Research - (2020) Volume 8, Issue 3
The Effect of Different Cement Space Thickness on Fracture Strength of CAD/ CAM all Ceramic Crown Restorations
Mohammed T Mohammed1 and Adel F Ibraheem2*
*Correspondence: Adel F Ibraheem, Department of Conservative and Esthetic Dentistry, College of Dentistry, University of Baghdad, Iraq, Email:
Abstract
Objectives: The purpose of this in vitro study was to evaluate the effect of variable cement space thickness on the fracture strength of CAD/CAM all ceramic crown restorations.
Materials and method: 16 sound human maxillary first permanent premolar teeth of comparable size and shape extracted for orthodontic purposes were collected and selected to be used in this in vitro study. All the dimensions of each crown were tested with using one-way ANOVA in order to reduce the confounding variables. The teeth samples were divided into two main groups according to the different cement space parameter setting (n=8). Group A: 0 cement space around the margin and additional cement space of 100 Mm starting 1mm above the finish lines of the teeth. Group B: 0mm cement space around the margin and additional cement space of 120 Mm starting 1mm above the finish lines of the teeth. Standardized tooth preparation for full contour monolithic ceramic crown restorations for all samples was done with the following preparation features: Deep chamfer finishing line of 1 mm thickness, axial reduction 1-1.5mm, occlso-axial height 4mm, anatomical occlusal reduction and total convergence angle 6 degree. The teeth were then scanned using 3 shape intra-oral digital scanner. Sirona In-Lab MC X5 milling device was used to fabricate the all ceramic crowns. Then the crowns are cemented with dual cure self-adhesive resin cement Rely X™ U200, and then tested with computer controlled Universal testing machine (Laryee, Beijing, China) and the mode of fracture also has been noted.
Results: The study revealed that the mean of fracture resistance of all ceramic crowns in Group A and Group B were (1688.75N), (1936.25 N) respectively. Student’s t-test was then applied to see whether the difference between two groups statistically significant or non, this test reveal, that, there is statistically a significant difference between two groups at p>0.05.
Conclusions: increasing cement space parameter setting significantly improve the fracture strength of all ceramic restoration.
Keywords
Cement space, Lithium disilicate, All ceramic crown
Introduction
The increasing demand for esthetics in the posterior region of the mouth and environmental concerns about restorations containing metal were behind the evolution of new techniques for fabrication of posterior inlays, onlays, and crowns [1].
Such restorations have several advantages, including lifelike appearance, biocompatibility, wear resistance, and color stability. However, their drawbacks include brittleness, especially glass or feldspathic ceramics, susceptibility to fracture, causing excessive wear to oppose dentition, requiring more involved tooth reduction, and being technique sensitive. When non-metallic crowns undergo fracture, the fracture typically originates from flaws or defects in the intaglio surfaces. Subcritical crack growth follows, which is enhanced in the aqueous environment. Ceramic materials are particularly susceptible to the tensile stresses, and mechanical resistance is also strongly influenced by the presence of superficial flaws and internal voids. Such defects may represent the sites of crack initiation.
This phenomenon may be influenced by different factors such as marginal design of the restoration, residual processing stress, magnitude and direction and frequency of the applied load, elastic modulus of the restoration components, restoration–cement interfacial defects, cement film thickness and oral environmental effects. The introduction of computer-aided design / computer-aided manufacturing (CAD/CAM) technology in dentistry enabled dentists to use new treatment modalities and changed the design and application limits of all-ceramic restorations as the demand for esthetics in the posterior region of the mouth has increased. Recent lithium disilicate restorations have provided functional, biocompatible, and esthetic demands. The strength of an all- ceramic restoration depends not only on the fracture resistance of the material, but also on a suitable preparation design, cement space thickness and adequate material thickness.
