Review - (2021) Volume 9, Issue 7
The Use of Biological Agents in External Sinus Lifting Procedures: A Systematic Review
Razan Alaqeely* and Najla AlMuayli
*Correspondence: Razan Alaqeely, Department of Periodontics, King saud university, Saudi Arabia, Email:
Abstract
Background: Biological agents are growth factors that aid in bone regeneration and increase healing potential. They are used to compensate for the shortcomings associated with bone grafts. Aim: The aim of this systematic analysis was to assess the effects of combining different biological agents with different types of bone grafts in lateral maxillary sinus lifting. The assessment considers newly formed bone, augmented bone height, soft tissue healing and post-operative complications. Methodology: Three electronic databases were searched, and manual searching was performed for relevant articles published before 2020. All relevant articles were independently screened for specific inclusion criteria. Primary outcomes were bone formation, soft tissue healing, and the percentage of remaining graft particles. Secondary outcomes were clinical findings and complications, survival, and success of implant. Result: Eight randomized clinical trials met the inclusion criteria. No statistically significant difference was found between different bone graft types. A borderline statistical difference was observed between Xenograft. Conclusion: There was no statistical or clinical difference between different biological agents that were combined with bone grafts when performing lateral sinus lifting procedures. The use of biological agents might be beneficial in short-term healing and in promoting bone regeneration.
Keywords
Sinus lifting, Biological agents, Growth factors, External sinus augmentation
Introduction
Post extraction of maxillary molars causes a proliferation of osteoclast activity in the Schneiderian membrane, leading to rapid sinus pneumatization [1]. The use of dental implants in posterior maxilla, as the gold standard treatment, is complicated by a rapid and large amount of vertical bone loss. Lateral sinus augmentation is one of the most highly predictable surgical approaches for the treatment of severely atrophic maxillary process [2,3].
In order to encourage predictable and acceptable quantities, and consistency, of regenerated tissue, the application of grafting materials, barrier membranes and/or biological agents must be carefully chosen [4]. Different bone grafting materials have been used in sinus augmentation to encourage new natural bone formation with capillary infiltration and support the implant with sufficient bone volume. Autogenous bone has osteogenesis, osteoinduction and osteoconduction capabilities, in addition to also containing growth factors. However, rapid resorption of the bone graft ,at gained height and width, is considered a major issue with autogenous bone [5].
Bone substitutes in the form of xenografts, allografts, and alloplasts have also been used; however, they also have their associated limitations such as inconvenience, cost, and delayed healing [5,6]. The use of bone alone as a scaffold typically fails to generate sufficient osteogenic induction and conduction for regeneration and the reconstruction of lost sinus height.
Biological agents comprise various growth factors present in natural bone that are known to aid in bone regeneration and increase healing potential [7]. They are used to compensate for disadvantages of bone grafts by mimicking the presence of important factors.
A range of widely studied growth factors [e.g., PDGF, PRP, PRF] are released by blood platelets. Research and clinical experience has highlighted the potential of these growth factors in improving periodontal regeneration, demonstrating greater bone formation, reduced healing times, and an improvement in the regeneration process [8,9].
Another biological agent, enamel matrix derivative (EMD), consists of various proteins related to enamel, mainly amelogenin (90%), and shows an improvement in regeneration potential.
Bone morphogenic proteins (BMPs) are members of the transforming growth factor-beta (TGF-β) superfamily, and play an important role in the generation of high osteo-inductive potential and increasing the expression of mineral tissue markers [4]. Some other agents, such as hyaluronic acid (HA)–a major component of the extracellular matrix in natural carbohydrates–has also been proposed to play an important role in the healing of periodontal wounds [10].
The aim of this systematic analysis was to assess the effects of various biological agents (including fibrin glue, platelet rich fibrin (PRF), rh-PDGF, EMD, HA, and BMPs) in addition to different types of bone grafts in lateral maxillary sinus lifting. The assessment considers newly formed bone, augmented bone height, soft tissue healing and post-operative complications.
The PICO was as follows
Population (P): Systematically healthy patients requiring bilateral maxillary sinus augmentation.
Intervention (I): Treated with bone graft combined with biological agents on one side and bone graft alone on the contralateral side.
Comparison (C): Grafting material with and without biological agents.
