Research - (2022) Volume 10, Issue 1
The Frequency of Inguinal Hernia in Relation to BMI at Altibri Medical College and Hospital: A Cross Sectional Study
Dharmoo Arija1, Ihsanullah Sial2, Rajesh Kumar3, Sadaf Jabeen2, Rekha Melwani2, Areeba Khan4 and Adnan Anwar5*
*Correspondence: Adnan Anwar, Hamdard College of Medicine and Dentistry, Pakistan, Email:
Abstract
Objective: Inguinal hernia is the most widespread hernia of abdominal wall. Hernia is a common condition affecting both men and women since time immemorial. The aim of the study is to determine the frequency of bilateral or unilateral inguinal hernias in normal and low Basal Metabolic Index (BMI). Methodology: This cross sectional study by using non-probability convenient sampling technique was carried out at Al-Tibri medical college and hospital, Karachi. The ethical approval for the study was taken from Institutional Research and Ethical Committee. An informed consent was taken from the patients and guardian. A total of 82 patients were selected for these studies in which78 were male and 4 were female. Inclusion criteria were based on the patient aged above 35 of either gender with complained of pain in groin region with clinical findings like swelling and tenderness, being an overweight and the labor that lifts heavy weight were also included in this study. However, the patient aged below 20 years with muscular pain in groin region without swelling were excluded from this study. Results: In a total of 82 patients diagnosed with inguinal hernia on clinical basis, the mean age was 45.95 ± 17.56 years. The mean height was 66.87 ± 3.77 inches. The mean weight was 61.90 ± 8.61 kgs. The mean BMI was 21.53 ± 2.56 kg/m2. Gender was male in 78(95.1%) and female in 4(4.9%). Diagnosis was right inguinal hernia in 34(41.5%), left inguinal hernia in 34(41.5%) and bilateral inguinal hernia in 14(17.1%). BMI was normal in 68(82.9%) and low in 14(17.1%). This indicated that in our study the patients with normal BMI were more likely to suffer from inguinal hernia as compared to the patients having low BMI. Conclusion: It was concluded in our study that the frequency of inguinal hernia (unilateral or bilateral) varies with the body mass index. Normal body mass index of male having a more chances of inguinal hernias than low body mass index. It was observed that the frequency of unilateral right inguinal hernia is more than bilateral. Similarly, males are more affected than females.
Keywords
Frequency, Inguinal hernia, Body mass index
Introduction
Amongst the abdominal wall hernias the most prevalent is inguinal wall hernia. Although 50% of the inguinal hernia patients were previously unaware of the condition, throughout the world one of the frequently carried out surgical procedure is the repair of inguinal hernia. Hernias of abdominal wall are often presented by an occurrence of 4% of cases who have ages of greater than 45 years and 1.7% of cases for all group of ages. Out of abdominal hernias 75% were reported as inguinal hernias and the risk within lifetime was approximately 3% in females and 27% in males [1]. Prevalence for Inguinal hernias (IHs) were very common around the world [2]. There is an unknown factual incidence of IH, however approximately 800,000 were diagnosed in the USA only, each year [3], and the requirement of inguinal hernia repair in men within his lifetime is predicted to be 1 out of each 2 [4]. Smoking, male gender, advanced age, elevated intraabdominal pressure, family history and connective tissue diseases [5] considered to be accountable to raise the chances of inguinal hernia [6].
Obesity was considered as a main threat for the IH development because it increases the intra-abdominal pressure that is correlated to increase in weight [7]. However, latest epidemiologic reports have observed the contradictory finding: elevated body mass index (BMI), while together with increased weight, is connected with decrease chances of acquiring of an IH as compared with normal weight individuals. Nevertheless, obesity is wellknown and recognized risk factor that raises the chances of recurrence of an IH [8]. It is essential to better understand and demarcate the association between body weight and the occurrence chances of IH, predominantly in countries like USA, where increased rate of obesity outbreak has turned into a central issue of health care [9].
Inguinal hernia exhibits a swelling at groin region which gets back to its normal position with minimum force while the patient is in lying down position. Slight discomfort is felt by the patient that increases with movement. Sometimes patients planned for surgery does not have pain, and intense pain is unusual (1.5% at rest and 10.2% on movement) [10]. Hernia is an outcropping of an organ through an abdominal aperture in the muscle wall of the cavity that surrounds it. It may be present at birth or because of failure of closure of various structures following birth or may acquire in later years because of overweight, weakness of muscles, surgery or some other illness. The most common sites in which hernia develops are the groin, umbilicus, linea Alba, semilunar line of spigelian, diaphragm and surgical incisions [11].
