Research Article - (2022) Volume 10, Issue 4
The Effect of Different Marginal Cement Space Thickness on the Fracture Strength of Monolithic Zirconia Crowns Using Different Luting Agents
*Correspondence: Ibtehal M Hussien, Department of Restorative and Esthetic Dentistry, College of Dentistry, University of Baghdad, Baghdad, Iraq, Email:
Abstract
Objectives: The main objective was to investigate the effect of marginal cement space thickness on the fracture strength of full contour monolithic zirconia crowns using different luting agents. Materials and methods: 48 sound human upper first premolar teeth were selected and prepared following the guidelines recommended for KATANATM zirconia. The prepared teeth were divided according to thickness of cement space around the margin into two main classes (n=24) as follow: (Class I: 0 μm) and (Class II: 25μm), additional cement space of 80 μm starting 1mm above the finish lines of the teeth. Every class was subdivided into three subclasses according to the type of luting material(n=8): subclasses(AI,AII) cemented with RelyX™ Ultimate adhesive luting agent, subclasses(BI,BII) cemented with RelyX™ Unicem 200 self-adhesive luting agent and subclasses(CI,CII) cemented with resin-modified glass ionomer cement (RMGIC). CAD/CAM was used to fabricate monolithic zirconia crown restorations; the fabricated crown was then luted to respective prepared tooth using the selected cementing agent for each subgroup. Compressive axial loading was used to evaluate the fracture strength of crowns via a computer-controlled universal testing machine. The statistical analysis of data was done by using one-way (ANOVA) and LSD test. Results: The tests revealed a significant impact of marginal cement space and luting agents on the fracture strength of zirconia crowns (p ≤ 0.05). Conclusions: The using of 25μm marginal cement space thickness results in better fracture strength of zirconia crowns. Additionally the Rely X™ Ultimate adhesive luting agent provided the highest fracture strength as compared with others.
Keywords
Zirconia, Marginal cement space, Monolithic crowns, Luting cement, CAD/CAM, Fracture strength
Introduction
As a result of increasing request for esthetically pleasing products, different manufacturing procedures for ceramic materials have been mostly studied in latest years [1]. Monolithic zirconia restorations have newly become common due to the evolution of CAD-CAM technology making it easier and less costly to fabricate. Different restoration parameters can be adjusted by CAD/CAM system settings during designing phase for example cement space and restorative material thickness [2]. A die-spacer (die relief) should be provided during the fabrication of crowns to decrease the resistance flow of the cementing material, which aids in full seating of the restoration and extrusion of excess cement from all preparation margins [3]. In addition, the positive effects of spacing are minimize the hydraulic pressure between the restoration and cement, improve adaptation, reduce marginal discrepancies and improve occlusal contact [4,5]. Hammood et al. evaluated the influence of different marginal cement space thickness on the internal and marginal fitness of full contour zirconia crowns. They found that zirconia crowns exhibited better marginal and internal fitness, when using 25μm marginal cement space thickness [6]. Also Nayyef et al. concluded that using of 25μm marginal cement space thickness decreased the microleakage of zirconia crown restorations [7]. Fracture strength, marginal fit and esthetics are the most essential factors for the success of ceramic restorations. The strength of restoration relays on the mechanical properties of the ceramic material, adequate material thickness, an appropriate preparation design, cement space thickness, and luting agent [8]. Manufacturers classify, compare, rank and advertise dental restoratives according to the fracture strength especially in posterior area [9]. For that reason, the present study was directed to investigate the influence of various marginal cement space and various luting agents on the fracture strength of full contour monolithic zirconia crowns.
Materials and Methods
48 sound human upper first premolar teeth (free from caries, cracks and enamel anomalies) were collected for use in this study. Teeth were obtained from patients with age range 18-25 years that extracted it for orthodontic reasons [10]. Each tooth was fixed into a singular block of acrylic resin up to 2mm apical to the cement-enamel junction (CEJ) to simulate level of alveolar bone support [11].
