Review Article - (2022) Volume 10, Issue 12
STEM CELLS REGENERATION AND TISSUE ENGINEERING.
Meghna Jagdish Paryani*, Anuja Ikhar and Priyanka Rajesh Bhojwani
*Correspondence: Dr. Meghna Jagdish Paryani, Department of Conservative Dentistry and Endodontics, Sharad Pawar Dental College and Hospital, Datta Meghe Institute of Medical Sciences (Deemed to be university), Sawangi (Meghe), Wardha, Maharashtra, India, Email:
Abstract
The objective of the article is to look at the clinical importance of regenerative cells in renewal by going over the following points over the latest research on regenerative cell regeneration potential. New therapy options for tooth and periodontal healing have evolved as a result of regenerative cell based tissue engineering. Regenerative cells of the periodontal ligament, regenerative cells of the dental pulp and apical papilla regenerative cells are the main regenerative cell populations used in periodontal regeneration, which include bone marrow derived mesenchymal regenerative cells and the main dental derived mesenchymal regenerative cell populations. Dentistry is very interested in tissue engineering and biology of the regenerative cells because they may provide a fresh approach to the manufacture of therapeutic materials and tissue regeneration. These regenerative cells, that can be identified and produced in controlled tissue culture environments, could be employed in tissue engineering applications such as dental tissues and bone repair. Because of their potential to self-renew and specialise into specific tissues, dental stem cells have emerged as a viable option for regenerating teeth and periodontal tissue. As a result, dental stem cell based regeneration medicine's potential to repair damaged tooth tissue or grow new teeth has been highlighted. In a variety of clinical trials, oral stem cells have been shown to effectively assist the creation of dental specialised structures and disease repair.
Keywords
Stem cell, Tissue engineering, Regeneration of the periodontium, Regeneration of the dental pulp, Mesenchymal stem cells
Introduction
Regenerative endodontic involves the replacement of inflamed pulpal tissue with regenerated pulp like tissue [1]. Cell transplantation or cell homing can be used to regenerate the oral pulp. The first is a cell based technique for regeneration of the root canal in which exogenous stem cells are infused into the host's root canal system via scaffolds containing signalling molecules. The transplanted cells are collected from the host or from other people and processed or cultured in cultures to boost their numbers. Regenerative cells are the key to regeneration of tissue in this scenario. Periodontal regeneration aims to recapitulate the crucial stages of wound healing associated with periodontal development in order to restore lost tissues to their original form and function [2]. Technique to boost periodontal regeneration is to inject bioactive polypeptide growth factors directly into the gums [3]. Components to the surface of the root in order to stimulate wound healing and the growth of new cementum and connective tissue. Two of the most well studied are Insulin Like Growth Factor-I (ILGF-I) and Platelet Derived Growth Factor (PDGF), both of which have shown to accelerate renewal in dogs and monkeys with disease of the periodontium [4,5]. BMPs, or morphogenetic proteins of bone, have also been demonstrated to promote regeneration of cementum and bone [6]. This protein function is yet unknown. The epithelial sheath of Hertwig’s is known to create them and they play a major part in cement genesis and periodontal attachment apparatus betterment [7]. For tooth and periodontal regeneration, dental and non-dental mesenchymal regenerative cells are employed (MSCs). Mesenchymal regenerative cells are multi potency stromal cells that differentiate into osteoblasts and chondrocytes, among other cell types [8]. For the first time, they were discovered in the bone marrow. Dental pulp regenerative cells, the first mesenchymal regenerative cells isolated from teeth of the humans, have the ability to divide in vitro into odontoblasts, osteoblasts, chondrocytes as well as neurocytes [9]. Cytokines are key signaling molecules in regeneration of the pulp because they mobilise endogenous cells and regulate the differentiation of regenerative cells. Oral regenerative cells, such as dental pulp regenerative cells, regenerative cells of the periodontium and apical papilla regenerative cells, have been found in a variety of teeth and tooth supporting tissues and are similar to bone marrow mesenchymal regenerative cells in vitro [10,11]. Periodontal Ligament Stem Cells (PDLSCs) are able to differentiate into adipogenic and osteogenic cells, under defined culture conditions in vitro and could mediate the regeneration of the periodontium in vivo [12]. Understanding the features of different dental regenerative cells and they might be used in tooth regeneration is critical. The most important studies in the field of oral regenerative cells and tooth regeneration are summarized in this study (Figure 1).
