Research - (2021) Volume 9, Issue 1
The Corona Chronicle from History TO Hitherto: A Dental Outlook
Aravind Kumar Subramanian1*, B Nivethigaa1 and Vivek Narayan2
*Correspondence: Aravind Kumar Subramanian, Department of Orthodontics and Dentofacial Orthopedics, Saveetha Dental College and Hospital, SIMATS, Saveetha University Tamilnadu, India, Email:
Abstract
COVID-19 has a global outbreak since its discovery in Hubei province, China in December 2019. Following this it had been declared as a “Public Health Emergency of International Concern” on 30th January 2020 by the World health Organization (WHO). Corona viridae, the causative species that is not new to the society yet poses serious threat to life in under developed to welldeveloped nations. First occurrence of such enveloped, non-segmented, single-stranded RNA viruses with club shaped projections was cited back in 1930’s attributing to cause respiratory infection in domesticated chickens. The human corona viral illness was eminently noted around 1960’s wherein healthy human volunteers were relied on to detect the virus involved in the causation of common cold, an infection of the upper respiratory tract. Tracing back the etiology of such sickness, emergence from the bats and transmission and adaptation in other mammals have occurred which had further led to extensive layout of the malady. It was after the year 2003 when the human population was heavily affected, these infections were thrown to limelight indicating the fierce nature of this mutated subspecies. Since then so many disease variants have been identified including Severe Acute Respiratory Syndrome (SARS-CoV), the Middle Eastern Respiratory syndrome (MERS-CoV), Bat corona virus (RaTG13) and the COVID 19 (The novel coronavirus- initially named to be SARS-CoV-2). Not just the upper respiratory tract anymore, this disease had turned out to be more aggressive affecting the entire system causing a complete shutdown. Knowing the various possible modes of spread of this contagious disease, dental fraternity poses most risk due to transmission through contact, especially the aerosols. But the atypical nature of this virus, with increasing number of mutated subspecies no possibility exists in using a routine antiviral drug to completely eradicate this infection. Diagnostics can play an important role in the containment of COVID-19, enabling the rapid implementation of control measures that limit the spread through case identification, isolation, and contact tracing. This chapter focuses on the epidemiological report, the pathogenesis involved and the sequalae of occurrence of coronal viral disease in humans with an update on the recent one, a brief overview of various diagnostic tools utilized including Molecular assays, Nucleic acid testing (RT-PCR), CT Scans and a dental outlook on how the spread occurs along with methods by which dental setup could be immunized to intercept any further viral ailment.
Keywords
COVID, Corona virus, Pandemic, Pathogenesis, SARS CoV-2, Respiratory tract infection, Dental implications
Introduction
The word pandemics isn’t new to this society. Since the time mankind evolved several new infections have been identified every now and then. It ranged in severity from mild flu to several deadly infectious diseases [1–6]. Plague, a bacterial disease first noted years ago around 1st century AD in several countries around the world [7]. The cholera had been deadlier in almost all the continents [8]. One major factor eminent in all these was that episodes of recurrence happened decades after the original outbreak. Ensuing incidences were due to some mutated subspecies which proved to be even lethal than the original disease itself [9,10]. Similar outburst happened in 2003 when the corona viral infection was first noted in human beings [11]. Flare-up of the mutated form of this viral infection had occurred in many nations far off from the original epicenter of the disease [12–14]. China reported an endemic viral infection among the residents of Wuhan, Hubei province, China around mid-December 2019. Although initially this disease was believed to contained within that geographical region it had rapidly spread to the other countries. Analyzing the scenario then, World health Organization announced it as a “Public Health Emergency of International Concern” on 30th January 2020. From then so many countries around the world has been alarmed of its fast spread and detrimental nature. Even three months after this, till date the spread of viral infection could not yet be controlled.
Occurrence of Corona viridae (the causative organism), an enveloped, non-segmented, single-stranded RNA virus with club shaped projections was cited back in 1930’s attributing to cause respiratory infection (zoonotic) in domesticated chickens [15,16]. The human corona viral illness was eminently noted around 1960’s wherein healthy human volunteers were relied on to detect the virus involved in the causation of common cold, an infection of the upper respiratory tract [17]. Tracing back the etiology of such sickness, emergence from the bats and transmission and adaptation in other mammals have occurred which had further led to extensive layout of the malady [18].