The lack of sufficient relief spaces in these areas impedes the flow of cement beyond the occlusal portion of the casting, resulting in incomplete seating due to hydraulic pressure [2]. Pilo, et al. said when the crown restoration precisely fits the prepared tooth, the escape pathway of cement between the crown restoration and prepared tooth surface become more difficult [3]. The final effects are creation of premature, occlusal contacts, inappropriate proximal contacts, marginal discrepancies and lack of coziness [4]. Many methods have been suggested previously in order to minimize post cementation marginal discrepancy such as Venting [5]. Cement escape channels and Internal relief space Internal relief space for cement has been shown to increase the marginal fit between restoration and preparation of the tooth, decreasing the risk of cement breakup, plaque accumulation, chronic decay and parodontal problems and restore support and load distribution to the restoration substrate [6]. All these advantages obtained from internal relief space might improve the fracture strength of cemented all ceramic crown. Thus, the aim of this in vitro study was to evaluate the effect of different cement spacer thicknesses on fracture resistance of CAD/CAM all ceramic crown restorations.
Materials and Methods
Sixteen natural sound maxillary first premolar with two roots that extracted for orthodontic reason were selected and collected to be used in this study. The teeth were kept in moist condition by immersing in distilled water. All teeth were then embedded in individual block of cold cure acrylic resin to 2 mm apical to cemento enamel junction. The acrylic block was constructed with (2.0 cm height=1.5 cm diameter) [7]. Dental surveyor (Dentaurum, Germany) was used to position the long axis of the tooth parallel to that of the acrylic resin block (Figure 1).
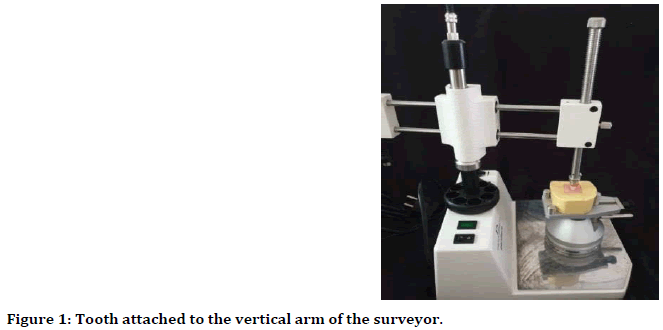
Figure 1. Tooth attached to the vertical arm of the surveyor.
Prior to teeth preparation, the pencil was used to demarcate the future finish line position. In order to obtain standardized preparation, a high speed water coolant handpiece connected and secured to dental surveyor upper arm, while acrylic specimen holding the tooth was adapted to the surveyor mobile lower member, by this way the long axis of the bur can be kept parallel to the long axis of the tooth throughout the cutting procedure. Each specimen was prepared to receive the recommended following preparation guidelines by ivoclar vivadent: anatomical occlusal reduction, 1 mm chamfer finishing line all around the tooth with a total circumferential axial reduction of about (1.5 mm) and 6 mm total axial tapering (Figure 2).
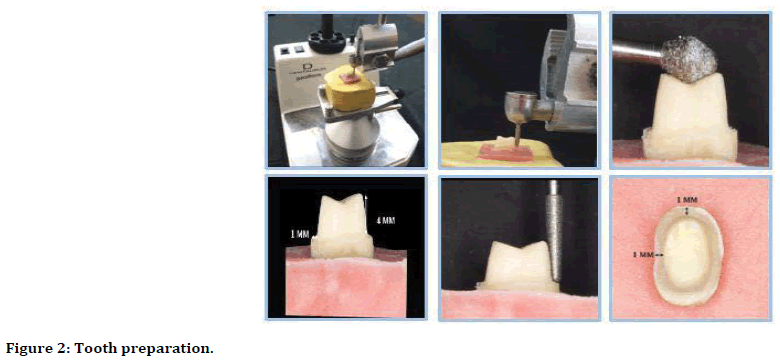
Figure 2. Tooth preparation.
All specimen is randomly divided into two groups A and B by the cement space thickness (n=8): the cement space parameter in Group A was set at 100 mm and for Group B was set at 120 mm. (Figure 3). Each sample were scanned using the 3-shaped intra-oral digital scanner (3-Shape, Copenhagen, Denmark) with Exo Cad software to create a 3D digital image for all teeth. The crowns were then milled with the MC X5 (Sirona Dental System, Germany) milling machine, IPS e.max CAD ceramic lithium disilicate blocks for CEREC and In Lab (Ivoclar Vivadent, Schaan, Liechtenstein).
