Research - (2022) Volume 10, Issue 6
Therapeutic Efficacy & Long-term Treatment Outcome of DPP-4 Inhibitors as an add-on Therapy with Metformin and Sulfonylureas in T2DM Patients at GP Clinics of Southern Odisha
Premakanta Mohanty1, Chinmaya Debasis Panda2 and Pradyut Kumar Pradhan3
Abstract
Introduction: Diabetes is a global health concern with T2DM being the most common type. Medical science has hardly been successful in managing this condition and its associated co-morbidities and complications. Most interestingly although it’s a condition primarily referred to super specialists, it has to be primarily managed by general practioners in primary healthcare setups. GPs face many problems in diabetes management, one of which is non-availability of a universal treatment guideline applicable to all patients. Hence to evaluate individual newer drugs like DPP-4 inhibitors for their efficacy, safety and long-term treatment outcome, this study was conducted. Aim and objective: To provide evidence about the therapeutic efficacy and long-term treatment outcomes in T2DM patients treated with DPP-4 inhibitors as an add-on therapy with metformin and sulfonylureas. Methodology: A sample of 153 T2DM patients with disease duration of around 5 years was selected who were being treated in GP clinics of southern Odisha. Among them around 74 patients were isolated who were taking either a combination of metformin and sulfonylureas (Group-A) or metformin, sulfonylureas and DPP-4 inhibitors (Group-B). Patient past data like their demography, blood glucose level, HBA1C level etc. were collected from their personal treatment files using a structured case record form and was statically evaluated to extract the efficacy with complication and co-morbidity outcomes in patients with and without DPP-4 inhibitors in their treatment regimen. Discussion and conclusion: In our study it was found that DPP-4 Inhibitors significantly improved glycemic outcome (OR, 2.862; 95% CI, 1.349-6.069) as compared to the control group (OR, 0.845; 95% CI, 0.299-2.385). Treatment group had shown relatively better blood pressure control (OR, 0.997; 95% CI, 0.487-2.043) than control group (OR, 0.114; 95% CI, 0.025-0.529). No statistically significant relationship could be established between DPP-4 Inhibitors and any of the chronic complications of T2DM. Further studies are needed to evaluate and establish the findings of our study.
Keywords
T2DM, GP clinics, Odisha, Global health
Introduction
Type 2 diabetes mellitus is a multisystem, heterogeneous, polygenic, multi-factorial and progressive chronic disease associated with multiple complications [1,2] Approximately 463 million adults aged between 20–79 year are diagnosed with type-2 diabetes worldwide which is around 9.3% of the world’s population [3] Unfortunately this number hardly shows real burden of the disease as many more are having either T2DM but undiagnosed, or are pre-diabetic and the numbers are only going to escalate further in future.
Traditionally the management of T2DM has been more focused on good glycemic control, while the real challenge has always been prevention of complications and improvement of standard of living. Although both appear to be closely related but not necessarily are the same thing. Due to some recent research breakthroughs, the approach is gradually changing [4,5], majority of newer guidelines are advising considerations of patient factors like cardiovascular risk factors, risk of chronic kidney disease, heart failure, risk of hypoglycemia, body weight, adverse effects and cost of management, preferences of patient etc. along with efficacy for glycemic control while choosing appropriate treatment regimen [4]. But unfortunately we do not have enough data to classify the anti-diabetic drugs as per their efficacy in preventing/promoting or being neutral for complications progression and co-morbidity outcomes. Once such database will be developed, it would be far easier to choose individualized treatment modalities for T2DM management which not only will result in good glycemic control but also would result in far lesser complications and better outcomes in co-morbidities. It can also help in developing treatment guidelines and flowcharts which will be of immense help for clinicians, more so for the general practitioners who are now dealing with vast majority of the patients at grass root levels.