In order to achieve standardized preparation for all teeth, the crown’s preparation was carried out by one operator to exclude inter-examiner variations, furthermore modified dental surveyor was used during tooth preparation. Teeth were prepared to restore by monolithic zirconium crown restorations, the preparation protocol according to the guidelines recommended for KATANATM zirconia which involve the following characters: functional occlusal reduction, 0.8mm chamfer finishing line 1.5mm above CEJ with a (1-1.5mm) circumferential axial reduction, occlusogingival height was 4mm and 6º convergence angles [12]. A digital caliper was used to check the measurements of the height of axial wall and the depth of finishing line (Figure 1 A).
According to thickness of cement space around the margin, the samples were divided arbitrarily into dual major classes (n=24): (Class I: zero μm) and (Class II: 25 μm), additional cement space of 80 μm starting 1mm above the finish lines of the teeth. After that every class was subdivided into three subclasses (n=8) according to type of cement used: (AI, AII) luted with RelyXTM Ultimate ( adhesive resin cement, 3M ESPE, Germany), (BI,BII) luted with RelyXTM U200 ( self-adhesive resin cement, 3M ESPE, Germany) and (CI, CII) luted with Riva Luting Plus RMGIC (SDI,Australia) and additional cement space (for all samples) starting 1 mm above the finish line of the teeth were set at 80 μm [13].
Scanning of every tooth was done via Medit i700 intraoral scanner (Medit, Korea). Sirona InLab CAD 20.0 software was used for designing of crown . KATANA disk was then introduced and secured into the milling machine (Sirona CEREC in-Lab MC X5). After the milling was completed, all the produced zirconia crowns were white, chalky in color and larger than the original size by 20-25%, so they need dense sintering process to have their final color, strength and original size. The sintering process was done via the high temperature in Fire HTC speed (Sirona, Germany). After that the sandblasting of the internal surface of crown restorations were done with aluminum oxide particles (≤ 50 μm) and 2.5 bar at a distance of 3 cm for 15 sec.(3M ESPE,2017) using a Renfert sandblasting machine.
Crown restorations were seated on their relevant teeth and checked for any marginal discrepancies using a digital microscope (Dino-Lite, Taiwan) (Figure 1B). After that, the cementation process was carried out following the manufacturer instructions. The inner surface of crown was occupied by the cement and settled initially by finger pressure, a specimen holding cementation device was used to apply a weight of 5 kg for about 6 minutes [14]. Distilled water was then used for storage of samples for at least 24 hours prior to testing.
Compressive axial loading was used to measure the fracture strength of crowns via a universal testing machine (Qualitest, USA) by using rod 4 mm in diameter with a crosshead speed of 0.5 mm/min. To act as a stress breaker, a 1 mm thick piece of rubber was placed between the crown and the occluding rod [15]. Computer software recorded the data of the fracture load in Newton's (all samples were loaded until fracture occurred). After completing the test, each specimen was examined visually and Burke's classification was used for assessment the fracture [16] (Table 1) (Figure 1C). The statistical analysis of data was done using one-way (ANOVA) and LSD test (p ≤ 0.05).
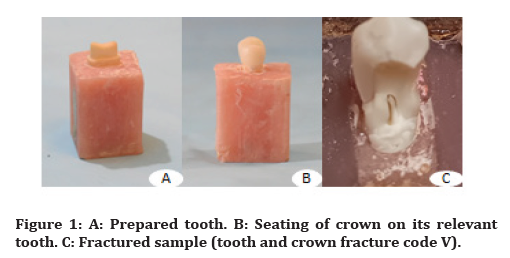
Figure 1. A: Prepared tooth. B: Seating of crown on its relevant tooth. C: Fractured sample (tooth and crown fracture code V).