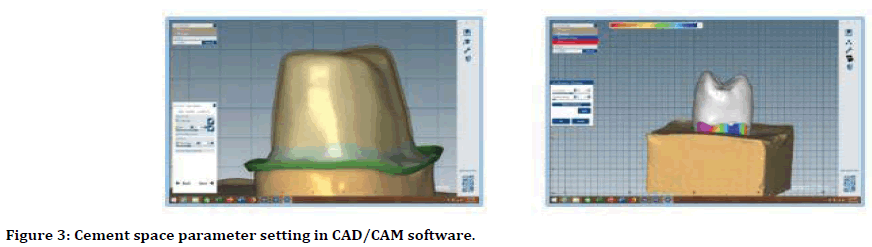
Figure 3. Cement space parameter setting in CAD/CAM software.
A custom-made holding device was especially fabricated to be used as a screw that secured the lithium disilicate crown on the natural tooth sample during marginal checking and cementation procedure to maintain standardized seating forces. The device was designed to have a load sensor attached to it. Furthermore, a modification was done on this device so that it will hold the crown parallel to the path of insertion of the prepare tooth during crown seating procedure by attaching the vertical arm of the device to the vertical arm of the surveyor. In order to apply the seating force more evenly and parallel to the path of insertion, a square custom-made mold of 8 mm × 4 mm with central round hole about 1 mm larger from the crown circumferential was attach to the tighten screw end of the device. This central hole was filled, later on, during cementation procedure with special type of silicon to cover 3 mm of occlusal surface of each cemented crown. Each crown was seated on the tooth sample with a standard load of 5 Kg (≅50 N) (Figure 4) [8].
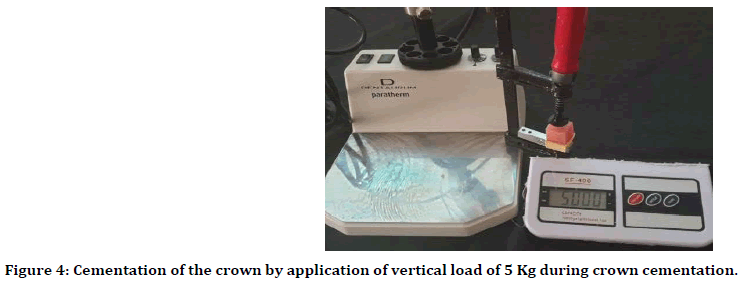
Figure 4. Cementation of the crown by application of vertical load of 5 Kg during crown cementation.
Prior the cementation procedure for all groups, the teeth were cleaned by alcohol, the luting agent were injected inside the inner surface of the crown until it complete filled. Each crown was, then, filled with the luting cement and seated over its respective tooth with finger pressure initially then a static load of 5 Kg was applied for 6 minutes according using the specimen holding device. Excess material was removed with a fine micro brush before complete polymerization. Each cemented specimen was kept for one hour to bench set. All specimens were then stored in distilled water at room temperature and then tested after one week after cementation [9].
Testing Procedure A single load to failure test using universal testing machine (Laryee, Beijing, China) (Figures 5 and 6) was used to assess the strength of the cemented crowns. In order to be suitable with the size of the specimen that used in this study, two modifications have been done on Instron test machine, one involved the upper jaw while the other involved the lower jaw. For upper jaw, Instron testing machine was mounted with a movable rod with semispherical head of 4 mm diameter attached to the upper jaw through the loading piston, while for the lower jaw, specially designed sample holding device was mounted to the lower jaw of the testing machine to securely hold the specimen.
Figure 5. The computer-controlled universal testing machine used in the study.