Epidemiology of the outbreak
Initially these cases presented with symptoms like pneumonia which included fever, difficulty in breathing, dry cough with a ground glass appearance of alveoli in both the lungs. The shanghai public health center along with the central hospital of Wuhan, released the Novel corona virus genomic sequence, which was believed to have caused the outbreak in the Hubei province [19].
On 31st of December, the Wuhan municipal health commission had put forward a formal statement indicating the spread of viral infection of unknown etiology in the Hubei province. It remained unclear regarding the antecedent involved in causation of this disease. The origin of this disease was then believed to be the seafood market in that location [20]. When fever and pneumonia was witnessed in cluster of cases at Wuhan Jinyintan Hospital, Broncho-alveolar lavage was performed, samples were collected and tested, it revealed SARS like corona virus strain, Bat CoV, RaTg 13 which showed almost 96% identity. Following isolation from cell lines, the appearance of crown like particles were confirmed which was then identified as SARS CoV 2. Also, postmortem samples confirmed widespread alveolar damage in both the lungs with cellular exudates of fibro-myxoid type. Evidence were in favor of Acute respiratory distress syndrome (ARDS) [21].
The number rose on 2nd of January when 41 patients who presented with similar symptoms were confirmed positive with n-COV infection. Ratio between male and female showed greater incidence of the disease in the male population (male being 73% among the overall infected people). Also, the mean age was then found to be 49 years. The prevalence of other systemic diseases like diabetes, hypertension and cardiovascular disease in exposed individuals posed a risk for developing extreme life-threatening symptoms among exposed individuals. At the start, seeing the nosocomial spread of the disease, this disease was thought to have a less aggressive spread. Since 16th of January 2020 there was a 10-fold increase in the total number of reported cases and cumulative score for the number of people rose to 440 on 22nd January 2020 [22].
Modes of transmission
Not just for corona virus, any contagious viral infection can have direct or indirect spread. Direct spread of the virus includes transmission through actual contact with infected person and various secretions from them such as cough, sneeze, or respiratory droplet. Indirect spread occurs through contact transmission with particles inhalation of aerosol contaminated with the virus, or any other surfaces where the infected person had been in contact with. Few of these are till now confirmed with human corona virus transmission. Respiratory spread of the virus has occurred with contact either directly with droplets of different sizes and through saliva directly or indirectly. Few cases have also been identified to be caused by asymptomatic carriers, like on in the Germany [23]. Medical procedures result in the synthesis of aerosol particles which become carrier of infection to the health care workers. The alpha and beta forms of the virus are said to use respiratory system as a main mode for transmission wherein the gamma and delta forms of the virus were transmitted through the fecal mode. Few studies suggest that the fecal route of transmission is possible for the mutated corona species and hence it can pose a problem to sanitation workers which can build up the chain of spread of this viral infection. In a study on the first few infected cases in United States of America it results from r RT-PCR test for the human stool have confirmed the presence of virus in the stool sample on the 7th day in the active phase of coronal viral disease [24].
Pathogenesis of COVID-19 [25] (Figure 1)
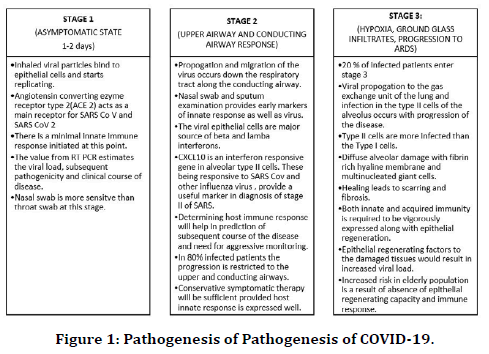
Figure 1. Pathogenesis of Pathogenesis of COVID-19.
Clinical features
The initial symptoms included fever, cough, muscle pain and tiredness; infrequent symptoms that occurred in very few cases were cough with sputum, headache, hemoptysis, diarrhea, new loss of taste sensation, hemoptysis, dyspnea and lymphopenia [26]. Almost all the patients had trouble in breathing and presented with a classical ground class appearance on CT with pneumonia like symptoms [27].