Inguinal hernias can develop at any age. Indirect hernias become visible before age 1 and often obvious before age 30; On the other hand, there appearance may become obvious later in life so far premature infants have an increase chance of developing an indirect inguinal hernia. A direct hernia, which usually occurs in male adults only, are much more common in older age because of deterioration of the muscles of the abdominal wall [12].
A person having a strong family history of inguinal hernia has more chances to develop inguinal hernias. Reports also propose that smoking has a great influence on inguinal hernia so people who smoke have greater risk of inguinal hernias [13].
Several factors are implicated during the development of inguinal hernia in which inheritance predominates. Other risk factors are prostatectomy, Ehlers-Danlos syndrome, severe constipation and low BMI, whereas it is still controversial that certain occupations have a strong impact on inguinal hernia formation [14]. For adult males, several risk factors suggesting the chances of inguinal hernia were reported. The chances of inguinal hernia development were about 8 times greater within cases having family history for inguinal hernia. Lifting heavy materials repeatedly for an extended period of time or actions demanding an immense constrain abruptly, chronic obstructive pulmonary disease or cough, increases the frequency of inguinal hernia [15,16]. In contrast, risk factors for adult females are umbilical hernia, chronic cough, tall, rural lifestyle, old age, constipation, family history, etc. [17]. The smoking and overweight are factors that rises the chances for occurrence of inguinal hernia [18]. The other risk factors that can increase the chances are inheritance, chronic constipation, chronic cough, cystic fibrosis, pregnancy, obese or overweight, premature birth, male gender, an earlier inguinal hernia and smoking [19,20]. Inguinal hernia is diagnosed clinically through physical examination. Furthermore, Radiological tests may consist of magnetic resonance imaging (MRI), ultrasound, computed tomography (CT) that have diagnostic effectiveness [21,22].
Hernia repair is classified into two primary subtypes: open surgery or laparoscopic surgery [23]. Both generally are performed on an outpatient basis and complete in about one hour. Open surgery is a usual method to repair most of the inguinal hernias and it is performed under general or local anesthesia according to the severity.
In laparoscopic hernia repair, a surgeon creates three minute incisions in the abdominal wall and then blow up the abdomen by a nontoxic gas. Insertion of laparoscope passes through the incisions by a surgeon [24]. The affiliation among the risk for inguinal hernia and body mass index (BMI) is still debatable. Therefore, to evaluate the frequency of inguinal hernia (IH) through different BMI categories was the goal for the study.
Method
The study design used was descriptive cross sectional study whereas sampling technique was convenient non probability sampling which had been conducted at Al- Tibri medical college and hospital, Karachi. The Institutional Research and Ethical Committee had provided the approval for the study .All the patients and guardian had given an informed consent. Around 82 patients in total were elected for this study.
Inclusion criteria have been set up on the patient aged over 35 of both genders had pain within the region of groin and other signs and symptoms present clinically e.g. tenderness with swelling, being an obese or manual laborers lifting weighty objects were as well incorporated within the study. But the patient aged below 20 years with muscular pain in groin region without swelling were removed from this study. Weight, height, BMI and age was recorded where BMI of <18.5 kg/m2 was considered as low while 18.5 to 24.9 was defined as normal.
Statistical Package for the Social Sciences (SPSS) version 20 (IBM Corporation, Armonk, NY, US) analyzed the data and presented in to table with calculated frequency and percentages as qualitative data while standard deviation and mean as quantitative data.
Results
Approximately 82 patients in total were diagnosed cases of inguinal hernia, the mean age had been 45.95 ± 17.56 years with the height of 66.87 ± 3.77 inches as a mean value. The weight was 61.90 ± 8.61 kgs as a mean vaule. The BMI was 21.53 ± 2.56 kg/m2 as a mean value. Gender was male in 78(95.1%) and female in 4(4.9%). Diagnosis was right inguinal hernia in 34(41.5%), inguinal hernia left sided in 34 (41.5%) and bilateral inguinal hernia in 14(17.1%). BMI had been normal in 68(82.9%) and low in 14(17.1%). Thus, it is indicated in our study that the patients along with normal BMI have had higher possibility of inguinal hernia in contrast to the patients having low BMI. (Table 1)
| Variables | Mean ± SD | ||
|---|---|---|---|
| N (%) | |||
| Age ( in Years) | 45.95 ± 17.56 | ||
| Height (Inches) | 66.87 ± 3.77 | ||
| Weight (Kg) | 61.90 ± 8.61 | ||
| BMI (kgm2) | 21.53 ± 2.56 | ||
| Gender | Females | 4 (4.9%) | |
| Males | 78 (95.1%) | ||
| Diagnosis | left Inguinal Hernia | 34(41.5%) | |
| Right Inguinal Hernia | 34(41.5%) | ||
| Bilateral Inguinal Hernia | 14(17.1%) | ||
| BMI | Normal | 68(82.9%) | |
| Low | 14(17.1%) |
Table 1: General outlines of the patients with inguinal hernia.