Usual first line of treatment for type 2 diabetes management is metformin as not only an individual initial drug but also as a co-therapy with other antidiabetic drugs including insulin. Primary benefits of this drug are its high efficacy, safety, affordability, cardiovascular protectiveness, weight loss etc. [6]. There are few adverse effects associated with metformin such as gastro intestinal intolerance, diarrhea, bloating etc which can be easily tackled by gradual dose titration. But the primary concerns in patients treated with metformin are possibility of lactic acidosis specifically when associated with reduced eGFR and worsening of neuropathy due to associated vitamin B-12 deficiency [7–10].
In most of the cases of type 2 diabetes mellitus, a stepwise addition of other drugs is needed to achieve target HBA1C level after around 3 months of metformin monotherapy trial when any of the drug classes from sulfonylurea, thiazolidinedione, DPP-4 inhibitor, SGLT2 inhibitor,GLP-1 RA, or basal insulin can be added depending on patient factors such as existing cardiovascular risk, safety, expense etc. (11) But, of late there is an increase in argument of initiating treatment with a combination therapy rather than stepwise addition of drugs, siting various benefits like reduced decline in glycemic control with any regimen, which is a matter of detailed evaluation and further research [11–14].
Sulfonylureas are one of the most potent and affordable anti-diabetic agents class with multiple advantages of its sleeve. Being one the oldest drug class with over 50 years of usage, it has a long history of safety and reliability with one of the highest potency for HBA1C reduction [4,15]. But on the other side, this drug group is associated with increased rate of myocardial infarction, all-cause mortality, hypoglycemia episodes, weight gain etc when compared with other standard treatment options [16–18].
In recent past, incretin based anti-diabetic drugs have come up as miracles for diabetes management that take help of incretin hormones like GLP-1 and its receptor, either directly through GLP-1 analogues or by reducing their metabolism by inhibiting the enzyme DPP-4.
Both these groups of drugs act by a novel mechanism of glucose dependent insulin secretion called as “The incretin effect” [19] DPP-4 inhibitors have some considerable advantages like lack of hypoglycemia, weight neutral and very well tolerated drugs, providing possible protection against prostate cancer, Alzheimer’s disease and even nephropathies [5,20–22]. But few recent increased incidences of pancreatitis, heart failures, DKA, Fournier’s gangrene, urticarial, arthralgia, bullous pemphigoid etc. have raised some questions on this relatively safe group of drugs [5,23]. On the other hand GLP-1 analogues have some unique advantages of cardio and renal protection, once weakly treatment option, weight reduction, blood pressure and cholesterol level management etc. along with the benefits of DPP- 4 inhibitors [5,24]. GLP-1 analogues have also been associated with some limitations like gastro intestinal side effects, increased heart rate, acute pancreatitis and very high cost [5].
Hence we have conducted this study to compare the therapeutic efficacy and long-term outcomes in patients treated with metformin and sulfonylureas alone alongside patients on a treatment regimen containing metformin, sulfonylureas and DPP-4 inhibitors. We have evaluated the parameters indicating glycemic control, complication and co-morbidity status along with ADR and effect on standard of living.
Aims and Objectives
The aim of this study is to provide evidence about the therapeutic efficacy and long term treatment outcomes in T2DM patients treated with DPP-4 inhibitors as an add-on therapy with metformin and sulfonylureas [25].
Methodology
Study design
The retrospective observational study was carried out on diagnosed T2DM patients with duration of the disease of 5 years & taking anti-diabetic treatment at GP clinics. Data was collected over a period of six months from January 2021 to june 2021 using a data extraction form/case record form.
Target population [26]
Patients who had received their treatment at GP clinics for one of the following OADs were included in the study
✓Sulfonylureas (e.g. glibenclamide, glimpiride);
✓ Biguanides (e.g. metformin),
✓ Thiazolidinediones (e.g. pioglitazone),
✓ Meglitinide analogues (e.g. repaglinide),
✓ Glucosidase inhibitor (e.g. acarbose),
✓ Oral dipeptidyl peptidase-4 inhibitor (e.g. sitagliptin)
✓SGLT2 inhibitors,
✓and combination therapy.
