Research - (2022) Volume 10, Issue 2
Smoking Causes Obstructive Changes in Routine Spirometry
Muhammad Ali1*, Ruqaya Nangrejo1, Saba Abrar1, Adnan Anwar2, Asma Bilquis1 and Qamer Aziz1
*Correspondence: Muhammad Ali, Department of Physiology, Baqai Medical University, Pakistan, Email:
Abstract
Objective: Chronic obstructive lung diseases are caused by Smoking. Therefore, the objective of this study was to assess the obstructive changes of lungs in spirometry caused by smoking. Methodology: This was a case control study conducted at Ghazi goth, more than 5 kms from New Subzi mandi (case area) by using non probability convenient sampling technique. The duration of study was about 6 months from August 2019 till Jan 2020. Sample size was 245. 100 subjects were residents of ghazi goth taken with age, socioeconomic strata & BMI while the 145 workers belong to vegetable market new Subzi mandi Karachi (case group). Males with age of 18 to 60 years, Residents of area more than 5 km away from vegetable market were included in the study. Three pulmonary function parameters such as FEV1, FVC and FEV1/FVC were evaluated in routine Spirometry. Chi square and independent t-test was applied. Results: The study results showed that baseline characteristics between both groups has insignificant association i.e. age, weight, BMI, hours of working & duration since working. While height has significant association, the workers of vegetable market were taller. Control group indulge more in smoking (53.77 ± 6.14) than case group (36.68 ± 3.42) (pack years of smoking has significant association (p<0.05). Mean of FEV1 (Forced expiratory volume in first second) found subnormal in this group (75 ± 25.8). Mean of FVC% (forced vital capacity) significantly reduced (p=0.000) in control group (90 ± 36.1) as compared to case group 122.4 ± 74.7. Conclusion: This study concluded that smoking is associated with obstructive changes in lung in routine spirometry. Furthermore, predicted forced vital capacity was significantly reduced in control group than case group owing to smoking was more indulge in control group.
Keywords
Body mass index, Chronic obstructive pulmonary disease, Spirometry, Predicted forced vital capacity
Introduction
Smoking is a public wellbeing dilemma that leads to develop a variety of disorders. About 1.2 billion populace smoke globally [1-3]. In the European Union, 700,000 deaths are caused by the smoking annually [1]. Disorders that are directly related to smoking involve respiratory, oncological, cardiovascular, and cerebrovascular critical situations [4,5]. Most extensively affected system by smoking is the human respiratory system wherein infection rapidly transmit from the smaller to the bigger airways. Moreover, Smoking is a prognostic factor for hyper responsiveness of bronchus, chronic obstructive pulmonary disease (COPD), asthma, and lung cancer [6]. In the United States, smoking is liable to develop chronic airway disease in 80% of cases [7]. Smoking also causes neutrophilia [8].
In order to evaluate the lung functions, Spirometry is the most generally used which is an easy and fast procedure. Routine spirometry measures Forced expiratory volume in first second (FEV1), Forced vital capacity (FVC), and the ratio of the two volumes (FEV1/FVC) [9]. Spirometry and the measurement of FEV1/FVC permit the recognition of restrictive or obstructive ventilator disorders. A FEV1/FVC less than 70 % in which FEV1 is decreased over FVC suggests an obstructive disorder for instance asthma and chronic obstructive pulmonary disease (COPD). The FEV1 might be reported as a proportion of the prognostic value that indicates the acuteness of the impairment. A FEV1/FVC more than 70% in which FEV1 is decreased over FVC indicates restrictive disorder for instance interstitial lung diseases (such as idiopathic pulmonary fibrosis) and chest wall malformations [10].
If spirometry indicates signs of impediment in airways as established due to reduction in forced expiratory volume in first second (FEV1) or FEV1/forced vital capacity (FVC), the findings reveal a decline in lung function [11].
One prospective, cross-sectional study by Dugral and Balkanci in which Spirometry was used to assess lung function; they measured the forced expiratory volume per second (FEV1), the forced vital capacity (FVC), and the FEV1/FVC ratio. They demonstrated that smokers reported considerably more breathlessness and production of sputum as compared to non-smokers, although revealed improved FVC and FEV1 rates. Persons who smoked not as much had notably poorer FVC and FEV1 rates as compared to non-smokers. Furthermore, smokers showed considerably lesser FEV1/FVC ratios in comparison with non-smokers [12]. Earlier studies performed by Nawafleh et al. [13] and by Lorensia et al. [14] observed that lung function (FEV1/FVC) were varied among smokers and non-smokers. Smoking decrease diffusing capacity & current smokers & people with COPD have an increased risk of severe complications & higher mortality with COVID-19 infection [15].