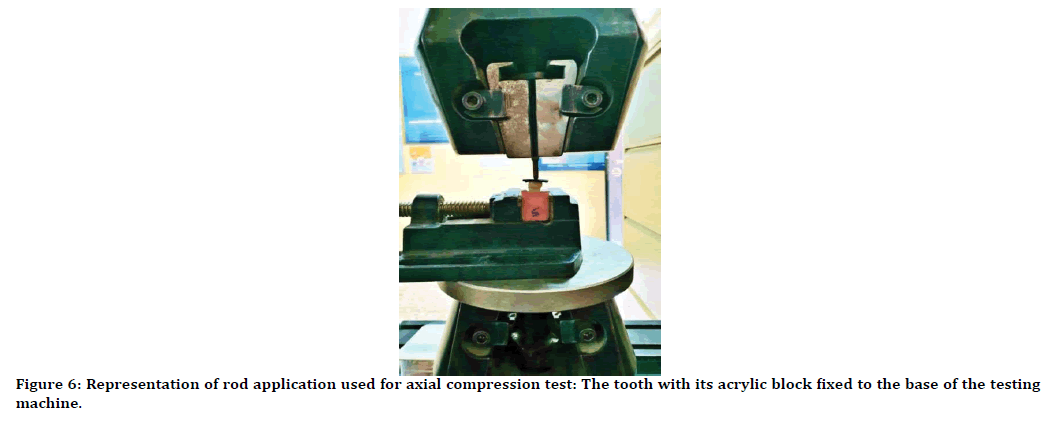
Figure 6. Representation of rod application used for axial compression test: The tooth with its acrylic block fixed to the base of the testing machine.
After one week of storage in distilled water, the specimen was secure on their position on Instron testing machine, the occlusal surface of the crown was covered by 1 mm thick rubber sheet, the loading force was then applied at the center of occlusal surface along the long axis of cemented crowns with a crosshead speed of 0.5 mm/min until fracture occurred [10]. All specimens were loaded up to fracture and a computer connected to the charging system automatically recorded the total breaking load of each sample in Newton (N) when rod’s end press on the slope of the cusps. Also, after the fracture strength test was completed, each specimen was examined visually using magnifying loupes (6 x) to assess the fracture mode as shown in Burke's classification (Table 1).
| Mode of fracture | Description |
|---|---|
| Code I | Minimal fracture or crack in crown |
| Code II | Less than half of crown lost |
| Code III | Crown fracture through midline (half of crown displaced or lost) |
| Code IV | More than half of crown lost |
| Code V | Severe fracture of crown and/or tooth |
Table 1: Burke's classification for the mode of fracture.
Results
The descriptive statistics including the mean, standard deviation, minimum and maximum values of the fracture strength in (N) of the two different groups are shown in Table 2.
| Groups | No | Mean | Std. Deviation | Minimum | Maximum |
|---|---|---|---|---|---|
| A | 8 | 1688.75 | 244.54 | 1448 | 2086 |
| B | 8 | 1936.25 | 188.53 | 1705 | 2252 |
Table 2: Descriptive statistics of fracture strength of the different groups measured in N.
Also from the Table 2 with (B) group in which the crowns are manufactured with cement space thickness 120 Mm ،the highest mean value of fracture strength as (1936.25 N), while the mean value was recorded in the groups (A) with cement space thickness 100 Mm is (1688.75N).
Additional t test also done to show the difference between the groups that luted with the same luting agent but with different cement space thickness as follow in Table 3. T test shown the significant difference of the fracture strength of the crowns fabricated with different cement space thickness and the same luting agent Table 4.
| Group A mean | Group B mean | T value | P value | Significance |
|---|---|---|---|---|
| 1688.75 | 1936.25 | -2.26709 | 0.019875 | S |
Table 3: T test for comparison of fracture strength among the groups with different cement space thickness.
| Groups | Code 1 | Code 2 | Code 3 | Code 4 | Code 5 | Total |
|---|---|---|---|---|---|---|
| Group A | 1(12.5%) | 7(87.5%) | 8 (100%) | |||
| Group B | 8 (100%) | 8 (100%) |
Table 4: Mode of fracture of the different groups.
Discussion
Material and method
In this analysis, freshly extracted human natural teeth are selected to be used as abutment teeth since the fracturing strength of all-ceramic restorations is heavily dependent on the supporting abutment's elastic component [11]. In addition, the use of natural teeth permits restoration adhesive cementation and more clinical relevance [12].
Due to the relative ease of their selection from patients in need of orthodontic treatment and can be collected as a sound tooth, maxillary first premolars were chosen for use in this study. Furthermore, relative to other teeth, maxillary premolars are the least variability in morphology [13].
To mimic the help of alveolar bone in a healthy tooth, all teeth samples are individually embedded in a cold cure acrylic resin block up to 2 mm apical to the CEJ [14].