Among all the 153 patients included in our study 74 patients were selected and were divided into two groups as group-A and group-B. Patients taking Metformin & sulfonylureas combination were kept in Group-A and patients taking a combination of Metformin, sulfonylureas and DPP-4 inhibitors were kept in group-B. It was made assure that the same treatment protocol was followed for more than a year in all the patients with the help of their treatment files and prescriptions.
Inclusion criteria [27]
✓ Patients with age more than equal to 18 years and less than 79 years.
✓ Diagnosed cases of T2DM with 4-6 years of disease duration.
✓Patients having at-least two prescriptions for one of the above mentioned OADs in last one year.
✓ Patients taking either metformin and sulfonylureas combination or metformin, sulfonylureas and DPP-4 inhibitor combination were kept for the purpose of present study.
✓ Patients who have maintained investigation and treatment documents like prescriptions/laboratory reports/EMRs/self-monitoring data of BP, Blood sugar level etc in a recorded format of file or e-file for at-least last one year.
Exclusion criteria [27]
✓ Type-1 and all other form of diabetes.
✓ Pregnant women.
✓ Patients with pre-existing serious diabetic complications like CKD, diabetic foot with amputation etc.
✓ Patients aged less than 18 years and more than 79 years.
Sample size
Total 153 patients were included in our study with consideration of inclusion and exclusions criteria as mentioned above. Sample size was calculated with the help of data from previous similar studies & using the formula n=1.962 × p(1-p)/d2, where prevalence(p) = 9%, absolute error of precision(d) 5% & confidence interval of 95%. Due to lack of data regarding percentage of diabetic patients attending GP clinics, the prevalence of T2DM in India was used for sample size calculation which is around 9% [28,29].
Procedures [30]
Patient consent were taken before data extraction with the help of a consent form and the privacy and confidentiality were strictly maintained. A case record form was utilized to extract the data like The body weight (kg), systolic and diastolic blood pressure (mmHg), blood glucose levels (mg/dL), HbA1c (%), serum urea/ Creatinine along with treatment summary & incidences of adverse events from the data obtained over last consecutive outpatient visits (at-least two), patients selfmonitored & recorded blood glucose and blood pressure data etc. for last one year and were evaluated in different treatment groups.
Different demographic data like age, gender, weight, height, BMI, duration of disease, family history, socio-economic status, qualification, addiction history & history of adverse effects were measured and studied for having any impact on efficacy & safety outcomes of different treatment groups. Treatment outcome targets were set like HBA1C<7, FBS<126, PPBS<200, BP< 130/80 etc. and people below that target were considered controlled and above were uncontrolled [31,32]. Presence of various micro & macro vascular complications were recorded with the help of the documents kept by the patients & evaluation outcomes at GP clinics. Finally all the parameters were analyzed using statistical software.
Statistical analysis [30]
Descriptive statistics (frequency and percentages) was used to summarize the categorical variables and multinomial logistic regression was used to calculate the adjusted odds ratio, which was further utilized to evaluate the relative efficacy & safety profile of the people in different treatment groups along with establishing the impact of other factors like demography and comorbidities on treatment outcomes. Confidence interval was taken as 95% and P value less than 0.05 was considered as statistically significant.
Results
It was observed that majority of the patients were from urban background (86, 56.2%). Number of male patients were more (87, 56.9%) & majority of the people belonged to middle class from socio economic point of view (125, 81.7%). Most of the people were having a minimum qualification of 10+ (117, 76.5%). Around 65% of the patients had a positive family history of T2DM with majority having it in 1st degree relatives (81, 52.9. Most of the people had no addiction history (113, 73.9%) & no major adverse effects seen in majority of patients taking anti-diabetic medications (86, 56.2%). The most common observed adverse effects were gastrointestinal disturbances (52, 34.6%) and hypoglycemia (14, 9.2%) (Tables 1 and 2).