| Code | Description |
|---|---|
| I | Minimal fracture or crack in the crown |
| II | Less than half of the crown lost |
| III | Crown fracture through midline (half of crown displaced or lost) |
| IV | More than half of the crown lost |
| V | Severe fracture of the tooth and/or crown |
Table 1: Modes of fracture as described by Burke in 1999
The descriptive statistical results of the fracture strength for the six subgroups measured in Newton (N) are recorded in Table 2. Table 2 reveals that the maximum mean of fracture strength was noted within subclass (AII) that represent the samples with 25 μm marginal cement space thickness with Rely X™ Ultimate adhesive luting agent (4832 N ± 251.29), whereas the minimum mean was noted within subclass (BI) that represent the samples with zero μm marginal cement space thickness with Rely X™ Unicem 200 self-adhesive luting agent (2571N ± 445.29).
| Classes | N | Mean | SD | Min. | Max. | |
|---|---|---|---|---|---|---|
| I | AI | 8 | 3577.38 | 251.29 | 3256 | 4090 |
| BI | 8 | 2571.75 | 445.29 | 2001 | 3149 | |
| CI | 8 | 2670.25 | 585.41 | 1854 | 3394 | |
| II | AII | 8 | 4832.13 | 426.6 | 4326 | 5405 |
| BII | 8 | 4074.25 | 550.69 | 3149 | 4855 | |
| CII | 8 | 4127.13 | 550.93 | 3168 | 4669 |
Table 2: Statistical analysis (Descriptive) of the fracture strength of six subclasses measured in N.
Furthermore Table 2 shows that the maximum mean of fracture strength within each individual class was as follow: For class I which represent crown with zero μm marginal cement space thickness, the maximum mean of fracture strength was showed within subclass (AI) (3577N ± 251.29), while the minimum mean of fracture strength was showed within subclass (BI)(2571N ± 445.29). For class II which represent crown with 25 μm marginal cement space thickness, the maximum mean of fracture strength was showed within subclass (AII) (4832.13N ± 426.60, while the lowest mean value was showed within subclass (BII)(4074.25N ± 550.69).
For comparison of significance among the different classes, one-way (ANOVA) test was used at a level of significance of 0.05 and revealed a statistically significant difference (p ≤0.05) (Table 3).
| Classes | Sum of squares | Df | Mean square | F | Sig. | |
|---|---|---|---|---|---|---|
| I | Between Classes | 4916959.083 | 2 | 2458479.542 | 12.208 | 0 |
| Within Classes | 4228958.875 | 21 | 201378.994 | (S) | ||
| Total | 9145917.958 | 23 | ||||
| II | Between Classes | 2864520.75 | 2 | 1432260.375 | 5.447 | 0.012 |
| Within Classes | 5521509.25 | 21 | 262929.012 | (S) | ||
| Total | 8386030 | 23 |
Table 3: One-way (ANOVA) test for comparison of significance between the different classes
Further comparisons among subclasses were done using LSD test with a level of significance (0.05) to localize the source of difference (Table 4). Table 4 shows that there was a statistically highly significant difference between AI and BI also between AI and CI while the difference between AII and BII also between AII and CII was statistically significance furthermore the difference between A2 and A3, also between B2 and B3 was statistically non significance.
| Dependent variable | (I)group | (J)group | Mean difference | Dependent variable | (I)group | |
|---|---|---|---|---|---|---|
| I | AI | BI | 1005.625 | 2.24E+02 | 0 | HS |
| CI | 907.125 | 2.24E+02 | 0.001 | HS | ||
| BI | AI | -1005.625 | 2.24E+02 | 0 | HS | |
| CI | -98.5 | 2.24E+02 | 0.665 | NS | ||
| CI | AI | -907.125 | 2.24E+02 | 0.001 | HS | |
| BI | 98.5 | 2.24E+02 | 0.665 | NS | ||
| II | AII | BII | 757.875 | 2.56E+02 | 0.008 | S |
| CII | 705 | 2.56E+02 | 0.012 | S | ||
| BII | AII | -757.875 | 2.56E+02 | 0.008 | S | |
| CII | -52.875 | 2.56E+02 | 0.839 | NS | ||
| CII | AII | -705 | 2.56E+02 | 0.012 | S | |
| BII | 52.875 | 2.56E+02 | 0.839 | NS |
Table 4: LSD test for comparison of fracture strength between the subclasses
Concerning the fracture modes, the majority of samples revealed sever tooth and crown fracture (code V). On the other hand, only few samples showed crown fracture only (Code IV) (Table 5).