There was a mean 10-day delay between exposure and presentation of clinical signs and symptoms, with an average of 5-6-day incubation period and 4-5 delay in hospitalization of infected individuals [28]. From the period of onset, death occurred in about 6 to 41 days based on the severity of the condition. More deceased were found to be the elderly population above the age group of 70 years and those who had other systemic ailments. Emergency medical care should be sought if the patient has trouble in breathing, diffuse and prolonged pain in the chest region, delirium, bluish discoloration of the lips and the face [29]. IL2, IL7, GCSF, IP10, MCP1, MIP1A and TNF alpha were found higher in patients who were under ventilator assisted breathing. Vascular lesions and skin lesion were reported in a few cases [30].
Complications and clinical outcomes
In COVID 19 positive cases apart from the acute respiratory distress syndrome patients also developed other complications including arrhythmia, shock, acute cardiac injury, kidney injury, liver dysfunction and few other secondary infections [31–36]. Stage III of the disease progression usually results in such multi organ failure especially in elderly people and neonates whose inbuilt innate immune system is week to respond to the viral attack [27].
Criteria to assess severity of COVID – 19
Mild cases: Cases that has remained in stage 1 or 2 without further progression. Only mild clinical symptoms persist with no cough or respiratory findings. Imaging doesn’t provide any detail in this stage.
Moderate cases: Fever, appearance of respiratory symptoms and ground glass appearance in the chest radiograph [37].
Severe cases: difficulty in breathing, partial pressure of oxygen drops to less than 300 mmHg and rapid timely changes appearing in the successive radiographs. Based on these findings need for vigorous treatment is decided [38].
Critical cases: Inability to respire without the help of a ventilator, respiratory and cardiogenic chock with a multi organ failure. Need for extensive monitoring is required with ventilator assisted breathing [39].
Radiographic diagnosis
Radiological assessments are vital in the discovery and the management of COVID-19 [40]. Ground glass opacity was seen in the chest radiographs in advanced stage but during the initial stage of the disease this feature is not evident. Hence chest radiography is not recommended as the confirmatory imaging modality for initial diagnosis of COVID–19. Significant number of clinicians proposed CT scan ought to be one vital assistant analytic strategy since it is increasingly sensitive in determining the severity [41,42].
The chest CT findings include ground glass opacities (GGO), peripheral subpleural distribution, patchy consolidations and crazy – paving pattern (GGO with superimposed inter and intra-globular septal thickening) [43]. GGO is a hazy increase in attenuation that appears in a variety of interstitial and alveolar processes with preservation of bronchial and vascular margins [44]. High resolution CT (HRCT) for the chest is basic for early finding and assessment of sickness seriousness of patients with SARSCoV- 2 [45]. According to the fifth trial version chest CT discoveries of viral pneumonia are viewed as the clinical finding of COVID-19 disease. In the initial stages of the pneumonia pure GGO appearance can be present. Pleural effusion, lung cavitation, lymphadenopathy and calcification are infrequently reported [44]. Diseases which appear similar to pneumonia must be distinguished from COVID–19. The other causes of pneumonia include streptococcus pneumonia, chlamydia pneumonia and older coronavirus infections. The COVID–19 also mimics certain other diseases such as common cold, influenza, SARS and MERS. Thin slice CT is recommended which aids not only in diagnosis but also to determine the extent of the disease. Even though CT findings are non-specific they significantly aid in the diagnosis of COVID–19.
Laboratory diagnosis
The virus spread through the respiratory mucosa and contaminate different cells, initiate a cytokine storm in the body, produce a progression of resistant reactions, and cause changes in peripheral WBCs and immune cells, for example, lymphocytes [46,47]. Patients might show normal WBCs or leukopenia, lymphopenia, or thrombocytopenia, with prolonged activated thromboplastin time and high C-reactive protein [44]. RT–PCR stands for reverse transcription polymerase chain reaction. At present, RT-PCR test remains the reference standard to make a complete conclusion of COVID-19 contamination [48]. The test involves reverse transcription of SARS-CoV-2 RNA into complementary DNA (cDNA) strands, followed by amplification of specific regions of the cDNA [49]. The measure can be structured as a two-target framework, where one primer recognizes various coronaviruses counting SARS-CoV-2 and a subsequent primer set just recognizes SARS-CoV-2.