| Patient details | Frequency | Percentage (%) | |
|---|---|---|---|
| Place | Rural | 67 | 43.8 |
| Urban | 86 | 56.2 | |
| Gender | Female | 66 | 43.1 |
| Male | 87 | 56.9 | |
| Socio economic status | High | 9 | 5.9 |
| Middle | 125 | 81.7 | |
| Low | 19 | 12.4 | |
| qualification | Post matric | 117 | 76.5 |
| Under matric | 36 | 23.5 | |
| Family history of T2DM | No history | 53 | 34.6 |
| Yes second degree | 19 | 12.4 | |
| Yes first degree | 81 | 52.9 | |
| Addiction history | No | 113 | 73.9 |
| Yes | 40 | 26.1 | |
| ADR history | No | 86 | 56.2 |
| GI side effects | 53 | 34.6 | |
| Hypoglycemia | 14 | 9.2 | |
| Total | 153 | 100 | |
Table 1: Demographic data.
The mean age of the patients in our study was 57.31±8.38 yrs., where people from the age of 33 year to 72 years were enrolled. People with a duration of disease between 4-6 years were taken with a mean age of 5.16±0.81 years. Average weight of the study population was 68.84±7.15 kg and average height was 1.6±0.1 meters. The mean BMI of the patients was 26.93±3.62 kg/meter2 which ranged from 19.14 to 33.78 kg/meter2 (Table 2).
| Patient details | Minimum | Maximum | Mean | Std. Deviation |
|---|---|---|---|---|
| Age | 33 | 72 | 57.31 | 8.38 |
| Duration of disease | 4 | 6 | 5.16 | 0.81 |
| Body weight in KG | 49 | 81 | 68.84 | 7.15 |
| Height In meter | 1.4 | 1.8 | 1.6 | 0.1 |
| Body Mass Index | 19.14 | 33.78 | 26.93 | 3.62 |
Table 2: Demographic data.
Around (90 & 70, 58.8% & 45.8%) people of our study population were having fasting & post prandial hyperglycemia with blood sugar level more than 126 & 200 respectively. HBA1C level was more than 7mg% in around (69, 45.1%) people of different treatment group. Serum creatinine & blood pressure were also above control level in 10.5% & 54.9% of the population (Table 3).
| Mean values of lab data of last one year | Frequency | Percentage (%) | |
|---|---|---|---|
| FBS(mg/dl) | less than 126 | 63 | 41.2 |
| more than or equal to 126 | 90 | 58.8 | |
| PPBS(mg/dl) | less than 200 | 83 | 54.2 |
| more than or equal to 200 | 70 | 45.8 | |
| HBA1C (mg %) | less than 7 | 84 | 54.9 |
| more than or equal to 7 | 69 | 45.1 | |
| Serum creatinine | normal | 137 | 89.5 |
| above normal | 16 | 10.5 | |
| Blood Pressure | controlled | 69 | 45.1 |
| uncontrolled | 84 | 54.9 | |
| Total | 153 | 100 | |
Table 3: Biochemical parameters.
In our study, multiple co-morbidities were also recorded along with T2DM. Around 114(74.5%) people were having hypertension, 94(61.4%) were having dyslipidemia and 48(31.4%) people were overweight or obese. While hypertension had a negative impact on glycemic outcome (OR, 0.191; 95% CI, 0.79-0.464) for HBA1C being less than 7, obesity had an opposite effect (OR, 6.204; 95% CI, 2.539-15.164). Rest of the co-morbidities had no statistically significant impact on HBA1C level (Table 4).
| Comorbidities | Frequency | Percentage (%) | |
|---|---|---|---|
| Hypertension | yes | 114 | 74.5 |
| no | 39 | 25.5 | |
| Dyslipidemia | yes | 94 | 61.4 |
| no | 59 | 38.6 | |
| Obesity | yes | 48 | 31.4 |
| no | 105 | 68.6 | |
| Total | 153 | 100 | |
Table 4: Comorbidities.