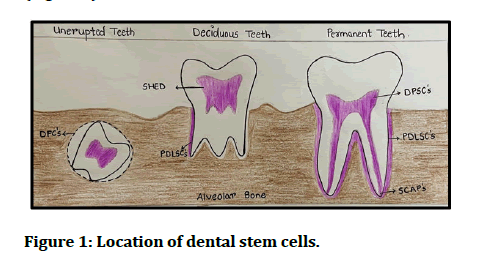
Figure 1: Location of dental stem cells.
Literature Review
Regeneration of the dental pulp
Because pulpal regenerative cells can differentiate into odontoblastic cells, they have been used for pulpal regeneration and in vitro research to generate biocompatible materials. For many years, the goal of pulpal regeneration research and clinical trials has been to eliminate the need for traditional treatments. The pulp in the teeth is a connective tissue that links the mineralized dentin to the connective tissue of the tooth. Dentin, a porous matrix resembling that of a bone, surrounds the tooth pulp. The dentin pulp complex is represented by both tissues. Dentinogenesis starts off by odontoblastic cells, the mineralized cells of the pulpal cells. Odontoblasts can help to repair modest damaged hard tissue caused by tooth decay. DPSCs are perivascular cells that exhibit mesenchymal regenerative marker cells such as CD105 and CD44 among others. DPSC like cells, also called as regenerative cells of human exfoliated deciduous teeth, were also found in human deciduous teeth. Deciduous teeth that have been exfoliated in human’s stem cells can be grown as flexible sticky cells or clusters resembling neurospheres. Dental pulpal regenerative cells are multi potent and have ability to differentiate into non oral tissue cells. The dental regenerative cells in this setting. A simple cell migration experiment could be utilized to improve MDPSCs. In transplantation of an ectopic tooth study of mice, these migratory cells produced more angiogenic and neurotropic factors than pulpal regenerative cells and they had a better ability to heal the dental pulp. Another example of remarkable DPSCs was identified by papaccio and colleagues. Isolation of a CD45-DPSC cell population was possible. The glycoprotein CD34, a hematopoietic progenitor cell hallmark, is present in these stem cells, unlike the normal pulpal regenerative cells found by Shi and colleagues. Despite the fact that the regenerated bone at the sites of graft looked nothing like typical alveolar bone, clinical testing showed that these CD34+cells produced functional bone tissue. According to Paino et al., CD34+DPSCs can create vascularized, tissue of the woven bone without the usage of a scaffold. Dental pulpal regenerative cells are multi potent and have the ability to Trans differentiate into non dental tissue cells. Dental mesoderm is commonly employed for the regeneration of injured neural tissues since it is formed from neural crest cells rather than skeletal mesenchyme stem cells from the lateral plate mesoderm. The use of chemotactic proteins like Stromal Cell Derived Factor (SDF)-1 to drive stem cell migration from the periapical region into the root canal is known as cell homing. As a result, immune rejection isn't a concern. The regulatory approval process for using this technology in human patients would be lot simpler and the cost would be much reduced. However, the outcome may be influenced by the distance that cells must travel, therefore the greater the root length, the worse the prognosis. Adult patients with fewer or no destitute stem cells may also be ineligible for such treatment, despite the fact that these individuals make up the bulk of endodontic practice patients. Large periapical lesions may necessitate lengthy treatment durations since a high level of disinfection is required for successful regeneration and it will take time for the lesion to heal before a source of stem cells becomes available for homing into the root canal space. REPs are a biological concept that combines regenerative cells and signaling molecules. The 'pulp dentine complex' is currently repaired rather than fully regenerated and root maturation is unpredictable. However, some practitioners believe that using REPs to treat young teeth with pulp necrosis is the best therapy option.
Regenerative cells of the periodontal ligament
Ligament of the periodontium is a specialized connective tissue which connects the teeth to rest of the body. It is a tissue of vascularization that has an increased rate of cellular and extracellular constituent turnover. Like all connective tissues, the ligament of the periodontium is consisting of cells also including an extracellular component consisting of collagenous and noncollagenous extracellular matrix. Among the constituent cells are osteoclasts and osteoblast (cells imprisoned in the ligament but functionally related to bone) fibroblasts, resting malassez epithelial cells, cement blasts and undifferentiated mesenchyme cells, (also present inside the ligament but functionally associated to cementum).