RT–PCR can be a single step or a dual step process. In the former the reverse transcription and PCR amplification are grouped into a single reaction. In the latter the reaction is done separately. The dual step process is more sensitive but also more time consuming. The samples are obtained from the upper respiratory tract and is the broadly recommended sample. Those who exhibit symptoms of a productive cough lower respiratory samples are obtained. The upper respiratory samples include nasopharyngeal swabs, oropharyngeal swabs, nasopharyngeal washes, and nasal aspirates. Lower respiratory tract samples include sputum, and tracheal aspirates. In the initial 14 days after beginning, SARS-CoV-2 could most dependably be distinguished in sputum followed by nasal swabs. There are three issues that have emerged with RT-PCR. To start with, the accessibility of PCR reagent packs has not kept up with request. Second, community clinics outside of urban communities come up short on the PCR foundation to oblige high test throughput. Finally, RT-PCR depends on the nearness of perceptible SARS-CoV-2 in the sample gathered. COVID-19 is presently determined by RT-PCR and has been screened for with CT scans, however both the procedure has its own downsides [50,51].
Differential diagnosis
✓ Common cold.
✓ Influenza.
✓ SARS.
✓ MERS.
✓ Chlamydia pneumoniae.
✓ Human meta-pneumonia virus.
✓ Human rhinovirus.
✓ Adenovirus.
✓ Primary viral or bacterial pneumonia.
Dental office a potential hotspot for spread of the virus
From the available resources on mode of transmission of the viral infection it is noticeably clear that the dental office can be a hotspot since transmission can occurs through direct contact with an infected patient to the dental health care workers or vice versa. The reason being the long incubation period before the active phase of the infection which has extended to 14 days after the initial time of contamination with the pathogen on the host, hence increasing the difficulty for the doctor to readily isolate these cases. Studies have shown the spread through saliva, which here proves to be the most common mode of transmission. This can happen when the cough or sneeze from the infected person had been contacted with. The corona virus has been shown to have a higher affinity towards the Angiotensin converting enzyme (ACE) receptors. Based on the coding studies done, it had been presumed than the ACE receptors predominate in number in the salivary gland than in the lungs. Confirmatory studies on this fact had fetched eye opening particulars that salivary glands (major and minor) are reservoirs for the corona virus especially among the asymptomatic carriers [52- 54].
Air and contact borne infection
Literatures have given a clear note on spread of the corona viral disease. It becomes inevitable to avoid all these while treating a patient. The concept of using a face mask and social distancing is not applicable in a dental setup. Spread can occur through the droplets propelled when the patient sneezes or coughs without mask while examining or while performing treatment and the aerosol that is generated while doing a dental procedure. Not just the oral secretions but also exposure to conjunctival, nasal secretions and the blood contamination from the infected patients can happen with the aerosols that are generated using micromotor and aerator handpiece. These particulate materials are formed in huge amount that the dental office becomes completely infected after procedures are done. Apart from this airborne direct spread, indirect spread can also occur in case of improper disinfection of the contaminated instruments. Understanding the different modes of spread of the disease, the dental setup is a highly susceptible place for acquiring and transmission of diseases, especially the aerosol borne particulate matter. The viral particles remain suspended over a longer period time of about 2 hours to even 9 days and a relative humidity of 50% it is more virulent than at 30%. Hence spread of such infection can be avoided by maintaining clean and dry environment.
Decision on need for dental treatment
Dentist should be professionally trained to manage such pandemic conditions. They must have the ability in diagnosing a case for Novel corona virus and isolating them. If in case they happen to identify any new case, then the infection control department must be alerted regarding this issue and the proper preventive and interceptive measures to be taken care of to prevent spread outside the dental office and within the health care workers. Dental treatment can be emergency care or elective care. Any patient in the active phase of the disease is completely unfit to undergo dental treatment. Almost all elective procedures can be postponed in patients during this period. But a dental emergency can arise anytime. Under such circumstances to act with caution is highly necessary to protect the dentist, dental assistant and the other patients who visit the dental fraternity.