Finally all the treatment groups were evaluated for relative glycemic control and other treatment outcomes. Patients treated with a combination of sulfonylureas/ metformin/DPP4 inhibitors (group-B) did show statistically significant better glycemic (OR, 2.862; 95% CI, 1.349-6.069) as compared to patients on a combination therapy of metformin & sulfonylureas (Group-A) (OR, 0.845; 95% CI, 0.299-2.385) (Table 5 and Figure 1). Among patients with hypertension as a comorbidity, the group-A have shown significantly lower BP control (OR, 0.114; 95% CI, 0.025-0.529) as compared to patients of Group-B where the association was not statistically significant (OR, 0.997; 95% CI, 0.487-2.043) (Table 6 and Figure 2). No statistically significant association was found between the diabetic complications and any of the treatment groups (Table 7 and Table 8).
| Treatment given | N | n(HBA1C<7) | Odds ratio | CI(95%) | P-value |
|---|---|---|---|---|---|
| Metformin+Sulfonylureas | 17 | 9 | 0.845 | 0.299-2.385 | 0.751 |
| Metformin+Sulfonylureas+DPP4I | 57 | 40 | 2.862 | 1.349-6.069 | 0.006 |
Table 5: Glycemic outcome.
| Treatment given | N | n | Odds ratio | CI (95%) | P-value |
|---|---|---|---|---|---|
| Metformin+Sulfonylureas | 17 | 2 | 0.114 | 0.025-0.529 | 0.006 |
| Metformin+Sulfonylureas+DPP4I | 57 | 28 | 0.997 | 0.487-2.043 | 0.994 |
Table 6: Blood pressure control.
| Treatment given | N | n(with neuropathy) | Odds ratio | P-value | CI(95%) |
|---|---|---|---|---|---|
| Metformin+Sulfonylureas | 17 | 8 | 0.412 | 0.101 | 0.143-1.188 |
| Metformin+Sulfonylureas+DPP4I | 57 | 36 | 1.154 | 0.723 | 0.524-2.541 |
Table 7: Patients developing neuropathy.
| Treatment given | N | n(with nephropathy) | Odds ratio | P-value | CI(95%) |
|---|---|---|---|---|---|
| Metformin+Sulfonylureas | 17 | 1 | 0.256 | 0.201 | 0.032-2.071 |
| Metformin+Sulfonylureas+DPP4I | 57 | 8 | 0.881 | 0.794 | 0.340-2.284 |
Table 8: Patients developing nephropathy.
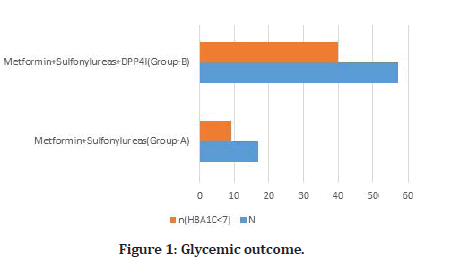
Figure 1: Glycemic outcome.
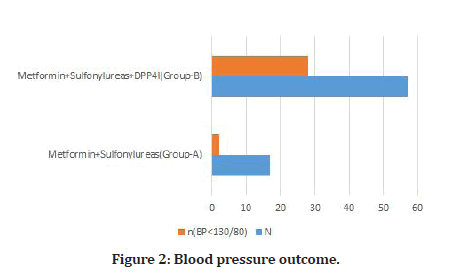
Figure 2:Blood pressure outcome.
Discussion
In our study, we found that most of the patients that attended a GP clinic belong to urban background. This might have been due to the location and the accessibility of a GP clinic catering to diabetic patients in an urban setup and a higher level of awareness about the disease in urban population [33]. More male patients were enrolled in the study than females indicate that women face multiple personal, sociocultural barriers in accessing healthcare services [34]. People from middle & low socio economic class were affected more by the disease as compared their high socio economic status counterparts. This might be due to the risk factors like genetic predisposition, poor diet quality, lack of physical activity, stress & smoking etc. [35]. Enrolment of more qualified people in the study possibly indicated more awareness about the disease and its complications in qualified people.
A higher proportion of diabetic patients having a positive family history strongly suggest it to be a very important risk factor for development of the disease [36]. Around 35% of the treated population reported minor ADRs like GI side effects while around 9% reported major side effects like hypoglycemia which has potentially high chance of hospitalization for management. Although producing multiple ADRs, the potential benefit of all the treatment protocols significantly out-weigh their risk. Incidence of ADRs may be attributed to multiple factors like polygenic variability, inter-ethnic variability, Clinical, anthropometric, and environmental factors such as age, sex, weight, concomitant use of other drugs etc. [37].