Outcomes (O): Newly formed bone, augmented bone height, soft tissue healing and post-operative complications implant stability and implant survival.
Materials and Methods
We conducted a thorough search of the literature using the electronic databases MEDLINE, EMBASE, and the Cochrane Central Register for Controlled Trials.
Selection criteria
Studies in which patients were treated with a maxillary sinus floor elevation with bone graft and additional biological material (or growth factor) were searched for.
Inclusion criteria
- Randomized clinical trials (RCTs) or clinical trials (CTs) or studies with a minimum follow-up period of six months or more.
- Surgical regenerative interventions using biological agents (fibrin glue, platelet rich fibrin, platelet rich plasma growth factors (rh-PDGF), enamel matrix derivative (EMD), hyaluronic acid (HA), and bone morphogenic proteins (BMPs) in addition to bone graft.
- Sites undergoing bilateral lateral maxillary sinus augmentation without simultaneous implant placement.
- Comparative studies assessing histological, histomorphometric, clinical, and radiographic outcomes.
- Human adults with good general health status.
- Non-smokers.
- English speakers.
Exclusion criteria
- Non-adult patients.
- Patients with any systemic disease.
- Unilateral sinus lifting.
- Patients with aggressive periodontitis.
- Smokers.
- Studies on regeneration of periodontal intrabony and furcation defects.
- Studies with inclusion of a total of less than five patients in the final analysis.
- Prospective and retrospective cohort studies and case series.
- In vitro studies.
- Preclinical (animal) studies.
Search strategy
The search strategy used was a combination of MeSH terms and free text words.
‘Maxillary sinus lift’ [MeSH] OR (sinus augmentation) OR (sinus floor elevation) OR (maxillary sinus lift) OR (sinus graft) AND ‘(“Platelet rich fibrin” OR “platelet rich plasma” OR “PRP” OR “PRF” OR “PRGF” OR “growth factor” OR “Hyaluronic acid” OR “HA” OR “bone morphogenic proteins” OR “BMP” OR “fibrin glue” OR “Enamel Matrix Derivative “OR “EMD” OR “PDGF” OR “platelet derived growth factor” OR “PDGF”).
The references of eligible studies were checked. Titles and abstracts were assessed independently by two examiners. Cohen’s Kappa score was used to assess interreviewer agreement of selection process [11]. Full-text documents were obtained and manual searches of the bibliographies of the full-text articles were also performed. Disagreements were resolved by discussion and consensus was reached.
Data extraction
Pre-designed extraction forms were developed to assess the following data: author name(s), publication year and place, study design, sample size, follow-up period, selection and description of the study population, definition and measurement method of the intervention, controls, outcomes, results and their variation, and risk of bias.
Data synthesis
Data synthesis was performed by organizing data in an evidence table and a descriptive summary was created to determine study characteristics (Table 1). Primary outcomes were the percentage of newly formed bone, percentage of residual-bone substitute material, and percentage of soft tissue area assessed by histomorphometric analysis. Furthermore, augmented bone height (mm) was assessed by radiographic evaluation and clinical outcomes in terms of implant stability, implant survival, and postoperative complications.
Table 1: Characteristics of included studies arranged by year.
| Author/year | Patients (n) | Mean age | Bone graft | Biological agent | Outcome measures |
|---|---|---|---|---|---|
| Bettega et al. 2009 [19] | 18 | 50.5 | Iliac crest graft (cancellous bone) | Autologous platelet concentrate (APC), biological glue | Histological and radiographic analysis |
| Yilmaz et al. 2013 [16] | 10 | 56.9± 5.95 | Bovine-derived xenograft (BDX) | Platelet rich plasma (PRP) | Radiographic and histological analysis |
| Froum et al. 2013 [13] | 12 | 61.2±7.7 | Anorganic bovine bone matrix (ABBM) | Recombinant human platelet derived growth factor (hPDGF) | Histomorphometric analysis |
| Taschieri et al. 2015 [15] | 6 | 59.5 | Deproteinized bovine bone | Platelet rich plasma (PRP) | Histological and Histomorphometric analysis |
| Nizam et al. 2017 [14] | 13 | 49.92 ± 10.37 | Deproteinized bovine bone | Leukocyte and platelet rich fibrin (L-PRF) | Histological and radiographic analysis |
| Nery et al. 2017 [17] | 10 | 55 | Biphasic calcium phosphate (B-TCP) | Enamel matrix proteins derivatives (EMD) | Histological and Histomorphometric analysis |
| Mourão et al. 2018 [18] | 10 | 56.5 | Nanostructured carbonated hydroxyapatite (cHA) | Blood-derived growth factors (BDGF) | Radiographic analysis |
| Adalı et al. 2020 [20] | 10 | 57 | Allograft | Concentrated growth factor (CGF) | Histomorphometric and radiographical analysis |
Table 2: Main results.