Collagenous and non-collagenous proteins are well differentiated in the extracellular compartment. Periodontitis is an infection of the soft and hard tissues that support the teeth that is the leading cause of loss of tooth. Immunomodulation is reduced in mesenchymal regenerative cells from inflammatory ligaments. MSC mediated tissue engineering for periodontal regeneration is now possible thanks to advances in regenerative medicine. Ligament of periodontal regenerative cells are the most important potential regenerative cells in periodontal regeneration among all mesenchymal regenerative cells. To achieve regeneration of the periodontium, periodontal ligament regenerative cells were transplanted directly into periodontal deficient areas. When autologous and allogeneic periodontal ligament regenerative cell were implanted into surgically created periodontal defect sites in small pigs, they were able to regenerate periodontal tissues. SCAPs are a recent type of MSC that can be present in the apical papilla of juvenile permanent teeth. SCAP seems to be the source of primary odontoblasts, which are responsible for the production of root dentin, whereas replacement odontoblasts are thought to come from Dental Pulp Stem Cells (DPSCs). They have been demonstrated to develop into odontoblasts and generate dentin when transplanted subcutaneously into immune compromised mice. Furthermore, data suggests that SCAPs can cause rise to a variety of cell lineages which including osteogenic and odontogenic cells, making them a prospective source for regenerative cell based therapy.
Discussion
Mesenchymal regenerative cell like populations produced from dental tissue are among the many different stem cell types discovered and characterized in specialized tissues. The periodontium and dentine, which lacks ameloblastic cells or other cell elements during development of tooth, have some regenerative or reparative potential. The presence of multi potent progenitor cells that can develop into functional, lineage specific cells is thought to be the reason for this. When compared to bone marrow derived mesenchymal regenerative cells, oral tissue derived progenitor cells are more constrained in their biological potency. Because, unlike bone tissues, oral tissues do not undergo continual remodeling, this is the case. Because of its early association with the neural crest, oral mesenchyme is also known as 'ectomesenchyme.' As a result, these ectomesenchyme derived oral regenerative cells are likely to have characteristics comparable to neural crest cells. The ligament of the periodontium contains cell populations that can develop into cement oblasts or osteoblasts, according to previous research. These cells can transform into cement blasts like cells and collagen forming cells, among other dental and non-dental tissues and can form postnatal regenerative cell like clonogenic colonies. Periodontal ligament stem cells, when injected into immune compromised animals, can form a cementum and ligament like structure and aid in regeneration of the periodontium. Periodontal ligament regenerative cells have ability to regenerate in a variety of dental and a craniofacial abnormality has been extensively studied in a variety of animal models. Periodontal ligament regenerative cells placed in the mouth produce cementum and periodontal ligament like structures that are identical to those found in the normal periodontal complex, according to the research. Within four weeks of autologous re-implantation of excised dental roots coated with PDL cells in mini pigs, connective tissue that looked like periodontium and mimicked the orientation of the fibre bundles formed. Periodontal ligament cell sheets have recently emerged as a novel alternative approach for periodontal tissue engineering because the technical handling of the implanted cell population avoids disruption of critical cell surface proteins such as ion channels, growth factor receptors and cell to cell junction proteins. Periodontal regeneration involving the formation of new bone, periodontal ligament and cementum was identified in three out of five test sites after eight weeks when autologous periodontal ligament cell sheets were implanted into dehiscence and intra-bony defects in dogs. PDLSCs were combined with regenerative cells from the root apical papilla in a HA, TCP and Gel form carrier to form a functional root or periodontal complex capable of sustaining a porcelain crown in miniature pigs in a more ambitious study. Before the implant constructs were put and sutured, the extraction socket was cleansed to ensure that all periodontal ligament tissues were removed before the lower incisor was extracted. The implant's surface was surgically opened three months after implantation and a porcelain crown resembling a small incisor of pig was placed and bonded onto a pre formed spot of the implant. Four weeks following crown placement, a CT scan and histological investigation demonstrated root or periodontal structural repair with much greater compressive strength than defects that did not get regenerative cells. This proof of concept work proved the viability of adopting a multi type regenerative approach of cells to reconstruct a bio physiological root or reconstruction. However, before these treatments can be employed as a standard of care in clinical practice, a number of challenges must be overcome.