| Codes(%)/Classes | I | II | III | IV | V | Total |
|---|---|---|---|---|---|---|
| AI | 8 (100%) | 8 (100%) | ||||
| BI | 1(12.5%) | 7(87.5%) | 8 (100%) | |||
| CI | 1(12.5%) | 7(87.5%) | 8 (100%) | |||
| AII | 8 (100%) | 8 (100%) | ||||
| BII | 8 (100%) | 8 (100%) | ||||
| CII | 8 (100%) | 8 (100%) |
Table 5: Mode of fracture of the different subclasses
Discussion
There are many studies evaluated the fracture strength of zirconium crown restorations based on the effect of different types of cement. However; limited available studies are present to assess the influence of different marginal cement space thickness on the fracture strength of zirconium crowns. When comparing fracture strength of the zirconium crowns using two different marginal cement space thickness and single luting agent, the highest mean of fracture strength values was recorded with 25 μm marginal cement space thickness, while the lowest mean was recorded with 0 μm marginal cement space thickness. This could be due to the following reasons: The 25 μm marginal cement space thickness of fabricated crown provides additional area for seepage of excess cement cervical more than occlusal during crown seating resulting in thinner cement film thickness, which leads to decrease the hydraulic pressure, evenly distributed cement and less seating crown discrepancies [17]. The difference in the elastic modulus of the supportive structure has a role on the fracture strength of the all restoration, which may contribute to stress build-up, ultimately leading to material failure. The elastic modulus of zirconia is (220 GPa), luting cement is (6 to 8 GPa) and that of dentin is (10 to16 GPa), so the lesser amount of cement is favored for higher fracture strength of zirconia crown restorations [18,19]. Also, when using 25 μm marginal cement space thickness that lead to the increased the interface leading to increase in the micromechanical interlocking, heavier bonding action and higher fracture strength [19,20]. On the other hand, intimate physical contact between the abutment, cement and ceramic could be observed that leads to good cement adaptation and improvement of the fracture strength, as transfer of stress will be better accomplished by a material with good adaptation.
However, it was statistically clear that the facture strength of the zirconia crown was improved with Rely X™ Ultimate adhesive luting agent in comparison to the Rely X™ Unicem 200 self- adhesive luting agent and Riva luting plus RMGI cement. This finding may be due to the following reasons: the use of phosphoric acid in adhesive cement steps increases the micromechanical interlocking between tooth substrate and resin, which increases the ability to bind and leads to heavier bonding action [20-22]. Also, single bond universal adhesive that was used before RelyX™ Ultimate adhesive luting agent application containing the functional monomers (particularly 10-methacryloxydecyl dihydrogen phosphate). It can improve the chemical bonding by creating chemical bonds with metal oxides of zirconia surface and produce secondary internal forces( van der Waals forces or hydrogen bonds) at the resin-zirconia interface. In addition, the functional monomers can demineralized the natural tooth, connect with calcium ions of the tooth structure (especially dentin) and produce insoluble calcium salts at the tooth-resin interface [23]. High flowability of RelyXTM Ultimate adhesive luting agent that has fine particle size and low viscosity as compared with the other two cements that were used in this study, resulting in increasing the bonding surface [23,24]. In addition, RelyXTM Ultimate adhesive luting agent characterized with high compressive strength, high bonding and low solubility in comparison with other two types of cement used in this study and this contribute to the stability of the zirconia crown which improved their fracture strength [25]. In contrast, the results of this study show that the fracture strength of zirconia crowns do not differ between RMGIC and Rely X™ Unicem 200 self- adhesive luting agent. Resin or conventional cementation of zirconia crown has been a controversial topic [26]. The result of the present study is in agreement with previous studies who reported that cementation with resin cement does not essentially result in higher fracture strength [19,24,26,27]. Although another researchers have found that luting agents would considerably affect the fracture strength of all-ceramic crowns [28,29], this disagreement may be due to the tested materials were glass-ceramic and feldspathic porcelain, which have much lesser flexural strength than zirconia, it is proposed that the high strength of zirconia contribute to prevail the influence of luting agents on it [19].