| Author/year | Histomorphometry | Radiographic | Clinical | ||||
|---|---|---|---|---|---|---|---|
| Vital bone | Residual graft | Soft tissue | Bone height (pre) | Bone height (post) | Complications | Implant survival | |
| Bettega et al. 2009 [19] | C:42.5% | NM | NM | 3 (1.75-6.25) | 10.5(8.5-16.25) | NM | NM |
| T: 37.1% | 3.5 (2-5.25) | 11.5 (9.5-16) | |||||
| Yilmaz et al.2013 | NM | NM | NM | C:3.13+1.05 | C:12.76+1.93 | 5 small perforations (<5mm); 3 in test and 2 in control. All sealed with collagen membrane. | NM |
| T:3.2+0.68 | T:12.77+2.45 | ||||||
| Froum et al. 2013 [13] | C:21.4+8.6 | C:40.3+6.7 | C:45.96+8.36 | NM | NM | NM | NM |
| T: 19.5+10.7 | T: 35.5+9.4 | T:52.12.53 | |||||
| Taschieri et al. 2015 [15] | C: 22.72+9.21 | NM | NM | 2.4+1.08 | NM | Less swelling and hematoma in the test side. | 100% survival after 1 year |
| T: 30.7 + 7.89 | 2.8+1.04 | ||||||
| Nizam et al. 2017 [14] | C: 21.25+5.59 | C: 32.79+5.89 | C:38.4+6.6 | 2.53+0.61 | 13.53+1.2 | 1 patient had excessive bleeding in both sides. | 100% survival after 1 year |
| T:21.38+8.78 | T: 25.95+9.54 | T:44.2+10.4 | 2.45+0.79 | 13.6+1.09 | |||
| Nery et al. 2017 [17] | C:43.3+6.1 | C:35.3+9 | C:21.3+6.8 | NM | NM | NM | NM |
| T:43+9 | T: 35.5+8.2 | T:21.5+5.3 | |||||
| Mourão et al. 2018 [18] | NM | NM | NM | Measuring panoramic and CT: P>0.05 | NM | NM | NM |
| Adalı et al. 2020 [20] | C:35.49% | C;5.1 | NM | NM | NM | 2 (<2mm) perforations; 1 in each group. | 100% survival after 1 year |
| T: 36.41% | T:5.8 | ||||||
NM: Not Mentioned, C: Control group, T: Test group
Risk of bias in individual studies
Critical appraisal for potential risk of bias was done by the Cochrane Collaboration’s tool for assessing risk of bias [12]. Studies were classified as either “low risk”, “unclear risk”, and “high risk” of bias.
Results
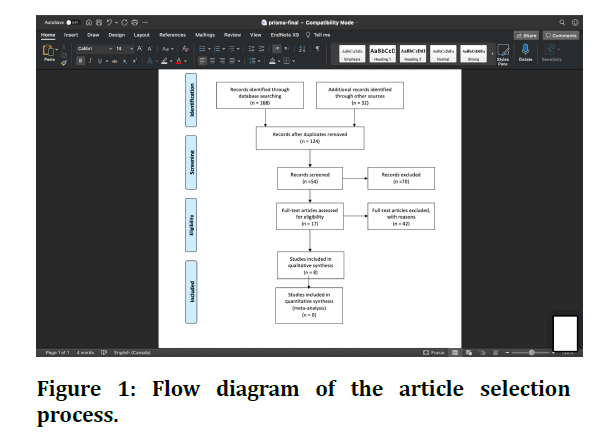
A flowchart of article selection is shown in Figure 1. The PubMed and Cochrane search resulted in 200 studies. After assessing titles and abstracts, 146 studies were excluded. Thirteen studies were eligible after full-text assessment.