Patient examination and isolation
Teleconferencing with the patient should be followed as the first step in any outpatient set up. Patient should be made aware about the seriousness of the current situation, asked for subjective signs of any active disease and any recent history of travel history or possibility in being within the epidemiological link. For this preparing, a questionnaire and following it for all patients will help us avoid negligence. This questionnaire should be filled in teleconferencing or when the patient enters the dental clinic before any examination is even started.
This should include the following criteria to be asked for
✓ Any history of recent illness including sore throat, fever, cough or rhinitis or other respiratory problems.
✓ Any history of recent travel abroad.
✓ Any history of recent travel within state.
✓ Any history of contact with people infected with the disease.
✓ Any history of infection in the neighborhood.
✓ Any history of active infection within family members.
✓ Any history of recent participation in groups or gatherings.
If any these questions turn out to be positive patient is advised to check for any active viral infection or remain in self-quarantine for the next 14 days. Patients’ further visit to the dental office is deferred until further notice from the health authorities on the status of the patient.
For walk in patients, the patient is systematically analyzed now patient enters into the dental office. Patient should be made sure that their temperature is within normal range of <100 F. For this contactless heat sensors should be used.
1. If any of these turns out to be positive like a patient experiencing any symptoms or those having a history of travel to COVID affected regions,
a. In case of life-threatening emergent situation patient can be allowed to come to the hospital set up but must be treated with special PPE precautions and separate waste protocol and negative pressure chamber.
b. If otherwise, for situations that can be brought under control with pharmacological agents, appropriate prescription can be given such that the patient returns to the dental office after he is tested negative for COVID (i.e., after two weeks preferably) and immediate dental treatment is avoided.
c. Elective dental procedures can be completely avoided, and the patient should be well educated regarding the lesser need of treatment at that point in time.
2. For those patients without any history of travel, possible epidemiological link or symptoms, dental treatment can be performed. But treatment involving the aerosol production can be deferred till the outbreak is brought under control, for the sake of remaining within the safety margin.
3. If the use of aerosol generating procedure becomes a part of necessary emergency care, then all the precautionary measures should be properly taken care off including the use of high-pressure suction for evacuation and proper isolation protocol involving rubber dams.
Immunization protocol for routine dental practice
i. Personal protective equipment
Earlier we did not have any proper guidelines for protective care for COVID 19. Recently it had been put forth by dental council existing in various countries. Few cases of COVID 19 have also been identified among dentists who treated asymptomatic infected patients, insisting the need to follow such council made protocol and guideline. Considerations have been given in terms of hand hygiene, use of personal protective equipment i.e., gown, eye protection goggles, and Facemask (N95 or higher-level respirator), their disposal and reuse strategies should be properly followed according to the CDC protocol and also the manufacturers instruction.54. Personal protective equipment to be worn while treating all patients preferably a sterilized one for each patient. Based on the spread of infection and increased need for control the wear of personal protective equipment has been subdivided into three categories [55,56]. In general cases which do not have any history, and the questionnaire is negative, Primary protection, use of facemask, gloves with a regular use sterilizable protective coat for the dental assistant. Advanced secondary protection can be attained for the dentist by the wear of facemask, surgical gloves, headcap, protective face shield, regular use protective coat along disposable isolation clothes on the outside. Tertiary level of care is required if the patient is in the active phase of the disease or under self-quarantine or if the questionnaire turns out to be positive. These patients are not advised to reach for any dental setup for elective treatments but in case of emergency extreme levels of protection should be followed by the dentist and the dental assistants and the number of people in the working area should be kept as minimum as possible [57,58].
ii. Hand Hygiene: The route of transmission had made it compulsory to follow extensive handwashing techniques. It is very essential to not acquire or transmit the disease and not be a potential carrier of transmission to others. Health advisories have advised following these protocols every time someone visits a new place or been in contact with another person. This same applies to a dental facility as well. In the clinic handwashing is followed by the patient when they enter in before any procedure or after the procedure is over. And the dentist is advised to follow hand hygiene before examining the patient, before starting any procedure, after the procedure is completed and when contacting with any dental unsterilized instruments or surfaces or if they meet blood saliva or other droplet anytime during the entire procedure. Care to be taken in avoiding contact with eye, nose and mouth anytime between the procedures, before an alcohol rub sanitizer is used.