Gender was males in 32(94.1%) for left inguinal hernia (LIH) group, in 32(94.1%) for right inguinal hernia (RIH), and in 14(100.0%) in bilateral inguinal hernia (BIH) group. It was female in 2(5.9%) in right inguinal hernia (RIH) group, in 2(5.9%) in left inguinal hernia (LIH), and it was noted that bilateral inguinal hernia (BIH) was not found in females. (Table III) BMI had been normal in 26(76.5%) for left inguinal hernia (LIH) group, in 28(82.4%) for right inguinal hernia (RIH), and in 14(100.0%) in bilateral inguinal hernia (BIH) group. It was Low in 6(17.6%) in right inguinal hernia (RIH) group, in 8(23.5%) in left inguinal hernia (LIH), and not found in bilateral inguinal hernia (BIH) (Table 2 and Figure 1).
| Variables | Bilateral | Right | Left Inguinal | ||
|---|---|---|---|---|---|
| Inguinal Hernia n(%) | Inguinal Hernia n (%) | Hernia n (%) | |||
| BMI | Low | 0(0.00%) | 6(17.6%) | 8(23.5%) | |
| Normal | 14(100.0%) | 28(82.4%) | 26(76.5%) | ||
| Gender | Females | 0(0.00%) | 2(5.9%) | 2(5.9%) | |
| Males | 14(100.0%) | 32(94.1%) | 32(94.1%) |
Table 2: The incidence of variety of hernia over the basis of BMI and gender.
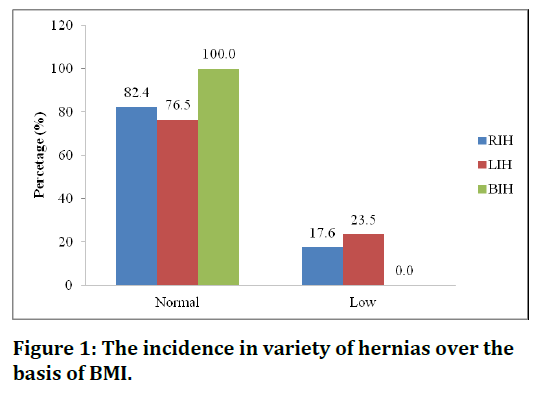
Figure 1. The incidence in variety of hernias over the basis of BMI.
Discussion
Abstractly, it is believed that obesity had been responsible for rise in the rate of inguinal hernia via increasing pressure insi de abdomen. Conversely, obese and overweight patients has shown lower chances of developing inguinal hernia within most of the reports [25], Rosemar et al. [26] had mentioned this, that for adult patients of inguinal hernia particularly males of age 44 to 55 years, the risk level is lowered by 4% , over raising 1 unit (3 to 4 kg) of BMI, and in contrast to patients with normal weight , the measure of risk for inguinal hernia development is lowered by 43%, in patients with obesity. Our study exhibits that the incidence of IH differs by BMI, with chances of inguinal hernia decreasing with low BMI on the contrary, patient with a normal BMI having increased incidence of inguinal hernia.
Some investigators concluded that patients who have higher weight, along with higher BMI, have a significant decrease in the development of IH throughout their lifetime [27].
Numerous probable justifications were hypothesized that explain for obesity as a “protective” aspect for the development of IH: Higher pre-peritoneal or intraabdominal fat might provide an obstruction by serving as a “plug” that put a stop to herniation of abdominal contents, however, the level and form of physical activity is a questionable risk factor in the development of an IH [28,29]. Furthermore, non-obese individuals are more active than obese individuals. In a study conducted via Reid et al. [30], the BMI was 27(19 to 38) as a median value , and cases who had weight as normal were 28%, whereas cases who had obesity or overweight were 72%. In this study of ours, the BMI was 21.53 ± 2.56 as a mean vaule and BMI was normal in 68(82.9%) patient but low in 14(17.1%) patients, so the incidence of inguinal hernia of right and left side found in patients of normal BMI rather than the low BMI. Similarly bilateral inguinal hernia are infrequent in females regardless of normal or low BMI but it is found that number of cases reported in males are low with normal BMI.
