years) and its association with different measures of overweight/obesity in India: A gendered perspective. BMC Endocr Disord 2021; 21:1-2.
- Arslanian S, Bacha F, Grey M, et al. Evaluation and management of youth-onset type 2 diabetes: A position statement by the American Diabetes Association. Diabetes care 2018; 41:2648-2668.
- https://u.osu.edu/diabetes2018/patho/
- Duncan BB, Schmidt MI. The epidemiology of low-grade chronic systemic inflammation and type 2 diabetes. Diabetes Technol Ther 2006; 8:7-17.
- Vikram NK, Misra A, Dwivedi M, et al. Correlations of C-reactive protein levels with anthropometric profile, percentage of body fat and lipids in healthy adolescents and young adults in urban North India. Atherosclerosis 2003; 168:305-313.
- Praveen PA, Tandon N. Childhood obesity and type 2 diabetes in India. WHO-SEAJPH 2016; 5:17-21.
- Vikram NK, Misra A, Pandey RM, et al.Heterogeneous phenotypes of insulin resistance and its implications for defining metabolic syndrome in Asian Indian adolescents. Atherosclerosis 2006; 186:193-199.
- Cree-Green M, Triolo TM, Nadeau KJ. Etiology of insulin resistance in youth with type 2 diabetes. Curr Diabetes Rep 2013; 13:81-88.
- Huang PL. A comprehensive definition for metabolic syndrome. Dis Model Mech 2009; 2:231-237.
- Jessup A, Harrell JS. The metabolic syndrome: Look for it in children and adolescents, too. J Diabetes Res 2005; 23:26-32.
- Weiss R, Kaufman FR. Metabolic complications of childhood obesity: identifying and mitigating the risk. Diabetes care 2008; 31:S310-316.
- Caprio SO, Hyman LD, Limb CH, et al. Central adiposity and its metabolic correlates in obese adolescent girls. Am J Physiol Endocrinol Metab 1995; 269:E118-126.
- Tiikkainen M, Tamminen M, Häkkinen AM, et al. Liver‐fat accumulation and insulin resistance in obese women with previous gestational diabetes. Obesity Res 2002; 10:859-867.
- Kelley DE, McKolanis TM, Hegazi RA, et al. Fatty liver in type 2 diabetes mellitus: Relation to regional adiposity, fatty acids, and insulin resistance. Am J Physiol Endocrinol Metab 2003; 285:E906-916.
- Yudkin JS, Eringa E, Stehouwer CD. “Vasocrine” signalling from perivascular fat: A mechanism linking insulin resistance to vascular disease. Lancet 2005; 365:1817-1820.
- Reinehr T. Clinical presentation of type 2 diabetes mellitus in children and adolescents. Int J Obes 2005; 29:S105-110.
- Mandavia CH, Aroor AR, DeMarco VG, et al. Molecular and metabolic mechanisms of cardiac dysfunction in diabetes. Life Sci 2013; 92:601-608.
- Vinicor F, Jack Jr L. 25 years and counting: Centers for disease control and prevention identifies opportunities and challenges for diabetes prevention and control. Ann Intern Med 2004; 140:943-944.
- Jørgenrud B, Jalanko M, Heliö T, et al. The metabolome in finnish carriers of the MYBPC3-Q1061X mutation for hypertrophic cardiomyopathy. PLoS One 2015; 10:e0134184.
- Min TZ, Stephens MW, Kumar P, et al. Renal complications of diabetes. Br Med Bull 2012; 104:113-127.
- Xue Y, Gao M, Gao Y. Childhood type 2 diabetes: Risks and complications. Exp Ther Med 2016; 12:2367-2370.
- Porth C. Essentials of pathophysiology: Concepts of altered health states. LWW 2011.
- Schwartz MS, Chadha A. Type 2 diabetes mellitus in childhood: Obesity and insulin resistance. Int J Osteopath Med 2008; 108:518-524.
- Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993; 329:977-986.
- Anderson BJ. Diabetes self-care: Lessons from research on the family and broader contexts. Curr Diabetes Rep 2003; 3:134-140.
- Krentz AJ, Bailey CJ. Oral antidiabetic agents. Drugs 2005; 65:385-411.
- Aguilar-Bryan L, Nichols CG, Wechsler SW, et al. Cloning of the β cell high-affinity sulfonylurea receptor: A regulator of insulin secretion. Science 1995; 268:423-426.
- Van De Laar FA, Lucassen PL, Akkermans RP, et al. α-Glucosidase inhibitors for patients with type 2 diabetes: Results from a cochrane systematic review and meta-analysis. Diabetes care 2005; 28:154-163.
- Garg M, Mohale S. Prevalence of Metabolic Obesity Normal Weight (MONW) in cardiovascular disease patients--A hospital-based case control study. J Evol Med Dent Sci 2020; 9:2427-2432.
- Hulkoti VS, Acharya S, Shukla S, et al. In search of an ideal obesity assessment tool: Is body mass index reliable enough. J Evol Med Dent Sci 2020; 9:2556-2560.
- Rasheed A, Acharya S, Shukla S, et al. High-sensitivity C-reactive protein in metabolic healthy obesity (MHO). J Evol Med Dent Sci 2020; 9:443-447.
- Inamdar SA, Agarwal H, Acharya S, et al. Coexistence of hypertriglyceredemia and hypercholesterolemia with gestational diabetes mellitus in pregnancy: A case report. Med Sci 2020; 24:594-598.
- Jankar JS, Harley KN, Mohod KM, et al. Association of urinary albumin with HbA1c levels in subjects of Type 2 diabetes mellitus in central India. J Evol Med Dent Sci 2020; 9:3921-3925.
- Unnikrishnan B, Singh A, Rathi P, et al. Risk factors of gestational diabetes mellitus: A hospital-based pairmatched case-control study in coastal South India. S Afr J Obstet Gynaecol 2020; 26:13-17.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Bhavya Rajeshwari and Guddi Laishram*
Department of Community Medicine, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences, Wardha, IndiaReceived: 02-Dec-2022, Manuscript No. JRMDS-22-85225; , Pre QC No. JRMDS-22-85225(PQ); Editor assigned: 05-Dec-2022, Pre QC No. JRMDS-22-85225(PQ); Reviewed: 20-Dec-2022, QC No. JRMDS-22-85225 (QC); Revised: 27-Dec-2022, Manuscript No. JRMDS-22-85225(R); Published: 03-Jan-2023