Tooth preparation is dependent on material for all-ceramic crowns. The stated strength of any ceramic material by the manufacturers depends entirely on the material thickness and the design of the perpetration. Anything less than following the recommendations of the manufacturers will lead to a weaker final restoration. On the other hand, lithium disilicate's least suggested axial reduction is 1 mm. Therefore, the manufacturers of the materials used in this study recommend deep chamfer finshing line in this study regarding the type of finshing line. This type of finishing line has been found to provide better marginal adjustment of all-ceramic [8,15].
Planar occlusal reduction was performed because a clinical simulation should be used to prepare a tooth or model in vitro [16]. In addition, it was found that planar occlusal reduction will provide better marginal adaptation of the crown restoration when chamfer finishing line was used [8]. To obtain standardization for all specimens, teeth were prepared occluso-gingivally at a height of 4 mm [17]. Tooth preparation was performed using a modified dental surveyor to monitor tooth preparation variables including the degree of axial taper, finish line layout, and insertion route [18].
Digital impression using intra-oral scanner was used in this study to overcome the errors that could occur during the steps of conventional impression making, including the dimensional changes of the impression material and gypsum used to manufacture the master model [19]. The same digital process was used for the manufacture of crowns for standardization purposes, including the use of the same design software, design mode, parameters of restoration and milling unit. Design mode "Biogeneric Reference" using a first premolar dentoform as the reference tooth was selected in this study to provide a standardized morphology for crowns of all teeth.
In this analysis, dual-curing resin cement was used to ensure a high conversion rate and full cement healing due to differences in the degree of translucency of the materials used since these cements were cured by two mechanisms: chemical and photo-initiated. If insufficient light penetrates through the reconstruction during the cement's final light curing, the concrete is chemically cured [20]. Each crown was seated under a constant load of 5 kg (approximately 50 N) during cementation to simulate the biting force during clinical cementation [21]. During the load application, a piece of rubber material was placed on the occlusal surface of the crown to spread the load evenly across the entire occlusal surface and to mimic the cotton roll cushion effect medically used during crown cementation [22]. During the seating and cementation process of the lithium disilicate crown to the preparation teeth, a Specimen Holding and Cementing Device was used in this research [8]. A modification has been added to this tool, this improvement allows for more reliable crown restoration seats for all specimens by allowing a single uniform load path perpendicular to the occlusal surface during cementation In this research, single load to failure testing was used to check the fracture strength of crowns as this method provides useful information to compare the materials tested without the input of confounding variables from fatigue testing [23].
The load was applied in this experiment at a crosshead speed of 0.5 mm / min as it was found that lower speeds were followed by greater plastic deformation and higher fracture strength measurements could be obtained [24].
Many forces act in all possible directions in the dynamic masticatory process, the most important being the compressive force; therefore, the choice of load application parallel to the long axis of the tooth was chosen to simulate the physiological function and obtain a degree of non-axial loading through existing occlusal contact variations [7]. Placing a piece of rubber between the load applicator and the tested crown was intended to act as a stress breaker to prevent damage caused by the load applicator's direct contact with the tested crown and to mimic the cushion effect of food between opposing teeth [25].
Comparisons among groups
In this study, the statistically highly significant differences in the fracture strength between different groups could be attributed, in general, to the variable internal fitness of all ceramic crown restorations that fabricated with different cement space thickness.in which the higher cement space thickness of fabricated all ceramic crown had a higher fracture strength, These result findings are agreed with different previous studies like [26-29]. Regarding to previous studies, increased cement space thickness is correlating with decreased seating discrepancies and thinner cement thickness.
Also, a modulus of elasticity of the supporting structure has a role on the fracture strength of the all ceramic restoration, in which the higher the elastic modulus, the higher the load to the failure. The modulus of elasticity of the dentin is (16 GPa) and that of the luting cement is (6 to 8 GPa),so the thinner cement thickness is preferred for higher fracture strength of overlying all ceramic crown The way to have a thinner well distributed cement is by decreasing the hydraulic pressure while crown seating. This can be achieved by increase the cement space thickness of fabricated crown to provide more space for escape of excess cement during crown seating [30]. Despite the statistically significant differences in fracture strength between the different subgroups, it should be noted that the mean value of the fracture strength of the crowns in all groups exceeded the maximum bite strength in the premolar region (450 N) [31].