iii. Mouth rinsing: Procedural mouth rinse with 1% hydrogen peroxide or povidone iodine is suggested to reduce the oral viral load and making it a better environment to carry out emergency procedures.
iv. Disposable instruments: Instead of the regular use stainless steel mouth mirror and probe for examination and isolation, it is better to use a disposable mouth mirror, probe, disposable needles, and single use materials on the patients.
v. Rubber dam isolation: With the aim of avoiding blood and saliva contamination with the aerosol, use of proper method of isolation such as a rubber dam kit can be considered. Aerosol that is generated can be evacuated using a high-volume evacuator that is used in case of surgical procedures. Those which leads to aerosol production should be avoided. Use of caries dissolving agents, atraumatic restorative treatment without handpiece and also hand scalers to be preferred over modernized aerosol generating procedures.
vi. Radiographs: Use of extraoral radiographs to be preferred over intraoral radiographs and also when intraoral radiographs are indicated, use of proper double layered barrier technique to be followed.
vii. Airborne infection isolation chambers: All suspected and confirmed cases, to be treated in negative pressure rooms or air borne infection isolation chambers. But this cannot be provided in a regular dental setup. Hence it would be more reasonable to treat these dental emergencies in a medical setup if the patient is either tested positive for COVID 19 or quarantined as a susceptible individual. The dental emergencies in such conditions include only the maxillofacial trauma or space infections like cellulitis, dentoalveolar abscess etc., which would turn into a life-threatening emergency if left untreated.
viii. Disinfection of dental office: Every time a patient moves out of the dental clinic, it is the responsibility of the dental assistant to clean all the in animate surfaces so that the viral spread through contact with these can be avoided. The dental assistant should be trained adequately regarding the importance of disinfection and sterilization twice as fold as in every day dental practice.
ix. Anti-retraction devices: In few cases even there is a chance of retrograde contamination of the waterline that supply the chair. This can act as potential reservoir to spread infection. Need for anti-retraction devices is vital at this point. Handpieces without anti retraction devices should be prohibited from use. And newer inventions should be made for the other dental water supplies also so that any retrograde infection can thus be prevented.
x. Dental waste management: Categorization of the dental waste need to be done and disposed in sealed container to prevent the spread of infection among the sanitation workers who collect and dispose the waste.
xi. In case of any sickness reported among the dental assistants, they must be strictly advised not to come to the dental office and handle any clinic related materials. If normal flu like symptoms subside in a day or two, then they can return to work once they are normal. But in case if it persists, they might be advised to maintain quarantine and seek adequate professional help.
Acknowledgments
The authors would like to extend their gratitude to Saveetha Dental and Hospital for providing a platform for this research.
Conflict of Interest
Nil.
References
- Taubenberger JK, Morens DM. 1918 Influenza: The mother of all pandemics. Rev Biomed 2006; 17:69-79.
- https://www.researchgate.net/profile/Taisuke_Horimoto/publication/7684820_Influenza_Lessons_from_past_pandemics_warnings_from_current_incidents/links/551c8d3d0cf2fe6cbf792596.pdf
- Epstein J. Modelling to contain pandemics. Nature 2009; 460:687.
- Tumpey TM, Basler CF, Aguilar PV, et al. Characterization of the reconstructed 1918 Spanish influenza pandemic virus. Science 2005; 310:77-80.
- Hsieh YC, Wu TZ, Liu DP, et al. Influenza pandemics: Past, present and future. J Formosan Med Assoc 2006; 105:1-6.
- https://books.google.co.in/books?hl=en&lr=&id=KYtAkAIHw24C&oi=fnd&pg=PP11&dq=pandemic&ots=09SNC5kD3G&sig=queK5oFCUEgHBUysh2z2isoUmXw&redir_esc=y#v=onepage&q=pandemic&f=false
- Butler T. Plague history: Yersin’s discovery of the causative bacterium in 1894 enabled, in the subsequent century, scientific progress in understanding the disease and the development of treatments and vaccines. Clin Microbiol Infection 2014; 20:202-209.