Smoking causes inactivation of an important enzyme alpha 1 antitrypsin which decrease the activity of proteases hence proteases spatially elastase become active & start damaging lungs & causes emphysema. Smoking also increases the risk of tuberculosis, certain eye diseases, problems of immune system & rheumatoid arthritis. Nicotine patch can be used as an alternative of smoking. Herbal cigarettes can give an advantage that doesn’t contain nicotine [16].
Termination of Smoking is the only most successful remedy for COPD. Additionally, smoking cessation reduces the chances of coronary heart disease, stroke, many types of cancer, and it is also related to an increased expectancy of life [17]. Regardless of the continuing inflammatory process, it is evidently supported that that the speed of progression of COPD can be decreased with the cessation of smoking [18]. The initial suggestion reported from longitudinal cohort researches that persons who smoke continuously had a much steeper decline in pulmonary function than those persons who had quit smoking [19].
There is an inadequate data in Pakistan to assess the obstructive changes caused by smoking on routinely performed Spirometry. Therefore, this study was conducted to assess the obstructive and restrictive changes due to smoking on regular Spirometry.
Methodology
This was a case control study conducted at Ghazi goth, more than 5 kms from New Subzi mandi by using non probability convenient sampling technique. The duration of study was about 6 months from August 2019 till Jan 2020. Sample size was 245 that were calculated using Statistical formula. 100 subjects were residents of ghazi goth (control group) taken with age, socioeconomic strata & BMI while the 145 workers belong to vegetable market new Subzi mandi Karachi (case group). Males with age of 18 to 60 years, Residents of area more than 5 km away from vegetable market were included in the study whereas females and known case of respiratory (asthma, COPD) or cardiovascular disease were excluded from the study.
After ethical approval and informed consent from cases and controls, Data was collected; Height & weight measured by measuring tape & digital weighing machine. Data consisted of cases & control history of profession, respiratory symptoms and past medical history, history of pack years of smoking. Two groups were formed on the basis of history of pack years. Pack years are defined as packets of cigarette consumed per day multiplied by years since smoking. 1 pack contains 20 cigarettes. For spirometry, electronic digital portable spirometer was used to measure 3 regular parameters. These were forced expiratory volume in 1st second (FEV1%), forced vital capacity (FVC%) and FEV1/FVC% calculated. Spirometry interprets obstructive (Limitation of expiratory airflow) and restrictive (Decrease lung volumes) patterns of lungs based on ATS/ERS Criteria. Decreased FEV1, (Normal or Decrease) FVC, Decreased FEV1/FVC indicated obstructive pattern whereas Decreased FEV1, Decrease FVC, Normal to Increased FEV1/FVC indicated restrictive (fibrosis) pattern.
For analysis of data, SPSS version 23.0 was used. Qualitative data was represented as frequency and percentages while quantitative data was presented as mean and standard deviation. To test for association inbetween cases and controls, Pearson Chi-square test was applied on qualitative data whilst on quantitative data, independent sample t-test was applied. p-value of <0.05 was considered as statistically significant.
Results
A total of 245 subjects were separated into two groups, 100 individuals in control group and 145 individuals were in case group. With respect to age categories in control group, 42(42%) subject lies in 18-26 years of age, 23(23%) lies in 27-35 years, 15(15%) lies in 36-44 years and 20(20%) lies in >44 years of age. In case group, 61(42.1%) subject lies in 18-26 years of age, 30(20.7%) lies in 27-35 years, 33(22.8%) lies in 36-44 years and 21(14.5%) lies in >44 years of age with an insignificant association between all age categories in case and control group. As far as BMI is concerned in control group, 16(16%) had ≤ 19.9, 40(40%) had 20 - 24.9, 21(21%) had 25 - 29.9, 23(23%) had ≥ 30 whereas in case group 16(11%) had ≤ 19.9, 53(36.6%) had 20-24.9, 53(36.6%) had 25-29.9, 23(15.9%) had ≥ 30, as shown in Table 1.
| Group | p-value | |||
|---|---|---|---|---|
| Control(n=100) | Case(n=145) | |||
| n(%) | n(%) | |||
| Age categories (Years) | 18-26 | 42(42%) | 61(42.1%) | 0.38 |
| 27-35 | 23(23%) | 30(20.7%) | ||
| 36-44 | 15(15%) | 33(22.8%) | ||
| >44 | 20(20%) | 21(14.5%) | ||
| Body Mass index (BMI) | ≤19.9 | 16 (16%) | 16(11%) | 0.054 |
| 20 – 24.9 | 40(40%) | 53(36.6%) | ||
| 25 – 29.9 | 21(21%) | 53(36.6%) | ||
| ≥30 | 23(23%) | 23(15.9%) | ||
| Pearson Chi Square test applied | ||||
| P<0.05 Significant | ||||
| P>0.05 Non-significant | ||||
Table 1: Age and body mass index categories in control & cases (n=245).