Mode of fracture
In this study, most of the samples of all groups showed severe fracture of the crown and tooth (catastrophic failure). This mode of fracture could be attributed to the nature of fracture test used, the single load to failure test, whereby the inclination of the cusps and the position of the load applicator during loading play a major role in determining the fracture behavior. Crown anatomy of the upper premolars with the sharp angle between the buccal and palatal cusps makes these teeth more susceptible to a mesiodistal split vertical fracture under occlusal load [32]. This mode of fracture was also found in previous studies done [33] and [34] who all found that static load to failure test provoked splitting of the crowns from the central fossa through the abutment mesio-distally below CEJ. On the other hand, this mode of fracture suggests a strong bond between the cemented crowns and their respective teeth owing to the adhesive cementation protocol used in this study. It has been shown that adhesive cementation reduces the risk of debonding of all-ceramic restorations due to its high bond strength to the tooth structure and ceramic restorative materials.
Limitation
One of the main limitations is that the study done in vitro (non-vital teeth) and the dentine quality of the samples is not identical exactly 100%.
Conclusion
The using of 120 μm cement space thickness with lithium disilicate crown fabrication to increase the fracture strength.
References
- Sunnegårdh-Grönberg K, Peutzfeldt A, van Dijken JWV. Flexural strength and modulus of a novel ceramic restorative cement intended for posterior restorations as determined by a three-point bending test. Acta Odontologica Scandinavica 2003; 61:87-92.
- White SN, Kipnis V. Effect of adhesive luting agents on the marginal seating of cast restorations. J Prost Dent 1993; 69:28-31.
- Pilo R, Cardash HS, Baharav H, et al. Incomplete seating of cemented crowns: A literature review. J Prost Dent 1988; 59:429-433.
- Mule SA, Dange SP, Khalikar AN, et al. Effect of varying layers of two die spacers on precementation space of full coverage restorations. J Indian Prosthodont Society 2014; 14:67-75.
- Jørgensen KD. Factors affecting the film thickness of zinc phosphate cements. Acta Odontologica Scandinavica 1960; 18: 479-490.
- Carter SM, Wilson PR. The effect of die-spacing on crown retention. Int J Prosthodont 1996; 9.
- Salameh Z, Sorrentino R, Papacchini F, et al. Fracture resistance and failure patterns of endodontically treated mandibular molars restored using resin composite with or without translucent glass fiber posts. J Endodont 2006; 32:752-755.
- Abdullah LS, Ibraheem AF. The effect of finishing line designs and occlusal surface reduction schemes on vertical marginal fit of full contour CAD/CAM zirconia crown restorations (a comparative in vitro study). Int J Dent Oral Health, 2017; 4:1-6.
- Oliva RA, Lowe JA. Effect of die spacer on the seating of cast restorations on composite core preparations. J Prost Dent 1987; 58:29-35.
- Tsitrou EA, Northeast SE, van Noort R. Evaluation of the marginal fit of three margin designs of resin composite crowns using CAD/CAM. J Dent 2007; 35:68-73.
- Dong XD, Wang HR, Darvell BW, et al. Effect of stiffness of cement on stress distribution in ceramic crowns. Chin J Dent Res 2016; 19:217-223.
- Chitmongkolsuk S, Heydecke G, Stappert C, et al. Fracture strength of all-ceramic lithium disilicate and porcelain-fused-to-metal bridges for molar replacement after dynamic loading. Eur J Prosthodont Restorative Dent 2002; 10:15-22.
- Monga P, Sharma V, Kumar S. Comparison of fracture resistance of endodontically treated teeth using different coronal restorative materials: An in vitro study. J Conservative Dent 2009; 12:154.
- Al-Joboury AI. An evaluation of the influence of different finishing lines on the fracture strength of full contour zirconia CAD/CAM and heat press all-ceramic crowns. J Baghdad College Dent 2015; 325:1-9.
- Al-Zubaidi ZA, Al-Shamma AM. The effect of different finishing lines on the marginal fitness of full contour zirconia and glass Ceramic CAD/CAM crowns (An in-vitro study). J Dent Materials Techniques 2015; 4:127-136.