The average age of onset being between 55 to 60 years starting from as low as 33 years old people being affected by T2DM is a clear warning of the risk shifting towards younger population. This dangerous trend can be attributed to multiple factors such as increase in prevalence of obesity among youth [38]. People with disease duration between 4-6 years with a mean duration of 5.16±0.81 have been enrolled in the study to minimize multiple confounders and establish relative equilibrium in the study population. It’s an wellestablished fact that high BMI is a risk factors not only for development of pre-diabetes and diabetes but also for development of multiple complications of T2DM with increased tendency of hemoglobin to be glycated which is re-established in our study with average BMI of around 27(overweight) of the study population [39].
When different treatment groups were compared with each other, patients treated with a combination therapy of sulfonylureas/metformin/DPP4I(Group-B) did show a significantly better glycemic outcome as compared to Group-A. This finding is in line with the fact that DPP4 inhibitors can act synergistically with sulfonylureas and metformin to lower blood glucose level & even increases the risk of hypoglycemia [40,41]. Due to the recommendations of newer guidelines and proposed theory of initiation of treatment with combination therapy, physicians usually combine other drugs with first line drug to achieve target glycaemia far before reaching the higher recommended doses of metformin [5,11]. In our study population, the most common treatment and combination regimen was of sulfonylureas/metformin/DPP4I. Among the type 2 diabetic patients, hypertension is a major co-morbidity which not only causes similar complications but is also associated with worsening the pathophysiology due to synergistic adverse effects on large and small blood vessels leading to significantly higher cardiovascular mortality than either of these conditions alone [42,43]. Although both metformin & sulfonylureas are very good anti diabetic drugs, the newer agents like DPP-4 have proven their superiority in cardiovascular protection in multiple recent studies, which might explain the worst blood pressure control in Group-A when compared with Group-B [40,44]. When different groups were compared for development of chronic complications, no significant deference was found between the groups.
Conclusion
DPP-4 inhibitors are definitely highly efficacious drugs for the purpose of achieving good glycemic control, especially when given as an ad-on therapy. In our study we also found a relatively better Blood pressure control in Group-B as compared to group-A, which perhaps needs further research. We could not find any significant association of onset of complications with any of the treatment regimens. We feel that, there is an urgent need of a large number of similar studies to find out the relationship of different anti diabetic drugs with not only glycemic control but also long term complication and comorbidity outcomes along with impact on standard of living.
References
- Pearson ER. Type 2 diabetes: A multifaceted disease. Diabetologia 2019; 62:1107–1112.
- Landgraf R, Aberle J, Birkenfeld AL, et al. Therapy of type 2 diabetes. Exp Clin Endocrinol Diabetes 2019; 127:73–92.
- https://diabetesatlas.org/atlas/ninth-edition/
- Association AD. Pharmacologic approaches to glycemic treatment: Standards of medical care in diabetes-2020. Diabetes Care 2020; 43:98–110.
- Davies MJ, D’Alessio DA, Fradkin J, et al. Management of hyperglycemia in type 2 diabetes, 2018. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2018; 41:2669–2701.
- Holman RR, Paul SK, Bethel MA, et al. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med 2008; 359:1577–89.
- https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-revises-warnings-regarding-use-diabetes-medicine-metformin-certain
- Out M, Kooy A, Lehert P, et al. Long-term treatment with metformin in type 2 diabetes and methylmalonic acid: Post hoc analysis of a randomized controlled 4.3 year trial. J Diabet Complications 2018; 32:171-178.
- Hashem MM, Esmael A, Nassar AK, et al. The relationship between exacerbated diabetic peripheral neuropathy and metformin treatment in type 2 diabetes mellitus. Sci Rep 2021; 11:1940.