- https://www.researchgate.net/publication/327350457_Cholera_Pandemics_1816-1861
- Chatterjee P, Kanungo S, Bhattacharya SK, et al. Mapping cholera outbreaks and antibiotic resistant Vibrio cholerae in India: An assessment of existing data and a scoping review of the literature. Vaccine 2020; 38:A93-A104.
- Jutla A, Khan R, Colwell R. Natural disasters and cholera outbreaks: Current understanding and future outlook. Curr Envir Health Rpt 2017; 4:99-107.
- van der Hoek L, Pyrc K, Jebbink MF, et al. Identification of a new human coronavirus. Nature Med 2004; 10:368-373.
- Woo PCY, Lau SKP, Huang Y, et al. Coronavirus diversity, phylogeny and interspecies jumping. Exp Biol Med 2009; 234:1117-1127.
- Holmes KV. SARS associated coronavirus. New England J Med 2003; 348:1948-1951.
- Chafekar A, Fielding BC. MERS-CoV: Understanding the latest human coronavirus threat. Viruses 2018; 10:93.
- https://www.annualreviews.org/doi/full/10.1146/annurev-virology-110615-042301?fbclid=IwAR2YIAsxULSnpTkYXS_rGpa_AK8_-wsT8n3T-MgxHIEG3sQB4v1HzKN1VcQ
- Brian DA, Baric RS. Coronavirus genome structure and replication. In: Enjuanes L Edn. Coronavirus replication and reverse genetics. Current Topics in Microbiology and Immunology. Springer 2005; 1-30.
- Cavanagh D. Coronavirus avian infectious bronchitis virus. Vet Res 2007; 38:281-297.
- Lun ZR, Qu LH. Animal-to-Human SARS-associated coronavirus transmission? Emerg Infect Dis 2004; 10:959.
- http://www.ncbi.nlm.nih.gov/nuccore/MN908947.3
- http://wjw.wuhan.gov.cn/
- Lu H. Drug treatment options for the 2019-new coronavirus (2019-nCoV). BST 2020; 14:69-71.
- https://www.imperial.ac.uk/media/imperial-college/medicine/mrc-gida/2020-01-22-COVID19-Report-2.pdf
- Rothe C, Schunk M, Sothmann P, et al. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. New England J Med 2020; 382:970-971.
- Holshue ML, DeBolt C, Lindquist S, et al. First case of 2019 novel coronavirus in the United States. New England J Med 2020.
- Mason RJ. Pathogenesis of COVID-19 from a cell biology perspective. Eur Respir J 2020; 55:2000607.
- Ren LL, Wang YM, Wu ZQ, et al. Identification of a novel coronavirus causing severe pneumonia in human: A descriptive study. Chinese Med J 2020.
- Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020; 395:497-506.
- http://www.imperial.ac.uk/mrc-global-infectious-disease-analysis/covid-19/report-1-case-estimates-of-covid-19/
- https://www.cdc.gov/coronavirus/2019-ncov/index.html
- Bouaziz JD, Duong TA, Jachiet M, et al. Vascular skin symptoms in COVID‐19: A French observational study. J Eur Acad Dermatol Venereol 2020; 34.
- Terpos E, Ntanasis‐Stathopoulos I, Elalamy I, et al. Hematological findings and complications of COVID-19. Am J Hematol 2020; 95:834-847.
- Lodigiani C, Iapichino G, Carenzo L, et al. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thrombosis Res 2020; 191:9-14.
- Klok FA, Kruip MJHA, van der Meer NJM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thrombosis Res 2020; 191:145-147.
- Long B, Brady WJ, Koyfman A, et al. Cardiovascular complications in COVID-19. Am J Emergency Med 2020; 38:1504-1507.
- Filatov A, Sharma P, Hindi F, Espinosa PS. Neurological complications of coronavirus disease (COVID-19): Encephalopathy. Cureus 2020; 12.
- Kochi AN, Tagliari AP, Forleo GB, et al. Cardiac and arrhythmic complications in patients with COVID-19. J Cardiovascular Electrophysiol 2020; 31:1003-1008.