Figure 1: Flow diagram of the article selection process.
However, five studies were excluded in this step: one study did not have a control group, and the remaining four studies did not include a bilateral comparison. The manual search did not reveal additional studies to be included (Table 1). The k-value for inter-reviewer agreement on the methodological appraisal was 0.8.
Study design and patient features
The articles included in this study were published in the period from 2009 to 2020 with a total of 178 sinus lift procedures performed in eight studies. Different treatment modalities including the bone graft type and biological agent added are shown in Table 1. Substantial heterogeneity existed regarding patient populations, bone graft material, and outcome measures. The age of the participants ranged from 40 to 68 years. Four studies compared xenograft alone to xenograft mixed with platelet concentrates [13-16], two studies compared alloplastic bone materials with EMD [17] and one study included blood-derived growth factors (BDGF) [18]. Autologous platelet concentrate was used with autogenous bone in one study [19]. The final study included a comparison of allograft alone versus allograft mixed with concentrated growth factor (CGF) [20].
Medications prescribed and post-operative management
Pre-operative prescriptions were discussed in five studies, including prophylactic antibiotics administered one hour prior to surgical intervention [13-15,17,18]. Post-operative care and medication were given in all studies except in the Bettega, et al. [19] study. Detailed post-operative care was mentioned in two studies [15,18]. Dexamethasone (4mg) was prescribed in one study for a period of three days [18].
Outcomes measured
Table 2 summarizes the reported similar outcome measures (i.e., percentage of new bone formation, residual graft etc.) according to data presented in each study.
Risk of bias assessment
The results of the bias assessment of the included studies are presented in Figure 2. Robvis was used to create the plot [21]. No studies obtained the highest score in the quality analysis. Two studies reported adherence to the CONSORT statement recommendations [15,18].
Discussion
The present systematic review focused on RCTs of external sinus lifting using different biological agents. The aim of this review was to evaluate the literature on combining various biological agents in lateral sinus lifting in regard to effect on bone regeneration, soft tissue healing, and amount of bone gained prior to implant placement.
The selected publications revealed heterogeneous conclusions, due to low power and incomplete recording of the data. Thus, no meta-analysis could be performed.
The addition of biological agents to bone grafts was found to overcome the limitations of using bone graft alone [22]. The stimulation of bone augmentation decreased healing time, and stabilization of gained bone height were found to be the results of adjunct use of the biological agents [5,23,24].
Under the criteria of this study, eight RCTs were eligible for final analysis. Despite the different bone graft materials used, the studies evaluated the effect of sole bone grafting in comparison to the addition of a biological agent. Since a variety of biological materials were collected, and to simplify the findings, we interpreted the results in accordance with the bone graft material used:
Autogenous bone graft
One study [19] used a combination of cancellous bone of iliac crest with autologous platelet concentrate (APC) (test group) compared to bone alone in 18 patients (control group). The mature vital bone structure reached 37.1% in the test group compared to 42.5% in control group with no significant difference. Radiographic bone height was not significantly different between the two groups. The one significant difference found was that less bone was needed to fill the sinus in the test group.
Alloplast bone graft
One study used hydroxyapatite in combination with BDGF [18]. BDGF proved to be efficacious, even when used with immediate implant placement without grafting material. However, this RCT found that BDGF had no additional effect on bone volume. The type of bone graft used in this study (nanostructured carbonated hydroxyapatite microspheres) might have also contributed to the results, as it’s claimed to promote formation of bone [25]. Another study used enamel matrix proteins added to β-tri-calcium-phosphate with hydroxyapatite bone ceramic [17]. No additional effect was found in histological analysis, which indicated that both groups had successful implant installation.
Allograft
One study in this category used demineralized allograft mixed with CGF (20). CGF has previously been shown to improve regenerative capacity as it is comprised of a mixture of growth factors. The results demonstrated that using CGF with allografts supports the stabilization of gained vertical bone height after sinus augmentation, even though no histological or radiographical differences were reported.
Xenograft
Other studies used xenografts mixed with plateletderived agents. The preparation techniques of platelets influence the released types of growth factors. Several generations of platelet concentration preparations, which were initially used to generate material to improve wound healing [26], were followed by PRP and PRGF isolation techniques in the late nineties. The development of the Choukroun technique facilitated and improved the use of platelet concentrates [27]. The newest generation of platelet includes L-PRF and PRFF, which have more favorable mechanical properties and results in a constant release of growth factors, improved bone formation and osseointegration [28].