- https://www.diabetesincontrol.com/is-metformin-the-best-choice-for-type-2-diabetes-patients/
- Cahn A, Cefalu WT. Clinical considerations for use of initial combination therapy in Type 2 diabetes. Diabetes Care 2016; 39:S137–45.
- Cersosimo E, Johnson EL, Chovanes C, et al. Initiating therapy in patients newly diagnosed with type 2 diabetes: Combination therapy vs. a stepwise approach. Diabetes Obes Metab 2018; 20:497–507.
- Abdul-Ghani MA, Puckett C, Triplitt C, et al. Initial combination therapy with metformin, pioglitazone and exenatide is more effective than sequential add-on therapy in subjects with new-onset diabetes. Results from the Efficacy and Durability of Initial Combination Therapy for Type 2 Diabetes (EDICT): A randomized trial. Diabetes Obes Metab 2015; 17:268–275.
- Phung OJ, Sobieraj DM, Engel SS, et al. Early combination therapy for the treatment of type 2 diabetes mellitus: Systematic review and meta-analysis. Diabetes Obes Metab 2014; 16:410–417.
- Alzaid A. Sulfonylureas in the treatment of type 2 diabetes mellitus: A fresh look and new insights. Diabetes Ther 2020; 11:1–3.
- Lv W, Wang X, Xu Q, et al. Mechanisms and characteristics of sulfonylureas and glinides. Curr Top Med Chem 2020; 20:37–56.
- Zhou JB, Bai L, Wang Y, et al. The benefits and risks of DPP4-inhibitors vs. sulfonylureas for patients with type 2 diabetes: Accumulated evidence from randomised controlled trial. Int J Clin Pract 2016; 70:132–141.
- Douros A, Dell’Aniello S, Yu OHY, et al. Sulfonylureas as second line drugs in type 2 diabetes and the risk of cardiovascular and hypoglycaemic events: Population based cohort study. Br Med J 2018; 362:2693.
- Nauck MA, Meier JJ. The incretin effect in healthy individuals and those with type 2 diabetes: Physiology, pathophysiology, and response to therapeutic interventions. Lancet Diabetes Endocrinol 2016; 4:525–536.
- Chalichem NSS, Sai Kiran PSS, Basavan D. Possible role of DPP4 inhibitors to promote hippocampal neurogenesis in Alzheimer’s disease. J Drug Target 2018; 26:670–675.
- Shah C, Hong YR, Bishnoi R, et al. Impact of DPP4 Inhibitors in Survival of patients with prostate, pancreas, and breast cancer. Front Oncol 2020; 10:405.
- Nicotera R, Casarella A, Longhitano E, et al. Antiproteinuric effect of DPP-IV inhibitors in diabetic and non-diabetic kidney diseases. Pharmacol Res 2020; 159:105019.
- Deacon CF. Dipeptidyl peptidase 4 inhibitors in the treatment of type 2 diabetes mellitus. Nat Rev Endocrinol 2020; 16:642–653.
- Cornell S. A review of GLP-1 receptor agonists in type 2 diabetes: A focus on the mechanism of action of once-weekly agents. J Clin Pharm Ther 2020; 45:17–27.
- Liang HL, Ma SJ, Xiao YN, et al. Comparative efficacy and safety of oral antidiabetic drugs and insulin in treating gestational diabetes mellitus: An updated PRISMA-compliant network meta-analysis. Medicine 2017; 96.
- Balkhi B, Alwhaibi M, Alqahtani N, et al. Oral antidiabetic medication adherence and glycaemic control among patients with type 2 diabetes mellitus: A cross-sectional retrospective study in a tertiary hospital in Saudi Arabia. BMJ Open 2019; 9.
- Huang H, Bell KF, Gani R, et al. A retrospective real-world study of dapagliflozin versus other oral antidiabetic drugs added to metformin in patients with type 2 diabetes. Am J Managed Care 2018; 24:S132-137.
- Geldsetzer P, Manne-Goehler J, Theilmann M, et al. Diabetes and hypertension in India. JAMA Intern Med 2018; 178:363–372.