- Contrepois M, Soenen A, Bartala M, et al. Marginal adaptation of ceramic crowns: A systematic review. J Prosthet Dent 2013; 110:447-454.
- Khdeir RM, Ibraheem AF. The marginal fitness of CAD/CAM all ceramic crowns constructed by two types of direct digitization techniques: An in vitro study. J Baghdad College Dent 2016; 325:1-4.
- Hmedat SJA, Ibraheem AF. An in vitro evaluation of fit of the crowns fabricated by zirconium oxide-based ceramic CAD/CAM systems, before and after porcelain firing cycles and after glaze cycles. J Baghdad College Dent 2013; 325:1-6.
- Pradíes G, Zarauz C, Valiverde A, et al. Clinical evaluation comparing the fit of all-ceramic crowns obtained from silicone and digital intraoral impressions based on wavefront sampling technology. J Dent 2015; 43:201-208.
- Arrais CAG, Rueggeberg FA, Waller JL, et al., Effect of curing mode on the polymerization characteristics of dual-cured resin cement systems. J Dent 2008; 36:418-426.
- Anunmana C, Charoenchitt C, Asvanund C. Gap comparison between single crown and three-unit bridge zirconia substructures. J Adv Prosthodont 2014; 6:253-258.
- Dimashkieh M. The effect of veneering porcelain on the marginal fit of cercon zirconia copings. 2010.
- Shahrbaf S, Van Noort R, Mirzakouchaki B, et al. Fracture strength of machined ceramic crowns as a function of tooth preparation design and the elastic modulus of the cement. Dent Mater 2014; 30:234-241.
- Siso ŞH, Hürmüzlü F, Turgut M, et al. Fracture resistance of the buccal cusps of root filled maxillary premolar teeth restored with various techniques. Int Endodont J 2007; 40:161-168.
- Beuer F, Stimmelmayr M, Gueth JF, et al. In vitro performance of full-contour zirconia single crowns. Dent Mater 2012; 28:449-456.
- Scherrer SS, De Rijk WG, Belser UC, et al. Effect of cement film thickness on the fracture resistance of a machinable glass-ceramic. Dent Mater 1994; 10:172-177.
- Aboushelib MN, Elmahy WA, Ghazy WH. Internal adaptation, marginal accuracy and microleakage of a pressable versus a machinable ceramic laminate veneers. J Dent 2012; 40:670-677.
- Molin MK, Karlsson SL, Kristiansen MS. Influence of film thickness on joint bend strength of a ceramic/resin composite joint. Dent Mat 1996; 12:245-249.
- Thompson VP, Rekow DE. Dental ceramics and the molar crown testing ground. J Applied Oral Sci 2004; 12:26-36.
- Lawn BR, Pajares A, Zhang Y, et al. Materials design in the performance of all-ceramic crowns. Biomaterials 2004; 25:2885-2892.
- Powers JM, Sakaguchi RL, Craig RG. Craig's restorative dental materials/edited by Sakaguchi RL, Powers JM. 2012; Philadelphia, Elsevier/Mosby.
- Sornsuwan T, Ellakwa A, Swain MV. Occlusal geometrical considerations in all-ceramic pre-molar crown failure testing. Dent Materials 2011; 27:1127-1134.
- Zhang Y, Mai Z, Barani A, et al. Fracture-resistant monolithic dental crowns. Dent Materials 2016; 32:442-449.
- Sieper K, Wille S, Kern M. Fracture strength of lithium disilicate crowns compared to polymer-infiltrated ceramic-network and zirconia reinforced lithium silicate crowns. J Mechanical Behavior Biomed Materials 2017; 74:342-348.
Author Info
Mohammed T Mohammed1 and Adel F Ibraheem2*
1Department of Restorative and Aesthetic Dentistry, College of Dentistry, University of Baghdad, Iraq2Department of Conservative and Esthetic Dentistry, College of Dentistry, University of Baghdad, Iraq
Citation: Mohammed T Mohammed, Adel F Ibraheem, The Effect of Different Cement Space Thickness on Fracture Strength of CAD/CAM all Ceramic Crown Restorations, J Res Med Dent Sci, 2020, 8 (3):181-188.
Received: 16-May-2020 Accepted: 01-Jun-2020