In this analysis, four papers used bovine bone with PRP, PDGF and L-PRF. The first study, performed in Turkey, used PRP with a bovine-derived xenograft. This resulted in a satisfactory bone height, in addition to more prominent and mature bone formation observed at sites treated with the combination [16]. In another study, anorganic bovine bone matrix was used in combination with rhPDGF [13]. The effect of this combination was found to be strong within the first six months of treatment, but this effect dissipated in the long-term. The study concluded that more rapid formation of vital bone with the addition of rhPDGF may allow for earlier implant placement. A further study [15] utilized PRP and deproteinized bovine bone matrix. The addition of pure PRP to deproteinized bovine bone mineral enhanced vital bone formation in the first six months of healing. The final study mixed L-PRF with bovine bone and found no significant difference in comparison to bone graft alone [14].
Although there were discrepancies in sample size, technique used, and materials used in the collected articles, the strict criteria of having at least six months of healing might have affected the findings. The healing period used in these studies might have masked the effect of biological agents in promoting healing and bone maturation. Due to the variation in study design and measured outcomes between studies, the results are inconclusive.
Another important consideration in the context of this procedure is the maintenance of sinus height after sinus lifting procedures. In the above-mentioned studies, only one took this factor into consideration where sinus height was measured immediately after grafting and before implant placement six months later [20].
The clinical implication of combining biological agents with bone graft material seems promising; however, extensive studies focusing on the best healing period before placing the implant, the preservation of sinus height, and long-term survival and success of implants placed in lifted sinuses with the addition of biological agents are recommended.
Conclusion
In conclusion, this systemic review offers an insight into the effects of various biological agents combined with different types of bone grafts in lateral maxillary sinus lifting procedures. While the findings presented in this review are not conclusive.
References
- Corinaldesi G, Piersanti L, Piattelli A, et al. Augmentation of the floor of the maxillary sinus with recombinant human bone morphogenetic protein-7: A pilot radiological and histological study in humans. Br J Oral Maxillofac Surg 2013; 51:247-52.
- Choukroun J, Diss A Fau-Simonpieri A, Simonpieri A Fau, et al. Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part V: Histologic evaluations of PRF effects on bone allograft maturation in sinus lift. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006; 101:299-303.
- Kim MS, Lee JS, Shin HK, et al. Prospective randomized, controlled trial of sinus grafting using Escherichia-coli-produced rhBMP-2 with a biphasic calcium phosphate carrier compared to deproteinized bovine bone. Clin Oral Implants Res 2015; 26:1361-8.
- Suárez-López Del Amo F, Monje A, Padial-Molina M, et al. Biologic agents for periodontal regeneration and implant site development. Biomed Res Int 2015; 957518.
- Starch-Jensen T, Mordenfeld A, Becktor JP, et al. Maxillary sinus floor augmentation with synthetic bone substitutes compared with other grafting materials: A systematic review and meta-analysis. Implant Dent 2018; 3:363-374.
- Boyne PJ, Lilly LC, Marx RE, et al. De novo bone induction by recombinant human bone morphogenetic protein-2 (rhBMP-2) in maxillary sinus floor augmentation. J Oral Maxillofac Surg 2005; 63:1693-707.
- Khairy NM, Shendy EE, Askar NA, et al. Effect of platelet rich plasma on bone regeneration in maxillary sinus augmentation (randomized clinical trial). Int J Oral Maxillofac Surg 2013; 42:249-55.
- Liu R, Yan M, Chen S, et al. Effectiveness of platelet-rich fibrin as an adjunctive material to bone graft in maxillary sinus augmentation: A meta-analysis of randomized controlled trails. Biomed Res Int 2019; 2019:7267062.
- Miron RJ, Zucchelli G, Pikos MA, et al. Use of platelet-rich fibrin in regenerative dentistry: a systematic review. Clin Oral Investig 2017; 21:1913-27.
- Eliezer M, Imber JC, Sculean A, et al. Hyaluronic acid as adjunctive to non-surgical and surgical periodontal therapy: A systematic review and meta-analysis. Clin Oral Investig 2019; 23:3423-35.