- Mitra A, Ray S. Evaluation of the safety and efficacy of teneligliptin at a higher dose in Indian type 2 diabetes patients: A retrospective analysis. Cureus 2020; 12.
- Nakanishi S, Iwamoto M, Kamei S, et al. Efficacy and Safety of switching from insulin glargine 100 u/ml to the same dose of glargine 300 u/ml in japanese type 1 and 2 diabetes patients: A retrospective analysis. Intern Med 2018; 57:1381–1389.
- https://www.idf.org/executive-office
- Park S. Ideal target blood pressure in hypertension. Korean Circ J 2019; 49:1002–1009.
- Hansen H, Pohontsch NJ, Bole L, et al. Regional variations of perceived problems in ambulatory care from the perspective of general practitioners and their patients - an exploratory focus group study in urban and rural regions of northern Germany. BMC Fam Pract 2017; 18:68.
- Suresh N, Thankappan KR. Gender differences and barriers women face in relation to accessing type 2 diabetes care: A systematic review. Indian J Public Health 2019; 63:65.
- Vinke PC, Navis G, Kromhout D, et al. Socio-economic disparities in the association of diet quality and type 2 diabetes incidence in the Dutch lifelines cohort. E Clin Med 2020; 19:100252.
- Anthanont P, Ramos P, Jensen MD, et al. Family history of type 2 diabetes, abdominal adipocyte size and markers of the metabolic syndrome. Int J Obes 2017; 41:1621–1626.
- Baye AM, Fanta TG, Siddiqui MK, et al. The genetics of adverse drug outcomes in type 2 diabetes: A systematic review. Front Genet 2021; 12:675053.
- Jensen ET, Dabelea D. Type 2 diabetes in youth: New lessons from the search study. Curr Diab Rep 2018; 18:36.
- Bala M, Meenakshi, Aggarwal S. Correlation of body mass index and waist/hip ratio with glycated hemoglobin in prediabetes. EJIFCC 2019; 30:317–324.
- Chaudhury A, Duvoor C, Reddy Dendi VS, et al. Clinical review of antidiabetic drugs: Implications for type 2 diabetes mellitus management. Front Endocrinol 2017; 8:6.
- Salvo F, Moore N, Arnaud M, et al. Addition of dipeptidyl peptidase-4 inhibitors to sulphonylureas and risk of hypoglycaemia: Systematic review and meta-analysis. Br Med J 2016; 353:i2231.
- Petrie JR, Guzik TJ, Touyz RM. Diabetes, hypertension, and cardiovascular disease: Clinical insights and vascular mechanisms. Can J Cardiol 2018; 34:575–584.
- Strain WD, Paldánius PM. Diabetes, cardiovascular disease and the microcirculation. Cardiovasc Diabetol 2018; 17:57.
- Davies MJ, D’Alessio DA, Fradkin J, et al. Management of Hyperglycemia in Type 2 Diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2018; 41:2669–2701.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Premakanta Mohanty1, Chinmaya Debasis Panda2 and Pradyut Kumar Pradhan3
1Department of medicine, FM medical College, Balasore, Odisha, India2Department of Pharmacology, MKCG Medical College, Brahmapur, Odisha, India
3Department of Pharmacology, FM Medical College, Balasore, Odisha, India
Citation: Premakanta Mohanty, Chinmaya Debasis Panda, Pradyut Kumar Pradhan, Therapeutic Efficacy & Long-term Treatment Outcome of DPP-4 Inhibitors as an add-on Therapy with Metformin and Sulfonylureas in T2DM Patients at GP Clinics of Southern Odisha, J Res Med Dent Sci, 2022, 10 (6):117-123.
Received: 06-Jun-2022, Manuscript No. JRMDS-22-65970; , Pre QC No. JRMDS-22-65970 (PQ); Editor assigned: 07-Jun-2022, Pre QC No. JRMDS-22-65970 (PQ); Reviewed: 21-Jun-2022, QC No. JRMDS-22-65970; Revised: 23-Jun-2022, Manuscript No. JRMDS-22-65970 (R); Published: 30-Jun-2022