Mean ages and anthropometry revealed that there was an insignificant association (p=0.43) found in between ages of control (33.2 ± 14.3 years) and case group (31.9 ± 11.3 years). An insignificant association (p=0.17) observed in between weight of control (64.5 ± 14.1 kg) and case group (67.1 ± 15.0 kg). A significant association (p<0.001) was seen in between height of control (161.6 ± 6.1 cm) and case group (164.8 ± 6.4 cm). An insignificant association (p=0.82) observed in between BMI of control (25.2 ± 5.2 Kg/m2) and case group (25.0 ± 5.0 Kg/m2). History of smoking revealed that Pack years has significant association (p<0.001) between control 53.77 ± 6.14 and case group 36.68 ± 3.42 was observed
An insignificant association (p=0.16) observed in between duration of working and hours of daily working of control (10.1 ± 2.2 years) and case group (11.3 ± 8.4 years). An insignificant association (p=0.63) observed in between hours of daily working of control (12.0 ± 0.01 hrs.) and case group (12.0 ± 0.3 hrs.). Pulmonary function tests reported, Predicted FVC% has significant association (p<0.001) between control group=90 ± 36.1 and case group=122.4 ± 74.7. On the other hand, Predicted FVC1% has insignificant association (p=0.73) between control group=75 ± 25.8 and case group=76.5 ± 35.4. Predicted FEV1/FVC (%) has insignificant association (p=0.22) between control group=74.2 ± 39.1 and case group=80.6 ± 41.7, as shown in Table II and Figure 1.
| Parameters | Controls | Cases | p-value |
|---|---|---|---|
| Mean ± SD | Mean ± SD | ||
| Age (Years) | 33.2 ± 14.3 | 31.9 ± 11.3 | 0.43 |
| Weight (Kg) | 64.5 ± 14.1 | 67.1 ± 15.0 | 0.17 |
| Height (cm) | 161.6 ± 6.1 | 164.8 ± 6.4 | <0.001 |
| BMI (Kg/m2) | 25.2 ± 5.2 | 25.0 ± 5.0 | 0.82 |
| Smoking pack years | 53.77 ± 6.14 | 36.68 ± 3.42 | <0.001 |
| Duration of working (Years) | 10.1 ± 2.2 | 11.3 ± 8.4 | 0.16 |
| Hours of Daily working (Hours) | 12.0 ± 0.01 | 12.0 ± 0.3 | 0.63 |
| Predicted FEV1 (%) | 75 ± 25.8 | 76.5 ± 35.4 | 0.73 |
| Predicted FVC (%) | 90 ± 36.1 | 122.4 ± 74.7 | <0.001 |
| Predicted FEV1/FVC (%) | 74.2 ± 39.1 | 80.6 ± 41.7 | 0.22 |
| Independent sample t-test applied | |||
| P<0.05 Significant | |||
| P>0.05 Insignificant | |||
Table 2: Association of mean ages and anthropometry, comparison of duration and working hours and mean comparison of pulmonary parameters between cases and controls.
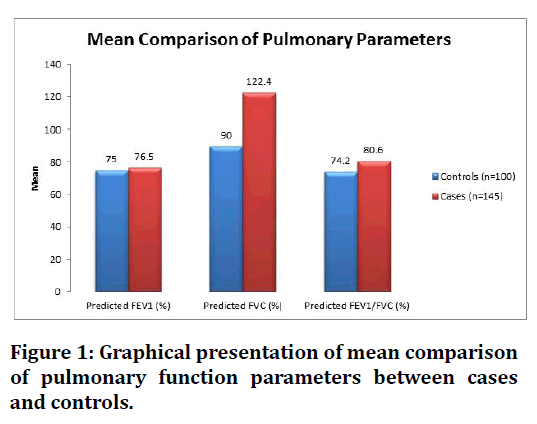
Figure 1. Graphical presentation of mean comparison of pulmonary function parameters between cases and controls.
Discussion
Pulmonary function is a marker of all-cause mortality/ morbidity; researches on the deleterious effect of smoking, particularly on adolescent, present valuable information. Smoking exhibits deleterious effects on human lungs ultimately symptoms develop [1]. Bronchial hyper responsiveness, chronic obstructive pulmonary disease, asthma, and lung cancer are attributed by the smoking [6].