Conclusion
Within the limitation of this research, the main conclusions of this in vitro study include: The 25μm marginal cement space thickness was attributed to improve the fracture strength of monolithic zirconia crown significantly with all cement types used in this study as compared with zero μm marginal cement space thickness. The adhesive resin cement seems to guarantee significantly higher fracture strength for zirconia crown as compared with the self-adhesive resin cement and RMGIC that were used in this study.
References
- Yin R, Lee MH, Bae TS, et al. Effect of finishing condition on fracture strength of monolithic zirconia crowns. Dent Materials J 2019; 38:203-210.
- Kale E, Seker E, Yilmaz B, et al. Effect of cement space on the marginal fit of CAD-CAM-fabricated monolithic zirconia crowns. J Prosthetic Dent 2016; 116:890-895.
- Carter SM, Wilson PR. The effects of die-Spacidng on post-cementation crown elevation and retention. Australian Dent J 1997; 42:192-198.
- https://epublications.marquette.edu/cgi/viewcontent.cgi?article=1244&context=theses_open
- Mule SA, Dange SP, Khalikar AN, et al. Effect of varying layers of two die spacers on Precementation space of full coverage restorations. J Indian Prosthod Society 2014; 14:67-75.
- ED H, AF. I. Evaluate and compare the effect of different marginal cement space parameter setting in the CAD software on the marginal and internal fitness of monolithic zirconia crowns with different types of luting agents (A comparative in vitro study). J Res Med Dent Sci 2020; 8:74-80.
- Nayyef MI, Ibraheem AF. Marginal microleakage of monolithic zirconia crowns using different marginal cement space thickness and luting cements. J Res Med Dent Sci 2021; 9:17.
- D’Addazio G, Santilli M, Rollo ML, et al. Fracture resistance of zirconia-reinforced lithium silicate ceramic crowns cemented with conventional or adhesive systems: An in vitro study. Materials 2020; 13:2012.
- Wendler M, Belli R, Petschelt A, et al. Chairside CAD/CAM materials. Part 2: Flexural strength testing. Dent Materials 2017; 33:99-109.
- El-Helali R, Dowling AH, McGinley EL, et al. Influence of resin-based composite restoration technique and endodontic access on cuspal deflection and cervical microleakage scores. J Dent 2013; 41:216-22.
- Taha NA, Palamara JE, Messer HH. Cuspal deflection, strain and microleakage of endodontically treated premolar teeth restored with direct resin composites. J Dent 2009; 37:724-730.
- Hmedat SJA, Ibraheem AF. An in vitro evaluation of fit of the crowns fabricated by zirconium oxide-based ceramic CAD/CAM systems, before and after porcelain firing cycles and after glaze cycles. J Baghdad College Dent 2013; 25:43-48.
- Rekow ED, Harsono M, Janal M, et al. Factorial analysis of variables influencing stress in all-ceramic crowns. Dent Materials 2006; 22:125-132.
- Anunmana C, Charoenchitt M, Asvanund C. Gap comparison between single crown and three-unit bridge zirconia substructures. J Adv Prosthod 2014; 6:253-258.
- Tsitrou EA, Northeast SE, van Noort R. Evaluation of the marginal fit of three margin designs of resin composite crowns using CAD/CAM. J Dent 2007; 35:68-73.
- Burke F. Maximising the fracture resistance of dentine-bonded all-ceramic crowns. J Dent 1999; 27:169-173.
- Hoang LN, Thompson GA, Cho SH, et al. Die spacer thickness reproduction for central incisor crown fabrication with combined computer-aided design and 3D printing technology: An in vitro study. J Prosthet Dent 2015; 113:398-404.