- Gandhi RT, Lynch JB, del Rio C. Mild or moderate Covid-19. N Engl J Med 2020; 2020:NEJMcp2009249.
- Hadjadj J, Yatim N, Barnabei L, et al. Impaired type I interferon activity and inflammatory responses in severe COVID-19 patients. Science 2020; 369:718-724.
- Li K, Wu J, Wu F, et al. The clinical and chest CT features associated with severe and critical COVID-19 pneumonia. Invest Radiol 2020.
- Chen SG, Chen JY, Yang YP, et al. Use of radiographic features in COVID-19 diagnosis: Challenges and perspectives. J Chin Med Assoc 2020; 83:644-647.
- Hui TCH, Khoo HW, Young BE, et al. Clinical utility of chest radiography for severe COVID-19. Quant Imaging Med Surg 2020; 10:1540-1550.
- Choi H, Qi X, Yoon SH, et al. Extension of coronavirus disease 2019 (COVID-19) on chest CT and implications for chest radiograph interpretation. Radiology 2020; 2:e200107.
- Pan F, Ye T, Sun P, et al. Time course of lung changes on chest CT during recovery from 2019 novel coronavirus (COVID-19) pneumonia. Radiology 2020:200370.
- Zu ZY, Jiang MD, Xu PP, et al. Coronavirus disease 2019 (COVID-19): A perspective from China. Radiol 2020; 200490.
- Pan Y, Guan H, Zhou S, et al. Initial CT findings and temporal changes in patients with the novel coronavirus pneumonia (2019-nCoV): A study of 63 patients in Wuhan, China. Eur Radiol 2020.
- Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet 2020; 395:507-513.
- Tang YW, Schmitz JE, Persing DH, et al. Laboratory diagnosis of COVID-19: Current issues and challenges. J Clin Microbiol 2020; 58:e00512-20.
- Yang W, Yan F. Patients with RT-PCR-confirmed COVID-19 and normal chest CT. Radiology 2020; 295:e3.
- Udugama B, Kadhiresan P, Kozlowski HN, et al. Diagnosing COVID-19: The disease and tools for detection. ACS Nano 2020.
- Tahamtan A, Ardebili A. Real-time RT-PCR in COVID-19 detection: Issues affecting the results. Expert Review Mol Diagnostics 2020; 20:453-454.
- Chan JFW, Yip CCY, To KKW, et al. Improved molecular diagnosis of COVID-19 by the novel, highly sensitive and specific COVID-19 RdRp/Hel real-time reverse transcription-PCR assay validated in vitro and with clinical specimens. J Clin Microbiol 2020; 58.
- Xu J, Li Y, Gan F, et al. Salivary glands: Potential reservoirs for COVID-19 asymptomatic infection. J Dent Res 2020.
- Ather A, Patel B, Ruparel NB, et al. Coronavirus disease 19 (COVID-19): Implications for clinical dental care. J Endodont 2020.
- https://www.cdc.gov/coronavirus/2019-ncov/hcp/dental-settings.html
- https://covid19.elsevierpure.com/en/publications/personal-protective-equipment-and-covid-19
- https://academic.oup.com/jamia/article/27/6/967/5815267
- Peng X, Xu X, Li Y, et al. Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci 2020; 12:9.
- Seto WH, Tsang D, Yung RWH, et al. Effectiveness of precautions against droplets and contact in prevention of nosocomial transmission of severe acute respiratory syndrome (SARS). Lancet. 2003; 361:1519-1520.
Author Info
Aravind Kumar Subramanian1*, B Nivethigaa1 and Vivek Narayan2
1Department of Orthodontics and Dentofacial Orthopedics, Saveetha Dental College and Hospital, SIMATS, Saveetha University Tamilnadu, Chennai, India2Department of Oral Medicine and Radiology, Saveetha Dental College and Hospital, SIMATS, Saveetha University Tamilnadu, Chennai, India
Citation: Aravind Kumar Subramanian, B Nivethigaa, Vivek Narayan, The Corona Chronicle from History TO Hitherto: A Dental Outlook, J Res Med Dent Sci, 2021, 9 (1): 319-327.
Received: 28-Nov-2020 Accepted: 04-Jan-2021