Pulmonary functions are explored by FEV1, FVC, and FEV1/FVC parameters; both smoking and physical exercise effects on all 3 standards. One research by Twisk et al revealed that smoking reduced the FEV1 and FVC, whereas value of FVC increased by the physical activity [20]. Another study by Holmen et al reported that the FEV1 and FVC parameters were prognostic factors of improved lung function [21] Similarly, one research observed that smokers had improved FEV1 and FVC levels as compared to non-smokers, however those persons who smoked < half pack on a daily basis had worst FVC and FEV1 levels over non-smokers [12]. The present study showed that mean predicted FVC 90 ± 36.1 was seen in smokers of control group and 122.4 ± 74.7 in smokers of case group with a significant difference between them (p=0.000). It indicated that decreased Forced Vital Capacity (FVC) in control group reflecting obstructive lung disease.
Another research demonstrated that smokers had a substantially lesser FEV1/FVC ratio as compared to nonsmokers. Although, the smokers had better values of FVC and FEV1, the lesser FEV1/FVC ratio might be an indicator of obstructive lung disease. Value of FEV1 is more affected by smoking than the FVC values [12]. Likewise, they observed that the FEV1, FVC, and FEV1/FVC reported parameters were lesser that was 97.14, 89.78, and 94.51 respectively in those person who work out frequently as compared to those who did not exercise on a regular basis; Moreover, they reported significant differences in FEV1 and FVC (FEV1 P =0 .000; FVC P = 0.002) while insignificant difference seen in FEV1/FVC ratio [12]. Our study was consistent with the above reported study and showed that lower FEV1/FVC ratio observed in smokers of control group owing to excessive cigarette use that indicates obstructive lung disease. Furthermore, predicted FEV1, FVC, and FEV1/FVC values on the basis of daily working hours revealed that significant difference observed in FVC of case and control group (p=0.000) while insignificant differences seen in FEV1 and FEV1/FVC ratio (p=0.73, p=0.22) respectively reported in 12.0 ± 0.01 hours working daily in control group and 12.0 ± 0.3 hours in case group.
Further analysis performed by by Mhase et al. in 2002 evaluated the smoking effect on 115 people who were occupationally exposed to dirt and smoke by analyzing pulmonary function parameters. Indicators like FVC, FEV1, and FEV1/FVC ratio were documented. It was noticed that smokers were significantly highly affected by lung diseases and were associated with their smoking habits. The variation in parameters were observed such as FVC (p<0.001), FEV1 (p<0.001) and FEV1/FVC (p<0.001) signifying the mutual effect of fumes and dirt on the disease progression [22]. The present study was inconsistent with the above reported study and stated that pulmonary functions were associated with the smoking and dust particles of case and control groups. It was observed that predicted FVC was significantly associated (p=0.000) with smoking in control and case group whereas insignificantly association found in Predicted FEV1 (p=0.73) and Predicted FEV1/FVC (p=0.22) of case and control group.
In Indian study conducted by Bano et al. in the year of 2009 examined pulmonary function test on spirometry of 100 males that comprised of 50 smokers and 50 nonsmokers in a rural areas, stated that smoking is a frequent practice that is commonly seen in both rural and urban areas. It was reported that all the pulmonary function parameters significantly decreased in smokers, reflecting obstructive lung impairment. Furthermore, it was also found that lung function impairment was 17.3 times more in smokers than non-smokers [23]. The present study was in accordance with the above cited study and revealed that significant reduction observed in predicted FVC between case and control group (p=0.000) while insignificant reduction observed in Predicted FEV1 (p=0.73) and Predicted FEV1/FVC (p=0.22) of smokers in case and control group.
Briefly, there are different facts that timely judgment by using a variety of pulmonary function parameters can assist to recognize lung function impairment in symptomless smokers. Timely recognition with appropriate psychotherapy for smoking termination can stop expected morbidity and alleviate the chances of diseases related with the smoking behavior.
Conclusion
This study concluded that smoking is associated with obstructive changes in lung in routine spirometry. Furthermore, predicted Forced Vital Capacity was significantly reduced in control group than case group owing to smoking was more indulge in control group. Hence, timely pulmonary function tests should be carried out in smokers to find out decrease in lung volumes and termination of smoking should be persuaded, especially in Pakistan where most of the people smoking tobacco.
Conflict of Interest
None.
Acknowledgement
We acknowledge all participants from Ghazi Goth Karachi for their support throughout the study.
References
- Jayes L, Haslam PL, Gratziou CG, et al. Tobacco control committee of the european respiratory society. Smoke haz: Systematic reviews and meta-analyses of the effects of smoking on respiratory health. Chest 2016; 150:164-179.