- Guazzato M, Albakry M, Ringer SP, et al. Strength, fracture toughness and microstructure of a selection of all-ceramic materials. Part II. Zirconia-based dental ceramics. Dent Materials 2004; 20:449-456.
- Nakamura K, Mouhat M, Nergård JM, et al. Effect of cements on fracture resistance of monolithic zirconia crowns. Acta Biomaterial 2016; 2:12-19.
- Asai T, Kazama R, Fukushima M, et al. Effect of overglazed and polished surface finishes on the compressive fracture strength of machinable ceramic materials. Dent Material J 2010; 29:661-667.
- Shinchi M, Soma K, Nakabayashi N. The effect of phosphoric acid concentration on resin tag length and bond strength of a photo-cured resin to acid-etched enamel. Dent Material 2000; 16:324-329.
- Shimada Y, Tagami J. Effects of regional enamel and prism orientation on resin bonding. Oper Dent 2003; 28:20-27.
- Liu X, Jiang X, Xu T, et al. Investigating the shear bond strength of five resin-based luting agents to zirconia ceramics. J Oral Sci 2020; 62:84-88.
- Rosentritt M, Hmaidouch R, Behr M, et al. Fracture resistance of zirconia FPDs with adhesive bonding versus conventional cementation. Int J Prosthod 2011; 24.
- Weigl P, Sander A, Wu Y, et al. In-vitro performance and fracture strength of thin monolithic zirconia crowns. J Adv Prosthod 2018; 10:79-84.
- Maroulakos G, Thompson GA, Kontogiorgos ED. Effect of cement type on the clinical performance and complications of zirconia and lithium disilicate tooth-supported crowns: A systematic review. J Prosthet Dent 2019; 121:754-765.
- Zesewitz TF, Knauber AW, Nothdurft FP. Fracture resistance of a selection of full-contour all-ceramic crowns: An in vitro study. Int J Prosthodont 2014; 27:264-266.
- Mörmann WH, Bindl A, Lüthy H, et al. Effects of preparation and luting system on all-ceramic computer-generated crowns. Int J Prosthod 1998; 11.
- Bindl A, Lüthy H, Mörmann WH. Strength and fracture pattern of monolithic CAD/CAM-generated posterior crowns. Dent Materials 2006; 22:29-36.
Indexed at, Google Scholar, Cross Ref,
Indexed at, Google Scholar, Cross Ref,
Indexed at, Google Scholar, Cross Ref,
Indexed at, Google Scholar, Cross Ref,
Indexed at, Google Scholar, Cross Ref,
Indexed at, Google Scholar, Cross Ref,
Indexed at, Google Scholar, Cross Ref,
Indexed at, Google Scholar, Cross Ref,
Indexed at, Google Scholar, Cross Ref,
Indexed at, Google Scholar, Cross Ref,
Indexed at, Google Scholar, Cross Ref,
Indexed at, Google Scholar, Cross Ref,
Indexed at, Google Scholar, Cross Ref,
Indexed at, Google Scholar, Cross Ref,
Indexed at, Google Scholar, Cross Ref,
Indexed at, Google Scholar, Cross Ref,
Indexed at, Google Scholar, Cross Ref,
Indexed at, Google Scholar, Cross Ref,
Indexed at, Google Scholar, Cross Ref,
Indexed at, Google Scholar, Cross Ref,
Indexed at, Google Scholar, Cross Ref,
Author Info
1Department of Restorative and Esthetic Dentistry, College of Dentistry, University of Baghdad, Iraq
Received: 07-Mar-2022, Manuscript No. JRMDS-22-52365; , Pre QC No. JRMDS-22-52365 (PQ); Editor assigned: 09-Mar-2022, Pre QC No. JRMDS-22-52365 (PQ); Reviewed: 23-Mar-2022, QC No. JRMDS-22-52365; Revised: 28-Mar-2022, Manuscript No. JRMDS-22-52365 (R); Published: 04-Apr-2022