Conclusion
Tissues of the periodontium that have been damaged due to trauma are extremely difficult to regrow. During periodontal regeneration, many factors that parallel periodontal growth must be considered, such as the selection of the best population of the progenitor cell and the matrix scaffold in a chronological and geographic order. While the ligament of the periodontium is now recognized as a rich source of regenerative cells of the bone marrow, it is challenging to harness and use this potential for clinical applications. Tissue engineering has so far relied on extra oral and oral tissue derived regenerative cells and progenitor cells. Numerous studies had looked into using dental stem cells to enhance bone for dentin/pulp complex regeneration or regeneration of the periodontium. Human dental stem cells, on the other hand, are unlikely to be suited for whole tooth regeneration. It's worth mentioning that oral stem cells have already been employed to regenerate brain tissue. The beneficial effect is assumed to be due to paracrine actions. Tooth and regeneration of the periodontium with stem cells may become more frequently used in clinical applications as the efficacy of tooth and periodontal regeneration improves.
References
- Eramo S, Natali A, Pinna R, et al. Dental pulp regeneration via cell homing. Int Endod J 2018; 51:405-419.
- MacNeil RL, Somerman MJ. Development and regeneration of the periodontium: Parallels and contrasts. Periodontal 2007; 19:8–20.
- Han J, Menicanin D, Gronthos S, et al. Stem cells, tissue engineering and periodontal regeneration. Aust Dent J 2014; 59:117-130.
- Lynch SE, de Castilla GR, Williams RC, et al. The effects of short term application of a combination of platelet derived and insulin like growth factors on periodontal wound healing. J Periodontol 1991; 62:458–467.
- Rutherford RB, Ryan ME, Kennedy JE, et al. Platelet derived growth factor and dexamethasone combined with a collagen matrix induce regeneration of the periodontium in monkeys. J Clin Periodontol 1993; 20:537–544.
- Ripamonti U, Reddi AH. Periodontal regeneration: Potential role of bone morphogenetic proteins. J Periodontal Res 1994; 29:225–235.
- Boss Hardt DD. Biological mediators and periodontal regeneration: A review of enamel matrix proteins at the cellular and molecular levels. J Clin Periodontol 2008; 35:87–105.
- Hu L, Liu Y, Wang S. Stem cell based tooth and periodontal regeneration. Oral dis 2018; 24:696-705.
- Miura M, Gronthos S, Zhao M, et al. SHED: Stem cells from human exfoliated deciduous teeth. USA. Proc Natl Acad Sci 2003; 100:5807-5812.
- Sonoyama W, Liu Y, Fang D, et al. Mesenchymal stem cell mediated functional tooth regeneration in swine. PLOS One 2006; 1:e79.
- Sonoyama W, Liu Y, Yamaza T, et al. Characterization of the apical papilla and its residing stem cells from human immature permanent teeth: A pilot study. J Endod 2008; 34:166-171.
- Seo BM, Miura M, Gronthos S, et al. Investigation of multi potent postnatal stem cells from human periodontal ligament. Lancet 2004; 364:149-155.
Author Info
Meghna Jagdish Paryani*, Anuja Ikhar and Priyanka Rajesh Bhojwani
Department of Conservative Dentistry and Endodontics, Sharad Pawar Dental College and Hospital, Datta Meghe Institute of Medical Sciences (Deemed to be university), Sawangi (Meghe), Wardha, Maharashtra, IndiaCitation: Meghna Jagdish Paryani, Anuja Ikhar, Priyanka Rajesh Bhojwani, Stem Cells Regeneration and Tissue Engineering, J Res Med Dent Sci, 2022, 10 (12): 211-214.
Received: 03-Oct-2022, Manuscript No. JRMDS-22-66150; , Pre QC No. JRMDS-22-66150(PQ); Editor assigned: 07-Oct-2022, Pre QC No. JRMDS-22-66150(PQ); Reviewed: 21-Oct-2022, QC No. JRMDS-22-66150; Revised: 06-Dec-2022, Manuscript No. JRMDS-22-66150(R); Published: 13-Dec-2022