- Polakowska M, Kaleta D, Piotrowski W, et al. Tobacco smoking in poland in the years from 2003 to 2014. Multicentre national population health examination survey (WOBASZ). Pol Arch Intern Med 2017; 127:91-99.
- Edwards R. The problem of tobacco smoking. Br Med J 2004; 328:217-219.
- Gomes R, Luís F, Tavares A, et al. Respiratory functional evaluation and pulmonary hyperinflation in asymptomatic smokers: Preliminary study. Rev Port Pneumol 2015; 21:126-131.
- Maritz GS, Mutemwa M. Tobacco smoking: Patterns, health consequences for adults, and the long-term health of the offspring. Glob J Health Sci 2012; 4:62-75.
- Juusela M, Pallasaho P, Rönmark E, et al. Dose-dependent association of smoking and bronchial hyperresponsiveness. Eur Respir J 2013; 42:1503-1512.
- Nye RT, Mercincavage M, Branstetter SA. Time to first cigarette, physical activity, and pulmonary function in middle-aged to older adult smokers. J Phys Act Health 2017; 14:612-616.
- Tommola M, Ilmarinen P, Tuomisto LE, et al. The effect of smoking on lung function: a clinical study of adult-onset asthma. Eur Respir J 2016; 48:1298-1306.
- Ranu H, Wilde M, Madden B. Pulmonary function tests. Ulster Med J 2011; 80:84-90.
- Fabbri L, Pauwels RA, Hurd SS, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary updated 2003.COPD 2004; 1:105-141.
- Westerdahl E, Engman KO, Arne M, et al. Spirometry to increase smoking cessation rate: A systematic review. Tob Induc Dis 2019; 17:31.
- Dugral E, Balkanci D. Effects of smoking and physical exercise on respiratory function test results in students of university: A cross-sectional study. Medicine 2019; 98:e16596.
- Nawafleh HA, Abo Zead SAS, Al-Maghairehc DF. Pulmonary function test: The value among smokers and nonsmokers. Health Sci J 2012; 6:703-771.
- Lorensia A, Muntu CM, Suryadinata RV, et al. Effect of lung function disorders and physical activity on smoking and non-smoking students. J Prev Med Hyg 2021; 62:E89-E96.
- Alqahtani JS, Oyelade T, Aldhahir AM, et al. Prevalence, severity and mortality associated with COPD and smoking in patients with COVID-19: A rapid systematic review and meta-analysis. PLoS One 2020; 15:e0233147.
- Evans MD, Pryor WA. Cigarette smoking, emphysema, and damage to alpha 1-proteinase inhibitor. Am J Physiol 1994; 266:L593-611.
- Taylor DH, Hasselblad V, Henley SJ, et al. Benefits of smoking cessation for longevity. Am J Public Health 2002; 92:990-996.
- van Schayck CP, Kaper J. Smoking and COPD: Will they ever vanish into smoke? Primary Care Respir J 2006; 15:81–83.
- Di Stefano A, Capelli A, Lusuardi M, et al. Severity of airflow limitation is associated with severity of airway inflammation in smokers. Am J Respir Crit Care Med 1998; 158:1277–1285. ‘
- Twisk JW, Staal BJ, Brinkman MN, et al. Tracking of lung function parameters and the longitudinal relationship with lifestyle. Eur Respir J 1998; 12:627-634.
- Holmen TL, Barrett-Connor E, Clausen J, et al. Physical exercise, sports, and lung function in smoking versus nonsmoking adolescents. Eur Respir J 2002; 19:8-15.
- Viju T Mhase, Reddy PSN. Effect of smoking on lung functions of workers exposed to dust and fumes. Indian J Community Med 2002; 27:1–3.
- Rubeena Bano, Mahagaonkar AM, Kulkarni NB. Study of pulmonary function tests among smokers and non-smokers in a rural area. Pravara Med Rev 2009; 4:11–15.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Muhammad Ali1*, Ruqaya Nangrejo1, Saba Abrar1, Adnan Anwar2, Asma Bilquis1 and Qamer Aziz1
1Department of Physiology, Baqai Medical University, Karachi, Pakistan2Department of Physiology, Hamdard University, Karachi, Pakistan
Received: 29-Jan-2022, Manuscript No. JRMDS-22-52761; , Pre QC No. JRMDS-22-52761 (PQ); Editor assigned: 29-Jan-2022, Pre QC No. JRMDS-22-52761 (PQ); Reviewed: 14-Feb-2022, QC No. JRMDS-22-52761; Revised: 18-Feb-2022, Manuscript No. JRMDS-22-52761(R); Published: 25-Feb-2022