- Cohen J. Weighted kappa: Nominal scale agreement with provision for scaled disagreement or partial credit. Psychol Bull 1968; 70:213-20.
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLOS Med 2009; 6:e1000097.
- Froum SJ, Wallace S, Fau-Cho SC, et al. A histomorphometric comparison of bio-oss alone versus bio-oss and platelet-derived growth factor for sinus augmentation: A postsurgical assessment. Int J Periodontics Restorative Dent 2013; 33:269-79.
- Nizam N, Eren G, Akcalı AAO, et al. Maxillary sinus augmentation with leukocyte and platelet-rich fibrin and deproteinized bovine bone mineral: A split-mouth histological and histomorphometric study. Clin Oral Implants Res 2017; 29:67-75.
- Taschieri S, Testori T Fau, Corbella S, et al. Platelet rich plasma and deproteinized bovine bone matrix in maxillary sinus lift surgery: A split-mouth histomorphometric evaluation. Implant Dent 2015; 24:592-7.
- Yilmaz S, Karaca Eo Fau, Ipci SD, et al. Radiographic and histologic evaluation of platelet-rich plasma and bovine-derived xenograft combination in bilateral sinus augmentation procedure. Platelets 2013; 24:308-15.
- Nery JC, Pereira L, Guimarães GF, et al. β-TCP/HA with or without enamel matrix proteins for maxillary sinus floor augmentation: A histomorphometric analysis of human biopsies. Int J Implant Dent 2017; 3:18.
- Mourão CFAB, Lourenço ES, Nascimento JRB, et al. Does the association of blood-derived growth factors to nanostructured carbonated hydroxyapatite contributes to the maxillary sinus floor elevation? A randomized clinical trial. Clin Oral Investig 2018; 23:369-79.
- Bettega G, Brun Jp Fau, Boutonnat J, et al. Autologous platelet concentrates for bone graft enhancement in sinus lift procedure. Transfusion 2009; 49:779-85.
- Adalı E, Yüce MO, Günbay T, et al. Does concentrated growth factor used with allografts in maxillary sinus lifting have adjunctive benefits? J Oral Maxillofac Surg 2020; 79:98-108.
- McGuinness LA, Higgins JPT. risk-of-bias visualization (robvis): An R package and shiny web app for visualizing risk-of-bias assessments. Res Synthesis Methods 2020.
- Browaeys H, Bouvry P, De Bruyn H. A literature review on biomaterials in sinus augmentation procedures. Clin Implant Dent Relat Res 2007; 9:166-77.
- Molemans B, Cortellini S, Jacobs R, et al. Simultaneous sinus floor elevation and implant placement using leukocyte- and platelet-rich fibrin as a sole graft material. Int J Oral Maxillofac Implants 2019; 34:1195–201.
- Pichotano EC, de Molon RS, de Souza RV, et al. Evaluation of L-PRF combined with deproteinized bovine bone mineral for early implant placement after maxillary sinus augmentation: A randomized clinical trial. Clin Implant Dent Relat Res 2019; 21:253-62.
- Shanbhag SF, Shanbhag V, Stavropoulos A. Volume changes of maxillary sinus augmentations over time: A systematic review. Int J Oral Maxillofac Implants 2014; 29:881-92.
- Matras H. Effect of various fibrin preparations on reimplantations in the rat skin. Osterr Z Stomatol 1970; 67:338-59.
- Choukroun J, Adda F, Schoeffer C, et al. An opportunity in perio implantology. Implantodontie 2000; 42:55-62.
- Dohan EDM, Andia I, Zumstein MA, et al. Classification of platelet concentrates (Platelet-Rich Plasma-PRP, Platelet-Rich Fibrin-PRF) for topical and infiltrative use in orthopedic and sports medicine: Current consensus, clinical implications and perspectives. Muscles Ligaments Tendons J 2014; 4:3-9.
Author Info
Razan Alaqeely* and Najla AlMuayli
Department of Periodontics, King saud university, Saudi ArabiaCitation: Razan Alaqeely, Najla AlMuayli,The Use of Biological Agents in External Sinus Lifting Procedures: A Systematic Review, J Res Med Dent Sci, 2021, 9(7): 160-165
Received: 13-Jun-2021 Accepted: 09-Jul-2021