Gupta et al reported an occurrence of inguinal hernia in 96% of males in contrast to females whereas Charles reported 93.2% of the total cases were males [31]. Identical results have been concluded out of different parts of India [32]. In study of ours, males have been greatly affected than females that were consistent with several different literatures. The probable cause of greater incidence of inguinal hernia within males might be related to their involvement in strenuous activities as compared to females. It is also found in our study, the most predominant was primary hernia rather than recurrent hernia. It was also considered to be same in the other studies [33,34]. Majority of the cases in our study were bilateral hernia rather than unilateral hernia. Bilateral hernia had seen within 17% of the cases only. Charles moreover reported the most prominent type to be right sided hernia as compare to left side. But in our study, among the unilateral hernias, incidence of the left side was equal to the right side. Saeed have found 30% were left sided while 70% to be right sided and 59% were direct hernias and 46% were indirect inguinal hernias [35]. This was reported that, for right sided inguinal hernia, the incidence was 62.3% of total as compared to bilateral or left side. Same cases were reported by other workers too. Whereas, our study showed that unilateral of right and left side are equal and bilateral are less in number in comparison with unilateral with individual of normal BMI. A number of workers have projected that the late descend of the right testis could be the possible cause behind right sided dominance of the hernia [36,37].
Our study gives an insight about the probable mechanism involved in the reduction of IH risk for low weight and BMI or normal weight and BMI, as well as in obese patients but advance research is needed to test this hypothesis. However the study might not be immune from observer bias. Considering the finding of the above study and to what extent the BMI levels are associated with the inguinal hernia will be helpful to reveal further facts in future studies.
Conclusion
In was predicted in our study that the rate of inguinal hernia in normal BMI has been high with the involvement of either right or left side. Bilateral inguinal hernia also found within individual having normal BMI than low BMI individuals. But the frequency of bilateral is less than unilateral. Studies also reported that males are more affected than female in unilateral inguinal hernia than the bilateral inguinal hernia.
References
- Kingsnorth A, LeBlanc K. Hernias: Inguinal and incisional. Lancet 2003; 362:1561-71.
- Burcharth J, Pedersen M, Bisgaard T, et al. Nationwide prevalence of groin hernia repair. PloS one 2013; 8:e54367.
- Rutkow IM. Demographic and socioeconomic aspects of hernia repair in the United States in 2003. Surg Clin 2003; 83:1045-51.
- Zendejas B, Ramirez T, Jones T. Incidence of inguinal hernia repairs in olmsted county, MN: A Population-Based Study. Annals Surg 2013; 257:520–6.
- Lambert DM, Marceau S, Forse RA. Intra-abdominal pressure in the morbidly obese. Obesity Surg 2005; 15:1225–32.
- Zendejas B, Hernandez-Irizarry R, Ramirez T, et al. Relationship between body mass index and the incidence of inguinal hernia repairs: A population-based study in Olmsted County, MN. Hernia 2014; 18:283–8.
- Varela JE, Hinojosa M, Nguyen N. Correlations between intra-abdominal pressure and obesity-related co-morbidities. Surg Obes Relat Dis 2009; 5:524–8.
- Rosemar A, Angerås U, Rosengren A, et al. Effect of body mass index on groin hernia surgery. Annals Surg 2010; 252:397-401.
- Wang Y, Beydoun MA. The obesity epidemic in the United States—gender, age, socioeconomic, racial/ethnic, and geographic characteristics: A systematic review and meta-regression analysis. Epidemiol Rev 2007; 29:6-28.
- Page B, Paterson C, Young D, et al. Pain from primary inguinal hernia and the effect of repair on pain. J Br Surg 2002; 89:1315-8.
- Chow A., Athanasiou T, Tekkis P, et al. Inguinal hernia. BMJ Clin Evi 2007; 9:1-20.
- Quintas ML, Rodrigues CJ, Jin HY, et al. Age related changes in the elastic fiber system of the interfoveolar ligament. Rev Hospital Clín 2000; 55:83-6.
- Simons MP, Aufenacker T, Bay-Nielsen M, et al. European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 2009; 13:343-403.
- Vad MV, Frost P, Bay-Nielsen M, et al. Impact of occupational mechanical exposures on risk of lateral and medial inguinal hernia requiring surgical repair. Occup Environ Med 2012; 69:802-9.
- Lau H, Fang C, Yuen WK, et al. Risk factors for inguinal hernia in adult males: A case-control study. Surg 2007; 141:262-6.
- Flich J, Alfonso JL, Delgado F, et al. Inguinal hernia and certain risk factors. Eur J Epidemiology 1992; 8:277-82.
- Sanjay P, Woodward A. Single strenuous event: Does it predispose to inguinal herniation? Hernia 2007; 11:493-6.
- Sultan B, Quresh Z, Malik MA. Frequency of external hernias in Ayub teaching hospital Abbottabad. J Ayub Med College Abbottabad 2009; 21:57-8.
- Oberg S, Andresen K, Rosenberg J. Etiology of inguinal hernias: A comprehensive review. Frontiers Surg 2017; 4:52.
- Sorensen LT, Friis E, Jorgensen T, et al. Smoking is a risk factor for recurrence of groin hernia. World J Surg 2002; 26:397.
- Burkhardt JH, Arshanskiy Y, Munson JL, et al. Diagnosis of inguinal region hernias with axial CT: The lateral crescent sign and other key findings. Radiograph 2011; 31:e1-2.
- Zoga AC, Mullens FE, Meyers WC. The spectrum of MR imaging in athletic pubalgia. Radiol Clin 2010; 48:1179-97.
- Kingsnorth A. Treating inguinal hernias. Br Med J 2004; 328:59-60.
- McCormack K, Wake B, Perez J, et al. Laparoscopic surgery for inguinal hernia repair: Systematic review of effectiveness and economic evaluation. Health Technol Assessment 2005; 9:1-203.
- Ruhl CE, Everhart JE. Risk factors for inguinal hernia among adults in the US population. A m J Epidemiology 2007; 165:1154-61.
- Rosemar A, Angerås U, Rosengren A. Body mass index and groin hernia: A 34-year follow-up study in Swedish men. Ann Surg 2008; 247:1064-8.
- Lilja M, Eliasson M, Stegmayr B, et al. Trends in obesity and its distribution: Data from the Northern Sweden MONICA survey, 1986–2004. Obesity 2008; 16:1120–8.
- Carbonell JF, Sanchez JL, Peris RT, et al. Risk factors associated with inguinal hernias: A case control study. Eur J Surg 1993; 159:481–6.
- Zendejas B, Ramirez T, Jones T, et al. Trends in the utilization of inguinal hernia repair techniques: A population-based study. Am J Surg 2012; 203:1–5.
- Reid TD, Sanjay P, Woodward A. Local anesthetic hernia repair in overweight and obese patients. World J Surg 2009; 33:138-41.
- Charles NR. A two year retrospective study of congenital inguinal hernia at western regional hospital, Nepal. J Nep Med Assoc 2000; 39:172-5.
- Balram. Prevalence of inguinal hernia in Bundelkhand region of India. Ann Int Med Den Res 2016; 2:137-8.
- Sayanna S. Prevalence of inguinal hernia in Indian population a retrospective study. Int Med J 2015; 2:75-8.
- Gulzar MR, Iqbal J, Ulhaq MI, et al. Darning vs bassini repair for inguinal hernia: A prospective comparative study. Professional Med J 2007; 14:128-33.
- Saeed BBA. Inguinal hernia repair by darning. Yemen Journal Med Sci 2009; 1:1-5.
- Sangwan M, Sangwan V, Garg M, et al. Abdominal wall hernia in a rural population in India: Is spectrum changing? Open J Epidemiol 2013; 3:135-8.
- Mbah N. Morbidity and mortality associated with inguinal hernia in northwestern Nigeria. West African J Med 2007; 2.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Dharmoo Arija1, Ihsanullah Sial2, Rajesh Kumar3, Sadaf Jabeen2, Rekha Melwani2, Areeba Khan4 and Adnan Anwar5*
1Ghulam Muhammad Mahar Medical College, Sukkur, Pakistan2Altibri Medical College and Hospital, Pakistan
3Jinnah Post Graduate Medical Center, Pakistan
4Ziauddin College of Rehabilitation Sciences, Ziauddin University, Karachi, Pakistan
5Hamdard College of Medicine and Dentistry, Pakistan
Citation: Dharmoo Arija, Ihsanullah Sial, Rajesh Kumar, Sadaf Melwani, Rekha Melwani, Areeba Khan, Adnan Anwar, The Frequency of Inguinal Hernia in Relation to BMI at Altibri Medical College and Hospital: A Cross Sectional Study, J Res Med Dent Sci, 2022, 10(1): 482-486
Received: 17-Dec-2021, Manuscript No. JRMDS-22-49851; , Pre QC No. JRMDS-22-49851 (PQ); Editor assigned: 20-Dec-2021, Pre QC No. JRMDS-22-49851 (PQ); Reviewed: 03-Jan-2022, QC No. JRMDS-22-49851; Revised: 06-Jan-2022, Manuscript No. JRMDS-22-49851 (R); Published: 13-Jan-2022
